Abstract
Background
The COVID-19 pandemic has become a serious global public health problem. Although the use of angiotensin-converting enzyme inhibitors (ACEIs) and angiotensin II receptor type 1 blockers (ARBs) has been recommended in patients with COVID-19 and cardiovascular diseases (CVDs), according to the results of some small-sample retrospective analyses, there remains a lack of sufficient evidence to validate their efficacy. This multicenter retrospective study investigated whether ACEI/ARB administration was beneficial in patients with COVID-19 and CVDs.
Methods
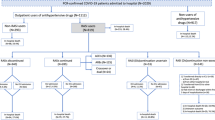
A total of 11,231 patients with confirmed COVID-19 and CVDs, from 138 hospitals in Hubei Province, were included in this multicenter retrospective study. We compared the clinical characteristics and outcomes between the ARB and non-ARB groups and analyzed the risk factors for in-hospital death using univariate and multivariate Cox regression analyses and Kaplan–Meier curves.
Results
In the multivariate Cox regression model, after adjusting for age, gender, comorbidities, and in-hospital medications, ARB use was associated with lower all-cause mortality (adjusted HR, 0.53; 95% CI, 0.38–0.73; P < 0.001). After propensity score-matched analysis, the adjusted HR for the use of ARB associated with all-cause mortality was 0.62 (95% CI, 0.40–0.88; P = 0.02). Further subgroup analyses found that the adjusted HRs for the use of ARB associated with all-cause mortality were 0.52 (95% CI, 0.30–0.89; P = 0.016), 0.37 (95% CI, 0.21–0.64; P < 0.001), 0.42 (95% CI, 0.28–0.64; P < 0.001), and 0.55 (95% CI, 0.37–0.84; P = 0.005) in patients with heart failure, diabetes, and hypercholesterolemia, and severe COVID-19, respectively.
Conclusions
ARB administration was significantly associated with a lower risk of all-cause mortality in patients with COVID-19 and CVDs.
Trial registration
ClinicalTrials.gov NCT05615792.




Similar content being viewed by others
Data Availability
The data underlying this article will be shared on reasonable request to the corresponding author.
Code Availability
The code underlying this article will be shared on reasonable request to the corresponding author.
References
Zheng Z, Peng F, Xu B, et al. Risk factors of critical & mortal COVID-19 cases: a systematic literature review and meta-analysis. J Infect. 2020;81(2):e16–25.
Li J, Huang DQ, Zou B, et al. Epidemiology of COVID-19: a systematic review and meta-analysis of clinical characteristics, risk factors, and outcomes. J Med Virol. 2021;93(3):1449–58.
Dale CE, Takhar R, Carragher R, et al. The impact of the COVID-19 pandemic on cardiovascular disease prevention and management. Nat Med. 2023;29(1):219–25.
Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):e13–e115.
Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA Guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145(18):e895–e1032.
Zhang P, Zhu L, Cai J, et al. Association of inpatient use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ Res. 2020;126(12):1671–81.
Cannata F, Chiarito M, Reimers B, et al. Continuation versus discontinuation of ACE inhibitors or angiotensin II receptor blockers in COVID-19: effects on blood pressure control and mortality. Eur Heart J Cardiovasc Pharmacother. 2020;6(6):412–4.
Semenzato L, Botton J, Drouin J, et al. Antihypertensive drugs and COVID-19 risk: a cohort study of 2 million hypertensive patients. Hypertension. 2021;77(3):833–42.
Hoffmann M, Kleine-Weber H, Schroeder S, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181(2):271–80.e8.
Gallo G, Calvez V, Savoia C. Hypertension and COVID-19: Current Evidence and Perspectives. High Blood Press Cardiovasc Prev. 2022;29(2):115–23.
Danser AHJ, Epstein M, Batlle D. Renin-angiotensin system blockers and the COVID-19 pandemic: at present there is no evidence to abandon renin-angiotensin system blockers. Hypertension. 2020;75(6):1382–5.
Borland JA, Kelsall C, Yacoub MH, Chester AH. Expression, localisation and function of ACE and chymase in normal and atherosclerotic human coronary arteries. Vascul Pharmacol. 2005;42(3):99–108.
Kaparianos A, Argyropoulou E. Local renin-angiotensin II systems, angiotensin-converting enzyme and its homologue ACE2: their potential role in the pathogenesis of chronic obstructive pulmonary diseases, pulmonary hypertension and acute respiratory distress syndrome. Curr Med Chem. 2011;18(23):3506–15.
Tan WSD, Liao W, Zhou S, Mei D, Wong WF. Targeting the renin-angiotensin system as novel therapeutic strategy for pulmonary diseases. Curr Opin Pharmacol. 2018;40:9–17.
Volpe M, Battistoni A, Bellotti P, et al. Recommendations for cardiovascular prevention during the Sars-Cov-2 pandemic: an executive document by the Board of the Italian Society of Cardiovascular Prevention. High Blood Press Cardiovasc Prev. 2020;27(5):373–7.
ESC guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic: part 2-care pathways, treatment, and follow-up. Eur Heart J. 2022;43(11):1059–103.
Grasselli G, Greco M, Zanella A, et al. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA Intern Med. 2020;180(10):1345–55.
Zhang Y, Luo W, Li Q, et al. Risk Factors for Death Among the First 80 543 Coronavirus Disease 2019 (COVID-19) Cases in China: relationships between age, underlying disease, case severity, and region. Clin Infect Dis. 2022;74(4):630–8.
Huang L, Li X, Gu X, et al. Health outcomes in people 2 years after surviving hospitalisation with COVID-19: a longitudinal cohort study. Lancet Respirat Med. 2022;10(9):863–76.
Zhang H, Li X, Huang L, et al. Lung-function trajectories in COVID-19 survivors after discharge: a two-year longitudinal cohort study. EClinicalMedicine. 2022;54:101668.
Son M, Seo J, Yang S. Association Between Renin-Angiotensin-Aldosterone System Inhibitors and COVID-19 Infection in South Korea. Hypertension. 2020;76(3):742–9.
Bavishi C, Whelton PK, Mancia G, Corrao G, Messerli FH. Renin-angiotensin-system inhibitors and all-cause mortality in patients with COVID-19: a systematic review and meta-analysis of observational studies. J Hypertens. 2021;39(4):784–94.
Mehta N, Kalra A, Nowacki AS, et al. Association of use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers with testing positive for coronavirus disease 2019 (COVID-19). JAMA Cardiol. 2020;5(9):1020–6.
Igase M, Kohara K, Nagai T, Miki T, Ferrario CM. Increased expression of angiotensin converting enzyme 2 in conjunction with reduction of neointima by angiotensin II type 1 receptor blockade. Hypertens Res. 2008;31(3):553–9.
Ni W, Yang X, Yang D, et al. Role of angiotensin-converting enzyme 2 (ACE2) in COVID-19. Crit Care. 2020;24(1):422.
Kundura L, Gimenez S, Cezar R, et al. Angiotensin II induces reactive oxygen species, DNA damage, and T-cell apoptosis in severe COVID-19. J Allergy Clin Immunol. 2022;150(3):594–603.e2.
Imai Y, Kuba K, Rao S, et al. Angiotensin-converting enzyme 2 protects from severe acute lung failure. Nature. 2005;436(7047):112–6.
Khalangot M, Sheichenko N, Gurianov V, Zakharchenko T, Kravchenko V, Tronko M. RAAS inhibitors are associated with a better chance of surviving of inpatients with Covid-19 without a diagnosis of diabetes mellitus, compared with similar patients who did not require antihypertensive therapy or were treated with other antihypertensives. Front Endocrinol. 2023;14:1077959. https://doi.org/10.3389/fendo.2023.1077959
de Abajo FJ, Rodríguez-Martín S, Lerma V, et al. Use of renin-angiotensin-aldosterone system inhibitors and risk of COVID-19 requiring admission to hospital: a case-population study. Lancet. 2020;395(10238):1705–14.
Zhao HJ, Li Y, Wang DY, Yuan HT. ARB might be superior to ACEI for treatment of hypertensive COVID-19 patients. J Cell Mol Med. 2021;25(23):11031–4.
Lopes RD, Macedo AVS, de Barros ESPGM, et al. Effect of discontinuing vs continuing angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers on days alive and out of the hospital in patients admitted with COVID-19: a randomized clinical trial. Jama. 2021;325(3):254–64.
Paguio JA, Casipit BA, John TA, Balu A, Lo KB. Angiotensin converting enzyme inhibitors and angiotensin II receptor blockers and outcomes in hospitalized patients with COVID-19: an updated systematic review and meta-analysis of randomized clinical trials. Expert Rev Cardiovasc Ther. 2023;21(3):219–26.
Liabeuf S, Moragny J, Bennis Y, et al. Association between renin-angiotensin system inhibitors and COVID-19 complications. Eur Heart J Cardiovasc Pharmacother. 2021;7(5):426–34.
Uehara G, Takeda H. Relative effects of telmisartan, candesartan and losartan on alleviating arterial stiffness in patients with hypertension complicated by diabetes mellitus: an evaluation using the cardio-ankle vascular index (CAVI). J Int Med Res. 2008;36(5):1094–102.
Nakajima T, Oh A, Saita S, et al. Comparative effectiveness of angiotensin II receptor blockers in patients with hypertension in Japan- systematic review and network meta-analysis. Circ Rep. 2020;2(10):576–86.
Acknowledgements
The authors would like to thank all the patients, their families, and all investigators involved in this study.
Funding
This study was supported in part by the National Natural Science Foundation of China (Nos. 82241034 and C-0052) and Top-Notch Talent Program of Hubei Province and Tongji Hospital (No. 2021YBJRC005).
Author information
Authors and Affiliations
Contributions
KX and WH designed the study, collected and analyzed data, performed the statistical analysis, and wrote the manuscript. BY, KZ, and DZ completed the data collation and was responsible for quality control. DWW designed the project, edited the manuscript, and supervised the study. All authors gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Corresponding author
Ethics declarations
Ethics Approval
This study was conducted in accordance with the principles of the Declaration of Helsinki and approved by the Research Ethics Committee of Tongji Medical College (no. TJ-IRB20210138).
Consent to Participate
Not applicable.
Consent for Publication
The authors declare that this manuscript is being submitted for consideration for publication.
Conflict of Interest
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 891 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xu, K., He, W., Yu, B. et al. Beneficial Effects of Angiotensin II Receptor Blockers on Mortality in Patients with COVID-19: A Retrospective Study from 2019 to 2020 in China. Cardiovasc Drugs Ther (2023). https://doi.org/10.1007/s10557-023-07494-5
Accepted:
Published:
DOI: https://doi.org/10.1007/s10557-023-07494-5