Abstract
Purpose
Both warfarin and non-vitamin K antagonist oral anticoagulants (NOACs) have pleiotropic effects including anti-inflammatory and anti-fibrotic properties. This study aims to explore whether arrhythmia recurrence after AF ablation is influenced by the choice of oral anticoagulant.
Methods
We retrospectively studied all patients who underwent primary AF ablation between 2011 and 2017 and divided them into two groups according to the anticoagulant used: Warfarin vs. NOACs. The primary endpoint was atrial tachyarrhythmia recurrence after ablation.
Results
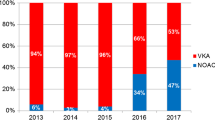
Of the 1106 patients who underwent AF ablation in the study period (median age 62.5 years; 71.5% males, 48.2% persistent AF), 697 (63%) received warfarin and 409 (37%) received NOACs. After a median of 26.4 months follow-up, arrhythmia recurrence was noted in 368 patients in warfarin group and 173 patients in NOACs group, with a 1-year recurrence probability of 35% vs. 36% (log rank P = 0.81) and 5-year recurrence probability of 62% vs. 63% (Log rank P = 0.32). However, NOACs use was associated with a higher probability of recurrence (46% for 1 year, 68% for 5 years) in patients with persistent AF compared with those taking warfarin (34% for 1 year, 63% for 5 years; log rank P = 0.01 and P = 0.02 respectively). Multivariate analysis indicated that in patients with persistent AF, use of NOACs was an independent risk factor of atrial tachyarrhythmia recurrence after ablation (HR 1.39, 95% CI 1.07–1.81, P = 0.013).
Conclusion
In this large contemporary cohort, overall AF recurrence after ablation was similar with NOACs or warfarin use. However, in patients with persistent AF, NOACs use was associated with a higher probability of arrhythmia recurrence and was an independent risk factor of recurrence at long-term follow-up.



Similar content being viewed by others
Data Availability
Data will be available upon reasonable request.
Abbreviations
- AF:
-
Atrial fibrillation
- AAD:
-
Antiarrhythmic drug
- CI:
-
Confidence interval
- HR:
-
Hazard ratio
- LA:
-
Left atrium
- NOACs:
-
Non-vitamin K antagonist oral anticoagulants
- OAC:
-
Oral anticoagulant
- PAR:
-
Protease-activated receptor
- TEE:
-
Transesophageal echocardiography
- VKA:
-
Vitamin K antagonist
References
Ziegler PD, Glotzer TV, Daoud EG, et al. Detection of previously undiagnosed atrial fibrillation in patients with stroke risk factors and usefulness of continuous monitoring in primary stroke prevention. Am J Cardiol. 2012;110:1309–14.
Miyasaka Y, Barnes ME, Gersh BJ, et al. Secular trends in incidence of atrial fibrillation in Olmsted County, Minnesota, 1980 to 2000, and implications on the projections for future prevalence. Circulation. 2006;114:119–25.
Krijthe BP, Kunst A, Benjamin EJ, et al. Projections on the number of individuals with atrial fibrillation in the European Union, from 2000 to 2060. Eur Heart J. 2013;34:2746–51.
Chugh SS, Havmoeller R, Narayanan K, et al. Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation. 2014;129:837–47.
Choudhury A, Lip GY. Atrial fibrillation and the hypercoagulable state: from basic science to clinical practice. Pathophysiol Haemost Thromb. 2003;33:282–9.
Kamel H, Okin PM, Elkind MS, Iadecola C. Atrial fibrillation and mechanisms of stroke: time for a new model. Stroke. 2016;47:895–900.
Connolly SJ, Ezekowitz MD, Yusuf S, et al. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009;361:1139–51.
Granger CB, Alexander JH, McMurray JJ, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011;365:981–92.
Patel MR, Mahaffey KW, Garg J, et al. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011;365:883–91.
Giugliano RP, Ruff CT, Braunwald E, et al. Edoxaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2013;369:2093–104.
Calkins H, Willems S, Gerstenfeld EP, et al. Uninterrupted dabigatran versus warfarin for ablation in atrial fibrillation. N Engl J Med. 2017;376:1627–36.
Cappato R, Marchlinski FE, Hohnloser SH, et al. Uninterrupted rivaroxaban vs. uninterrupted vitamin K antagonists for catheter ablation in non-valvular atrial fibrillation. Eur Heart J. 2015;36:1805–11.
January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64:e1-76.
January CT, Wann LS, Calkins H, et al. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2019;74:104–32.
Ting C, Fanikos C, Fatani N, Buckley LF, Fanikos J. Use of direct oral anticoagulants among patients with limited income and resources. J Am Coll Cardiol. 2019;73:526–8.
Spronk HM, De Jong AM, Verheule S, et al. Hypercoagulability causes atrial fibrosis and promotes atrial fibrillation. Eur Heart J. 2017;38:38–50.
Font J, Simeon M, Simard C, et al. PAR1 contribution in acute electrophysiological properties of oral anticoagulants in rabbit pulmonary vein sleeve preparations. Fundam Clin Pharmacol. 2018;32:378–91.
Gröber U, Reichrath J, Holick MF, Kisters K. Vitamin K: an old vitamin in a new perspective. Dermatoendocrinol. 2015;6:e968490.
Popov Aleksandrov A, Mirkov I, Ninkov M, et al. Effects of warfarin on biological processes other than haemostasis: a review. Food Chem Toxicol. 2018;113:19–32.
van Gorp RH, Schurgers LJ. New insights into the pros and cons of the clinical use of vitamin K antagonists (VKAs) versus direct oral anticoagulants (DOACs). Nutrients. 2015;7:9538–57.
American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Society of Echocardiography, American Heart Association, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Critical Care Medicine, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance, Douglas PS, Garcia MJ, Haines DE, Lai WW, Manning WJ, Patel AR, Picard MH, Polk DM, Ragosta M, Ward RP, Weiner RB. ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/SCCT/ SCMR 2011 Appropriate Use Criteria for Echocardiography. A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Society of Echocardiography, American Heart Association, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Critical Care Medicine, Society of Cardiovascular Computed Tomography, and Society for Cardiovascular Magnetic Resonance Endorsed by the American College of Chest Physicians. J Am Coll Cardiol. 2011;57:1126–66.
Wokhlu A, Monahan KH, Hodge DO, et al. Long-term quality of life after ablation of atrial fibrillation the impact of recurrence, symptom relief, and placebo effect. J Am Coll Cardiol. 2010;55:2308–16.
Wokhlu A, Hodge DO, Monahan KH, et al. Long-term outcome of atrial fibrillation ablation: impact and predictors of very late recurrence. J Cardiovasc Electrophysiol. 2010;21:1071–8.
Manfioletti G, Brancolini C, Avanzi G, Schneider C. The protein encoded by a growth arrest-specific gene (gas6) is a new member of the vitamin K-dependent proteins related to protein S, a negative coregulator in the blood coagulation cascade. Mol Cell Biol. 1993;13:4976–85.
Yanagita M, Arai H, Ishii K, et al. Gas6 regulates mesangial cell proliferation through AXL in experimental glomerulonephritis. Am J Pathol. 2001;158:1423–32.
Zimmerman SW, Moorthy AV, Dreher WH, Friedman A, Varanasi U. Prospective trial of warfarin and dipyridamole in patients with membranoproliferative glomerulonephritis. Am J Med. 1983;75:920–7.
Nagai K, Arai H, Yanagita M, et al. Growth arrest-specific gene 6 is involved in glomerular hypertrophy in the early stage of diabetic nephropathy. J Biol Chem. 2003;278:18229–34.
Kubo H, Nakayama K, Yanai M, et al. Anticoagulant therapy for idiopathic pulmonary fibrosis. Chest. 2005;128:1475–82.
Delbeck M, Nickel KF, Perzborn E, et al. A role for coagulation factor Xa in experimental pulmonary arterial hypertension. Cardiovasc Res. 2011;92:159–68.
Hanna N, Cardin S, Leung TK, Nattel S. Differences in atrial versus ventricular remodeling in dogs with ventricular tachypacing-induced congestive heart failure. Cardiovasc Res. 2004;63:236–44.
Eichbaum FW, Slemer O, Zyngier SB. Anti-inflammatory effect of warfarin and vitamin K. Naunyn Schmiedebergs Arch Pharmacol. 1979;307:185–90.
Maclean PS, Tait RC, Rumley A, McMahon AD, Lowe GD. Anticoagulation with warfarin downregulates inflammation. J Thromb Haemost. 2003;1:1838–9.
Berkarda B, Bouffard-Eyüboğlu H, Derman U. The effect of coumarin derivatives on the immunological system of man. Agents Actions. 1983;13:50–2.
Mirkov I, Popov Aleksandrov A, Demenesku J, et al. Intestinal toxicity of oral warfarin intake in rats. Food Chem Toxicol. 2016;94:11–8.
Popov A, Belij S, Subota V, et al. Oral warfarin affects peripheral blood leukocyte IL-6 and TNFα production in rats. J Immunotoxicol. 2013;10:17–24.
Spronk HM, de Jong AM, Crijns HJ, Schotten U, Van Gelder IC, Ten Cate H. Pleiotropic effects of factor Xa and thrombin: what to expect from novel anticoagulants. Cardiovasc Res. 2014;101:344–51.
Jumeau C, Rupin A, Chieng-Yane P, et al. Direct thrombin inhibitors prevent left atrial remodeling associated with heart failure in rats. JACC Basic Transl Sci. 2016;1:328–39.
Kondo H, Abe I, Fukui A, et al. Possible role of rivaroxaban in attenuating pressure-overload-induced atrial fibrosis and fibrillation. J Cardiol. 2018;71:310–9.
Nakase T, Moroi J, Ishikawa T. Anti-inflammatory and antiplatelet effects of non-vitamin K antagonist oral anticoagulants in acute phase of ischemic stroke patients. Clin Transl Med. 2018;7:2–7.
Kikuchi S, Tsukahara K, Sakamaki K, et al. Comparison of anti-inflammatory effects of rivaroxaban vs dabigatran in patients with non-valvular atrial fibrillation RIVAL-AF study: multicenter randomized study. Heart Vessels. 2019;34:1002–13.
Lau DH, Linz D, Schotten U, Mahajan R, Sanders P, Kalman JM. Pathophysiology of paroxysmal and persistent atrial Fibrillation: rotors, foci and fibrosis. Heart Lung Circ. 2017;26:887–93.
Funding
This work was partially supported by the National Natural Science Foundation of China (NSFC 81870243).
Author information
Authors and Affiliations
Contributions
KM, SB, and SNW were responsible for data acquisition. SNW was responsible for data interpretation and writing up of the paper. DH contributed to data acquisition and analysis. KM and CP helped with manuscript composition and proofreading. DP, SP, and SA contributed substantially to the conception and design of the study and helped with data interpretation, they also took overall responsibility for the study and final revision of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
This study was approved by the Mayo Clinic Institutional Review Board. All patients signed informed consent to use their medical data for research purpose.
Research Involving Human Participants and/or Animals
This article does not contain any studies with human participants or animals performed by any of the authors.
Consent for Publication
All authors read and approved the final manuscript.
Competing Interests
Dr. Packer reported receiving grants from the Abbott, Biosense Webster, Boston Scientific/EPT, CardioInsight, CardioFocus, Endosense, Hansen Medical, Medtronic, NIH, Robertson Foundation, St. Jude Medical, Siemens, and Thermedical; serving on the advisory board without compensation for Abbott, Biosense Webster, Inc., Boston Scientific, CardioFocus, Johnson & Johnson, Medtronic, St. Jude Medical, and Siemens, SigNum Preemptive Healthcare, Inc., Spectrum Dynamics, and Thermedical; speaking with an honorarium from Biotronik and MediaSphere Medical, LLC; receiving royalties from Wiley & Sons, Oxford, and St Jude Medical; Dr. Packer and Mayo Clinic jointly have equity in a privately held company, External Beam Ablation Medical Devices, outside the submitted work. Dr Packer has mapping technologies with royalties paid. Dr. Asirvatham has received honoraria for speaking from Boston Scientific, Biotronik, Medtronic, St. Jude Medical. He also has received Aegis-Consultant/Consulting fee. Other authors had no disclosures to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wen, S., Pislaru, C., Monahan, K.H. et al. Arrhythmia Recurrence After Atrial Fibrillation Ablation: Impact of Warfarin vs. Non-Vitamin K Antagonist Oral Anticoagulants. Cardiovasc Drugs Ther 36, 891–901 (2022). https://doi.org/10.1007/s10557-021-07200-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-021-07200-3