Abstract
Background
Statins are widely prescribed for the primary and secondary prevention of cardiovascular disease (CVD), but their effectiveness is dependent on the level of adherence and persistence.
Objectives
This study aimed to explore the patterns of switching, adherence and persistence among the Australian general population with newly dispensed statins.
Methods
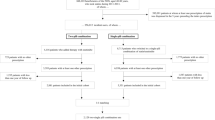
A retrospective cohort study was conducted using a random sample of data from the Australian national prescription claims data. Switching, adherence to and persistence with statins were assessed for people starting statins from 1 January 2015 to 31 December 2019. Switching was defined as either switching to another intensity of statin, to another statin or to a non-statin agent. Non-persistence to treatment was defined as discontinuation (i.e. ≥90 days with no statin) of coverage. Adherence was measured using proportion of days covered (PDC), and patients with PDC < 0.80 were considered non-adherent. Cox proportional hazard models were used to compare discontinuation, switching and reinitiation between different statins.
Results
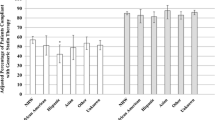
A cohort of 141,062 people dispensed statins and followed over a median duration of 2.5 years were included. Of the cohort, 29.3% switched statin intensity, 28.4% switched statin type, 3.7% switched to ezetimibe and in 2.7%, ezetimibe was added as combination therapy during the study period. Overall, 58.8% discontinued statins based on the 90-day gap criteria, of whom 55.2% restarted. The proportion of people non-adherent was 24.0% at 6 months to 49.0% at 5 years. People on low and moderate intensity statins were more likely to discontinue compared to those on high-intensity statins (hazard ratio [HR] 1.20, 95% confidence interval [CI] 1.09–1.31), (HR 1.28, 95%CI 1.14–1.42), respectively. Compared to maintaining same statin type and intensity, switching statins, which includes up-titration (HR 0.77, 95%CI 0.70 to 0.86) was associated with less likelihood of discontinuation after reinitiation.
Conclusions
Long-term persistence and adherence to statins remains generally poor among Australians, which limits the effectiveness of these medicines and the consequent health impact they may provide for individuals (and by extension, the population impact when poor persistence and adherence is considered in the statin-taking population). Switching between statins is prevalent in one third of statin users, although any clinical benefit of the observed switching trend is unknown. This, combined with the high volume of statin prescriptions, highlights the need for better strategies to address poor persistence and adherence.



Similar content being viewed by others
Abbreviations
- CVD:
-
Cardiovascular disease
- PBS:
-
Pharmaceutical Benefits Scheme
- LDL-C:
-
Low-density lipoprotein cholesterol
- PCSK9:
-
Proprotein convertase subtilisin/kexin type 9
- PDC:
-
Proportion of days covered
- GPs:
-
General practitioners
- PBAC:
-
Pharmaceutical Benefits Advisory Committee
References
World Health Organization. WHO cardiovascular diseases fact sheet providing key facts and information on risk factors, symptoms, rheumatic heart disease, treatment and prevention, WHO response. 2017. Available from: https://www.who.int/health-topics/cardiovascular-diseases/#tab=tab_1.
Roth GA, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159)1736–88.
Roth GA, Mensah GA, Johnson CO, Addolorato G, Ammirati E, Baddour LM, et al. Global burden of cardiovascular diseases and risk factors, 1990-2019: update from the GBD 2019 study. J Am Coll Cardiol. 2020;76(25):2982–3021.
AIHW. Cardiovascular disease. Canberra: Australian Institute of Health and Welfare, 2020. https://www.aihw.gov.au/reports/heart-stroke-vascular-diseases/cardiovascular-health-compendium/contents/how-many-australians-have-cardiovascular-disease.
Yusuf PS, Hawken S, Ôunpuu S, Dans T, Avezum A, Lanas F, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364(9438)937–52.
Abdullah SM, Defina LF, Leonard D, Barlow CE, Radford NB, Willis BL, et al. Long-term association of low-density lipoprotein cholesterol with cardiovascular mortality in individuals at low 10-year risk of atherosclerotic cardiovascular disease: results from the Cooper Center longitudinal study. Circulation. 2018;138(21):2315–25.
Clinician guide to the ABCs of primary and secondary prevention of atherosclerotic cardiovascular disease. American College of Cardiology. https://www.acc.org/latest-in-cardiology/articles/2018/03/30/18/34/clinician-guide-to-the-abcs.
Arnett DK, Roger Blumenthal C-CS, Michelle Albert C-CA, Buroker AB, Goldberger ZD, Hahn EJ, et al. Force on clinical practice guidelines. Circulation. 2019;140:563–95.
MacMahon S, Duffy S, Rodgers A, Tominaga S, Chambless L, De Backer G, et al. Blood cholesterol and vascular mortality by age, sex, and blood pressure: A meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. Lancet. 2007;370(9602):1829–39.
Newman CB, Preiss D, Tobert JA, Jacobson TA, Page RL, Goldstein LB, et al. Statin safety and associated adverse events a scientific statement from the American Heart Association. Arterioscler Thromb Vasc Biol. 2019;39(2):E38–81.
Rosenson RS, Baker S, Banach M, Borow KM, Braun LT, Bruckert E, et al. Optimizing cholesterol treatment in patients with muscle complaints. J Am Coll Cardiol. 2017;70(10):1290–301.
Mantel-Teeuwisse AK, Goettsch WG, Klungel OH, De Boer A, Herings RMC. Long term persistence with statin treatment in daily medical practice. Heart. 2004;90(9):1065–6.
Toth PP, Granowitz C, Hull M, Anderson A, Philip S. Long-term statin persistence is poor among high-risk patients with dyslipidemia: a real-world administrative claims analysis. Lipids Health Dis. 2019;18(1):175.
Wei MY, Ito MK, Cohen JD, Brinton EA, Jacobson TA. Predictors of statin adherence, switching, and discontinuation in the USAGE survey: understanding the use of statins in America and gaps in patient education. J Clin Lipidol. 2013;7(5):472–83.
Ho K, Jamsen KM, Bell JS, Korhonen MJ, Mc Namara KP, Magliano DJ, et al. Demographic, clinical and lifestyle factors associated with high-intensity statin therapy in Australia: the AusDiab study. Eur J Clin Pharmacol. 2018;74(11):1493–501.
Ofori-Asenso R, Ilomaki J, Tacey M, Zomer E, Curtis AJ, Si S, et al. Switching, discontinuation, and reinitiation of statins among older adults. J Am Coll Cardiol. 2018;72(21):2675–7.
Ofori-Asenso R, Ilomaki J, Tacey M, Zomer E, Curtis AJ, Bell JS, et al. Patterns of statin use and long-term adherence and persistence among older adults with diabetes. J Diabetes. 2018;10(9):699–707.
Mann DM, Woodward M, Muntner P, Falzon L, Kronish I. Predictors of nonadherence to statins: a systematic review and meta-analysis. Ann Pharmacother. 2010;44(9):1410–21.
Mellish L, Karanges EA, Litchfield MJ, Schaffer AL, Blanch B, Daniels BJ, et al. The Australian pharmaceutical benefits scheme data collection: a practical guide for researchers. BMC Res Notes. 2015;8:634.
Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. Circulation. 2014;129(25 Suppl 2):S1–45.
Cramer JA, Roy A, Burrell A, Fairchild CJ, Fuldeore MJ, Ollendorf DA, et al. Medication compliance and persistence: terminology and definitions. Value Health. 2008;11(1):44–7.
Ofori-Asenso R, Ilomaki J, Zomer E, Curtis AJ, Zoungas S, Liew D. A 10-year trend in statin use among older adults in Australia: an analysis using national pharmacy claims data. Cardiovasc Drugs Ther. 2018;32(3):265–72.
Simons LA, Ortiz M, Calcino G. Long term persistence with statin therapy -- experience in Australia 2006-2010. Aust Fam Physician. 2011;40(5):319–22.
Ofori-Asenso R, Zoungas S, Liew D. Reinitiation of statin therapy after discontinuation: a meta-analysis. Mayo Clin Proc. 2018;93(5):666–8.
Ofori-Asenso R, Jakhu A, Zomer E, Curtis AJ, Korhonen MJ, Nelson M, et al. Adherence and persistence among statin users aged 65 years and over: a systematic review and meta-analysis. J Gerontol A Biol Sci Med Sci. 2018;73(6):813–9.
Booth JN, Colantonio LD, Chen L, Rosenson RS, Monda KL, Safford MM, et al. Statin discontinuation, Reinitiation, and persistence patterns among Medicare beneficiaries after myocardial infarction. Circ Cardiovasc Quality Outcomes. 2017;10(10):e003626.
Vinogradova Y, Coupland C, Brindle P, Hippisley-Cox J. Discontinuation and restarting in patients on statin treatment: prospective open cohort study using a primary care database. BMJ. 2016;353:i3305.
Andrade SE, Walker AM, Gottlieb LK, Hollenberg NK, Testa MA, Saperia GM, et al. Discontinuation of antihyperlipidemic drugs--do rates reported in clinical trials reflect rates in primary care settings? N Engl J Med. 1995;332(17):1125–31.
Chodick G, Shalev V, Gerber Y, Heymann AD, Silber H, Simah V, et al. Long-term persistence with statin treatment in a not-for-profit health maintenance organization: a population-based retrospective cohort study in Israel. Clin Ther. 2008;30(11):2167–79.
Chew DP, Scott IA, Cullen L, French JK, Briffa TG, Tideman PA, et al. National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand: Australian clinical guidelines for the management of acute coronary syndromes 2016. Med J Aust. 2016;205(3):128–33.
Ridker PM, Mora S, Rose L, Group JTS. Percent reduction in LDL cholesterol following high-intensity statin therapy: potential implications for guidelines and for the prescription of emerging lipid-lowering agents. Eur Heart J. 2016;37(17):1373–9.
Qi K, Reeve E, Hilmer SN, Pearson SA, Matthews S, Gnjidic D. Older peoples’ attitudes regarding polypharmacy, statin use and willingness to have statins deprescribed in Australia. Int J Clin Pharm. 2015;37(5):949–57.
Schiattarella GG, Perrino C, Magliulo F, Ilardi F, Serino F, Trimarco V, et al. Statins and the elderly: recent evidence and current indications. Aging Clin Exp Res. 2012;24(3 Suppl):47–55.
Navarese EP, Robinson JG, Kowalewski M, Kołodziejczak M, Andreotti F, Bliden K, et al. Association between baseline LDL-C level and Total and cardiovascular mortality after LDL-C lowering: a systematic review and meta-analysis. JAMA. 2018;319(15):1566–79.
Ho PM, Spertus JA, Masoudi FA, Reid KJ, Peterson ED, Magid DJ, et al. Impact of medication therapy discontinuation on mortality after myocardial infarction. Arch Intern Med. 2006;166(17):1842–7.
Herttua K, Martikainen P, Batty GD, Kivimaki M. Poor adherence to statin and antihypertensive therapies as risk factors for fatal stroke. J Am Coll Cardiol. 2016;67(13):1507–15.
De Vera MA, Bhole V, Burns LC, Lacaille D. Impact of statin adherence on cardiovascular disease and mortality outcomes: a systematic review. Br J Clin Pharmacol. 2014;78(4):684–98.
Yan AT, Yan RT, Tan M, Hackam DG, Leblanc KL, Kertland H, et al. Contemporary management of dyslipidemia in high-risk patients: targets still not met. Am J Med. 2006;119(8):676–83.
Vonbank A, Saely CH, Rein P, Sturn D, Drexel H. Current cholesterol guidelines and clinical reality: a comparison of two cohorts of coronary artery disease patients. Swiss Med Wkly. 2013;143:w13828.
Vonbank A, Agewall S, Kjeldsen KP, Lewis BS, Torp-Pedersen C, Ceconi C, et al. Comprehensive efforts to increase adherence to statin therapy. Eur Heart J. 2017;38(32):2473–9.
Giugliano RP, Cannon CP, Blazing MA, Nicolau JC, Corbalan R, Spinar J, et al. Benefit of adding ezetimibe to statin therapy on cardiovascular outcomes and safety in patients with versus without diabetes mellitus: results from IMPROVE-IT (improved reduction of outcomes: Vytorin efficacy international trial). Circulation. 2018;137(15):1571–82.
Koskinas KC, Siontis GCM, Piccolo R, Mavridis D, Raber L, Mach F, et al. Effect of statins and non-statin LDL-lowering medications on cardiovascular outcomes in secondary prevention: a meta-analysis of randomized trials. Eur Heart J. 2018;39(14):1172–80.
Vavlukis M, Vavlukis A. Adding ezetimibe to statin therapy: latest evidence and clinical implications. Drugs Context. 2018;7:212534.
Yu M, Liang C, Kong Q, Wang Y, Li M. Efficacy of combination therapy with ezetimibe and statins versus a double dose of statin monotherapy in participants with hypercholesterolemia: a meta-analysis of literature. Lipids Health Dis. 2020;19(1):1.
Fung V, Graetz I, Reed M, Jaffe MG. Patient-reported adherence to statin therapy, barriers to adherence, and perceptions of cardiovascular risk. PLoS One. 2018;13(2):e0191817-e.
Fernandez-Lazaro CI, García-González JM, Adams DP, Fernandez-Lazaro D, Mielgo-Ayuso J, Caballero-Garcia A, et al. Adherence to treatment and related factors among patients with chronic conditions in primary care: a cross-sectional study. BMC Fam Pract. 2019;20(1):132.
Rafii F, Fatemi NS, Danielson E, Johansson CM, Modanloo M. Compliance to treatment in patients with chronic illness: a concept exploration. Iran J Nurs Midwifery Res. 2014;19(2):159–67.
Penson PE, Mancini GBJ, Toth PP, Martin SS, Watts GF, Sahebkar A, et al. Introducing the ‘Drucebo’ effect in statin therapy: a systematic review of studies comparing reported rates of statin-associated muscle symptoms, under blinded and open-label conditions. J Cachexia Sarcopenia Muscle. 2018;9(6):1023–33.
Nct. Self-Assessment Method for Statin Side-effects Or Nocebo. 2016. https://www.clinicaltrials.gov/ct2/show/NCT02668016.
Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2889–934.
Grabowski DC, Lakdawalla DN, Goldman DP, Eber M, Liu LZ, Abdelgawad T, et al. The large social value resulting from use of statins warrants steps to improve adherence and broaden treatment. Health Aff. 2012;31(10):2276–85.
Matthews A, Herrett E, Gasparrini A, Van Staa T, Goldacre B, Smeeth L, et al. Impact of statin related media coverage on use of statins: interrupted time series analysis with UK primary care data. BMJ. 2016;353:i3283.
Andrade AQ, Roughead EE. Consumer-directed technologies to improve medication management and safety. Med J Aust. 2019;210(Suppl 6):S24–S7.
Karatasakis A, Danek BA, Karacsonyi J, Rangan BV, Roesle MK, Knickelbine T, et al. Effect of PCSK9 inhibitors on clinical outcomes in patients with hypercholesterolemia: a meta-analysis of 35 randomized controlled trials. J Am Heart Assoc. 2017;6(12):e006910.
Krahenbuhl S, Pavik-Mezzour I, von Eckardstein A. Unmet needs in LDL-C lowering: when statins won’t do! Drugs. 2016;76(12):1175–90.
Marquina C, Zomer E, Vargas-Torres S, Zoungas S, Ofori-Asenso R, Liew D, et al. Novel treatment strategies for secondary prevention of cardiovascular disease: a systematic review of cost-effectiveness. Pharmacoeconomics. 2020;38(10):1095–113.
Nissen SE, Stroes E, Dent-Acosta RE, Rosenson RS, Lehman SJ, Sattar N, et al. Efficacy and tolerability of Evolocumab vs ezetimibe in patients with muscle-related statin intolerance: the GAUSS-3 randomized clinical trial. JAMA. 2016;315(15):1580–90.
Cardoso R, Blumenthal RS, Kopecky S, Lopez-Jimenez F, Martin SS. How low to go with lipid-lowering therapies in a cost-effective and prudent manner. Mayo Clin Proc. 2019;94(4):660–9.
Korman M, Wisløff T. Modelling the cost-effectiveness of PCSK9 inhibitors vs. ezetimibe through LDL-C reductions in a Norwegian setting. Eur Heart J Cardiovasc Pharmacother. 2018;4(1):15–22.
Ference BA, Yoo W, Alesh I, Mahajan N, Mirowska KK, Mewada A, et al. Effect of long-term exposure to lower low-density lipoprotein cholesterol beginning early in life on the risk of coronary heart disease: a Mendelian randomization analysis. J Am Coll Cardiol. 2012;60(25):2631–9.
Bhatt DL, Briggs AH, Reed SD, Annemans L, Szarek M, Bittner VA, et al. Cost-effectiveness of alirocumab in patients with acute coronary syndromes. The Odyssey Outcomes Trial. 2020;75(18):2297–308.
Cybulska B, Kłosiewicz-Latoszek L, Penson PE, Nabavi SM, Lavie CJ, Banach M. How much should LDL cholesterol be lowered in secondary prevention? Clinical efficacy and safety in the era of PCSK9 inhibitors. Prog Cardiovasc Dis. 2020;S0033-0620(20):30210-3.
Penson PE, Pirro M, Banach M. LDL-C: lower is better for longer—even at low risk. BMC Med. 2020;18(1):320.
Availability of Data and Material
Data are accessible or available upon request.
Funding
Amgen Australia Pty Ltd. has provided financial support to Monash University for analyses that describe the current burden and treatment of CVD in Australia, of which this manuscript forms a part.
Author information
Authors and Affiliations
Contributions
ST conceptualized the study, performed the analysis, validated and cross-checked analysis outputs with assistance from ROA and wrote the initial draft of the manuscript; CM, AJO, JI, MP, EZ and DL contributed to writing of the manuscript; JI, DT, SL provided constructive feedback and expert advice; ROA provided statistical support and expert feedback. ZA contributed to writing of the manuscript and supervised the project.
Corresponding author
Ethics declarations
ROA declares no conflict of interest. Authors ZA, EZ, ST, CM, MP, AO and DL have received research funding from Amgen Australia Pty Ltd. underlying this manuscript. JI has received funding from AstraZeneca, Amgen, Dementia Australia, National Breast Cancer Foundation and National Health and Medical Research Council. DT is employed by Amgen Australia Pty Ltd., and SL was employed by Amgen Australia Pty Ltd. at the time of development of the research and is now employed by Amgen Europe GmbH. EZ reports grant support from Amgen, AstraZeneca, Pfizer, and Shire, outside the submitted work. DL declares grants from Abbvie, Amgen, AstraZeneca, Bristol-Myers Squibb, Pfizer and Sanofi, and past participation in advisory boards and/or receipt of honoraria from Abbvie, Amgen, Astellas, AstraZeneca, Bristol-Myers Squibb, Edwards Lifesciences, Novartis, Pfizer, Sanofi and Shire, outside the submitted work.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Talic, S., Marquina, C., Ofori-Asenso, R. et al. Switching, Persistence and Adherence to Statin Therapy: a Retrospective Cohort Study Using the Australian National Pharmacy Data. Cardiovasc Drugs Ther 36, 867–877 (2022). https://doi.org/10.1007/s10557-021-07199-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-021-07199-7