Abstract
Objective
The study sought to assess the impact of treatment with beta-blocker (BB) or ACE inhibitor/angiotensin receptor blocker (ACEi/ARB) on secondary survival in patients presenting with ventricular tachyarrhythmia.
Background
Data regarding outcome of patients presenting with ventricular tachyarrhythmia treated with BB and ACEi/ARB is limited.
Methods
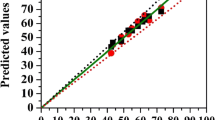
A large retrospective registry was used including consecutive patients presenting with ventricular tachycardia and fibrillation from 2002 to 2016 on admission. Applying propensity-score matching for harmonization, the impact of “BB” and “ACEi/ARB” was comparatively evaluated. The primary prognostic outcome was long-term all-cause death at 3 years.
Results
A total of 972 matched patients were included. Both patients with BB (long-term mortality rate 18 versus 27%; log rank p = 0.041; HR = 0.661; 95% CI = 0.443–0.986; p = 0.043) and with ACEi/ARB (long-term mortality rate 13 versus 23%; log rank p = 0.004; HR = 0.544; 95% CI = 0.359–0.824; p = 0.004) revealed better secondary survival compared to patients without after presenting with ventricular tachyarrhythmia on admission. The prognostic benefit of BB was comparable to ACEi/ARB (long-term mortality rate 21 versus 26%; log rank p = 0.539).
Conclusion
BB and ACEi/ARB were associated with improved secondary survival in patients surviving ventricular tachyarrhythmia on admission.
Trial Registration
ClinicalTrials.gov identifier: NCT02982473




Similar content being viewed by others
References
Priori, S.G., et al., 2015 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). European Heart Journal, 2015. 36(41): p. 2793–2867.
Refaat MM, Hotait M, London B. Genetics of sudden cardiac death. Curr Cardiol Rep. 2015;17(7):53.
Arshad A, Mandava A, Kamath G, Musat D. Sudden cardiac death and the role of medical therapy. Prog Cardiovasc Dis. 2008;50(6):420–38.
Katritsis DG, Gersh BJ, Camm AJ. A clinical perspective on sudden cardiac death. Arrhythmia Electrophysiol Rev. 2016;5(3):177–82.
Israel CW. Mechanisms of sudden cardiac death. Indian Heart J. 2014;66(Supplement 1):S10–7.
Erath JW, Hohnloser SH. Drugs to prevent sudden cardiac death. Int J Cardiol. 2017;237:22–4.
Turakhia M, Tseng ZH. Sudden cardiac death: epidemiology, mechanisms, and therapy. Curr Probl Cardiol. 2007;32(9):501–46.
Kamath GS, Mittal S. The role of antiarrhythmic drug therapy for the prevention of sudden cardiac death. Prog Cardiovasc Dis. 2008;50(6):439–48.
Landray MJ. Sudden death: ACE inhibitors and beta-blockers. Vol 95 Suppl 1. 2000. I37–40.
Cohen-Solal A, Jacobson AF, Piña IL. Beta blocker dose and markers of sympathetic activation in heart failure patients: interrelationships and prognostic significance. ESC Heart Failure. 2017;4:499–506.
Weeks PA, Sieg A, Gass JA, Rajapreyar I. The role of pharmacotherapy in the prevention of sudden cardiac death in patients with heart failure. Heart Fail Rev. 2016;21(4):415–31.
Boriani G, Diemberger I, Valzania C, Biffi M, Martignani C, Raschi E, et al. Role of drugs and devices in patients at risk of sudden cardiac death. Fundam Clin Pharmacol. 2010;24(5):575–94.
Latini R, Maggioni AP, Flather M, Sleight P, Tognoni G. ACE inhibitor use in patients with myocardial infarction. Circulation. 1995;92(10):3132–7.
Heart Outcomes Prevention Evaluation Study, I., et al. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. N Engl J Med. 2000;342(3):145–53.
Peck KY, Lim YZ, Hopper I, Krum H. Medical therapy versus implantable cardioverter-defibrillator in preventing sudden cardiac death in patients with left ventricular systolic dysfunction and heart failure: a meta-analysis of >35,000 patients. Int J Cardiol. 2014;173(2):197–203.
Goldberger JJ, Bonow RO, Cuffe M, Liu L, Rosenberg Y, Shah PK, et al. Effect of beta-blocker dose on survival after acute myocardial infarction. J Am Coll Cardiol. 2015;66(13):1431–41.
Investigators C-I. The cardiac insufficiency bisoprolol study II (CIBIS-II): a randomised trial. Lancet. 1999;353(9146):9–13.
Shekelle PG, Rich MW, Morton SC, Atkinson CSW, Tu W, Maglione M, et al. Efficacy of angiotensin-converting enzyme inhibitors and beta-blockers in the management of left ventricular systolic dysfunction according to race, gender, and diabetic status. J Am Coll Cardiol. 2003;41(9):1529–38.
Priori SG, et al. 2015 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J, 2015 36(41): p. 2793–867.
Ponikowski P, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J, 2016. 37(27): p. 2129–200.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivariate Behav Res. 2011;46(3):399–424.
Ferdinand D, Otto M, Weiss C. Get the most from your data: a propensity score model comparison on real-life data. Int J Gen Med. 2016;9:123–31.
Alberte C, Zipes DP. Use of nonantiarrhythmic drugs for prevention of sudden cardiac death. J Cardiovasc Electrophysiol. 2003;14(s9):S87–95.
Timolol-induced reduction in mortality and reinfarction in patients surviving acute myocardial infarction. N Engl J Med, 1981; 304(14): p. 801–7.
Olsson G, et al. Metoprolol-induced reduction in postinfarction mortality: pooled results from five double-blind randomized trials. Eur Heart J. 1992;13(1):28–32.
Friedman LM, Byington RP, Capone RJ, Furberg CD, Goldstein S, Lichstein E. Effect of propranolol in patients with myocardial infarction and ventricular arrhythmia. J Am Coll Cardiol. 1986;7(1):1–8.
Rutherford JD, Pfeffer MA, Moye LA, Davis BR, Flaker GC, Kowey PR, et al. Effects of captopril on ischemic events after myocardial infarction. Results of the survival and ventricular enlargement trial. SAVE Investigators. Circulation. 1994;90(4):1731–8.
Hall AS, Murray GD, Ball SG. Follow-up study of patients randomly allocated ramipril or placebo for heart failure after acute myocardial infarction: AIRE Extension (AIREX) Study. Lancet. 1997;349(9064):1493–7.
Torp-Pedersen C, Køber L. Effect of ACE inhibitor trandolapril on life expectancy of patients with reduced left-ventricular function after acute m yocardial infarction. Lancet. 1999;354(9172):9–12.
Ponikowski P, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. European Heart Journal, 2016; 37(27): p. 2129–2200.
Flather MD, Yusuf S, Køber L, Pfeffer M, Hall A, Murray G, et al. Long-term ACE-inhibitor therapy in patients with heart failure or left-ventricular dysfunction: a systematic overview of data from individual patients. Lancet. 2000;355(9215):1575–81.
Effect of metoprolol CR/XL in chronic heart failure: metoprolol CR/XL Randomised Intervention Trial in-Congestive Heart Failure (MERIT-HF). Lancet, 1999. 353(9169): p. 2001–2007.
Kochs M, Eggeling T, Hombach V. Pharmacological therapy in coronary heart disease: prevention of life-threatening ventricular tachyarrhythmias and sudden cardiac death. Eur Heart J. 1993;14(suppl_E):107–19.
Reiter MJ, Reiffel JA. Importance of beta blockade in the therapy of serious ventricular arrhythmias. Am J Card Imaging. 82(4):9I–19I.
Hallstrom AP, Cobb LA, Yu BH, Weaver WD, Fahrenbruch CE. An antiarrhythmic drug experience in 941 patients resuscitated from an initial cardiac arrest between 1970 and 1985. Am J Cardiol. 1991;68(10):1025–31.
Brodsky MA, Allen BJ, Bessen M, Luckett CR, Siddiqi R, Henry WL. Beta-blocker therapy in patients with ventricular tachyarrhythmias in the setting of left ventricular dysfunction. Am Heart J. 1988;115(4):799–808.
Brodsky MA, Allen BJ, Luckett CR, Capparelli EV, Wolff LJ, Henry WL. Antiarrhythmic efficacy of solitary beta-adrenergic blockade for patients with sustained ventricular tachyarrhythmias. Am Heart J. 1989;118(2):272–80.
AlJaroudi WA, et al. Effect of angiotensin-converting enzyme inhibitors and receptor blockers on appropriate implantable cardiac defibrillator shock in patients with severe systolic heart failure (from the GRADE Multicenter Study). Am J Cardiol. 2015;115(7):924–31.
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507–20.
Pfeffer MA, Braunwald E, Moyé LA, Basta L, Brown EJ Jr, Cuddy TE, et al. Effect of captopril on mortality and morbidity in patients with left ventricular dysfunction after myocardial infarction. Results of the survival and ventricular enlargement trial. The SAVE Investigators. N Engl J Med. 1992;327(10):669–77.
Swedberg K, Held P, Kjekshus J, Rasmussen K, Rydén L, Wedel H. Effects of the early administration of enalapril on mortality in patients with acute myocardial infarction. Results of the Cooperative New Scandinavian Enalapril Survival Study II (CONSENSUS II). N Engl J Med. 1992;327(10):678–84.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
There is no potential conflict of interests to disclose for any author. This study is based on a retrospective data analysis/registry and has been approved by the local ethics commission II of the faculty of Medicine Mannheim, University of Heidelberg, where no informed consent was deemed necessary for this study (ethical approval number 2016-612NMA) (ClinicalTrials.gov identifier: NCT02982473).
Conflict of Interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
ESM 1
(DOC 33 kb)
Rights and permissions
About this article
Cite this article
Schupp, T., Behnes, M., Weiß, C. et al. Beta-Blockers and ACE Inhibitors Are Associated with Improved Survival Secondary to Ventricular Tachyarrhythmia. Cardiovasc Drugs Ther 32, 353–363 (2018). https://doi.org/10.1007/s10557-018-6812-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-018-6812-z