Abstract
ᅟ
The interaction between the heart and the arterial system (ventricular-arterial coupling - VA) is an important determinant of cardiovascular performance. Vascular stiffness (Ea) and left ventricular (LV) endsystolic stiffness (Elv) augment with age and in heart failure (HF). Beta blockers (BB) are recommended therapy for patients with HF. However, data about the effects of BB on VA coupling are scarce.
Aims of the Study: To assess
1) changes in VA after BB therapy; 2) interactions between VA and LV functions, 3) predictive factors influencing VA change.
Methods
Eight hundred seventy-seven elderly patients with HF (aged ≥ 65, NYHA ≥ II, LV ejection fraction (LVEF) ≤ 45 %), treated with BB according to the CIBIS-ELD protocol of up-titration, underwent Doppler echocardiography with clinical and laboratory assessment before and after 12 weeks of BB. VA coupling was calculated as Ea/Elv ratio.
Results
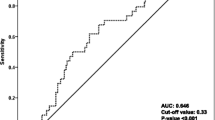
Ventriculo-arterial interaction improved after 12 weeks of BB in elderly patients with HF. Values of Ea significantly decreased from 2.73 ± 1.16 to 2.40 ± 1.01, p < 0.001, resulting in a VA level close to the optimal range i.e. from 1.70 ± 1.05 (1.46) to 1.50 ± 0.94 (1.29), p < 0.001. A similar degree of VA change was found in the patients with ischemic and non-ischemic HF after the treatment. Improvement in the clinical stage of HF closely correlated with VA coupling change after BB (p = 0.006). The strongest predictor of VA coupling alteration during BB was the improvement in global LVEF (p < 0.001) followed by the age of patients (p = 0.014).
Conclusions
The beneficial effect of BB in elderly patients with HF was achieved by optimizing VA coupling close to recommended range, associated with an improvement in LVEF and contractility.
Similar content being viewed by others
References
Grayburn PA, Appleton CP, DeMaria AN, Greenberg B, Lowes B, Oh J, et al. Echocardiographic predictors of morbidity and mortality in patients with advanced heart failure: the Beta-blocker Evaluation of Survival Trial (BEST). J Am Coll Cardiol. 2005;45:1064–71.
Her YA, Kim JYK, Choi EY, Kim SA, et al. Value of ventricular siffness index and ventriculoarterial interaction in patients with nonischemic dilated cardiomyopathy. Circ J. 2009;73:1683–90.
Ishihara H, Yokota M, Sobue T, Saito H. Relation between ventriculoarterial coupling and myocardial energetics in patients with idiopathic dilated cardiomyopathy. J Am Coll Cardiol. 1994;23:406–16.
Chen C, Fetics B, Nevo E, Rochitte CE, Chiou KR, Ding PA, et al. Nonivasive single beat determination of left ventricular elastance in humans. J Am Coll Cardiol. 2001;38:1028–34.
Chantler PD, Lakatta EG. Arterial-ventricular coupling with aging and disease. Front Physiol. 2012;3:90.
Guarracino F, Baldassari R, Pinsky MR. Ventriculo-arterial decoupling in actually altered hemodynamic states. Crit Care. 2013;17:213.
Burkhoff D, Mirsky I, Suga H. Assessment of systolic and diastolic ventricular properties via pressure-volume analysis: a guide for clinical, translational, and basic researchers. Am J Physiol Heart Circ Physiol. 2005;289:501–12.
Kelly RP, Ting CT, Yang TM, Liu CP, Maughan WL, Chang MS. Effective arterial elastance as index of arterial vascular load in humans. Circulation. 1992;86:513–21.
Sunagawa K, Maughan WL, Burkhoff D, Sagawa K. Left ventricular interaction with arterial load studied in isolated canine ventricle. Am J Physiol. 1983;245(5 Pt 1):H773–80.
Zhong L, Ghista DN, Ng EY, Lim ST. Passive and active ventricula elastances of the left ventricle. Biomed Eng Online. 2005;4–10
Iakovou I, Karpanou EA, Vyssoulis GP, Toutouzas PK, Cokkinos DV. Assessment of arterial ventricular coupling changes in patients under therapy with various antihypertensive agents by a non-invasive echocardiographic method. Int J Cardiol. 2004;96:355–60.
Sagawa BA, Kass DA. Ventriculo-vascular interaction in heart failure. Heart Fail Clin. 2008;4:23–36.
Kass DA. Age-related changes in venticular-arterial coupling: pathophysiologic implications. Heart Fail Rev. 2002;7:51–62.
Borlaug BA, Kass DA. Ventricular-vascular interaction in heart failure. Heart Fail Clin. 2008;4:23–36.
Borlaug BA, Kass DA. Ventricular-vascular interaction in heart failure. Cardiol Clin. 2011;29:447–59.
López-Sendón J, Swedberg K, McMurray J, Tamargo J, Maggioni AP, Dargie H, et al. Expert consensus document on beta-adrenergic receptor blockers. Eur Heart J. 2004;25:1341–6.
Düngen HD, Apostolović S, Inkrot S, Tahirović E, Krackhardt F, Pavlović M, et al. Bisoprolol vs. carvedilol in elderly patients with heart failure: rationale and design of the CIBIS-ELD trial. Clin Res Cardiol. 2008;97:578–86.
Gelbrich G, Edelmann F, Inkrot S, Lainscak M, Apostolovic S, Neskovic AN, et al. Is target dose the treatment target? Uptitrating beta-blockers for heart failure in the elderly. Int J Cardiol. 2012;23(155):160–6.
Morgenthaler NG, Struck J, Thomas B, Bergmann A. Immunoluminometric assay for the midregion of pro-atrial natriuretic peptide in human plasma. Clin Chem. 2004;50:234–6.
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification. Eur J Echocardiogr. 2006;7:79–108.
Bauer F, Jones M, Shiota T, Firstenberg MS, Qin JX, Tsujino H, et al. Left ventricular outflow tract mean systolic acceleration as a surrogate for the slope of the leftventricular end-systolic pressure-volume relationship. J Am Coll Cardiol. 2002;40:1320–7.
Oh JK, Seward JB, Tajik AJ. The echo manual. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 1999.
Rich MW. Heart failure in the 21st century: a cardiogeriatric syndrome. J Gerontol A Biol Sci Med Sci. 2001;56(2):M88–96.
Torjesen AA, Sigurðsson S, Westenberg JJ, Gotal JD, Bell V, Aspelund T, et al. Pulse pressure relation to aortic and left ventricular structure in the Age, gene/environment susceptibility (AGES)-Reykjavik study. Hypertension. 2014;64:756–61.
Prabhu SD. Altered left ventricular-arterial coupling precedes pump dysfunction in early heart failure. Heart Vessels. 2007;22:170–7.
Redfield MM, Jacobsen SJ, Borlaug BA, Rodeheffer RJ, Kass DA. Age- and gender-related ventricular-vascular stiffening: a community-based study. Circulation. 2005;112:2254–62.
Burkhoff D, Sagawa K. Ventricular efficiency predicted by an analytical model. Am J Physiol. 1986;250(6 Pt 2):R1021–7.
Ky B, French B, May Khan A, Plappert T, Wang A, Chirinos JA, et al. Ventricular-arterial coupling, remodeling, and prognosis in chronic heart failure. J Am Coll Cardiol. 2013;62:1165–72.
Lechar P, Escolano S, Golmerd JL. Prognostic value of bisoprolol induced hemodynamic effects in heart failure during the cardiac insufficiency bisoprolol study (CIBIS). Circulation. 1997;96:2197–205.
Laperche T, Logeart D, Cohen Solal A, Gourgon R. Potential interests of heart rate lowering drugs. Heart. 1999;81:336–41.
Dekleva M, Düngen HD, Gelbrich G, Incrot S, Suzic Lazic J, Pavlovic Kleut M, et al. Beta blockers therapy is associated with improved left ventricular systolic function and sustained exercise capacity in elderly patients with heart failure. CIBIS-ELD sub-study. Aging Clin Exp Res. 2012;24:675–81.
Hernandez AF, Hammill BG, O’Connor CM, Schulman KA, Curtis LH, Fonarow GC. Clinical effectiveness of beta-blockers in heart failure: findings from the OPTIMIZE-HF (Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure) Registry. J Am Coll Cardiol. 2009;53:184–92.
Aaron MF, Borlaug BA. Heart failure with preserved ejection fraction: pathophysiology and emerging therapies. From AM et al. Cardiovasc Therapeutics. 2011;29:6–21.
Flather MD, Shibata MC, Coats AJ, et al. Randomized trial to determine the effect of nebivolol on mortality and cardiovascular hospital admission in elderly patients with heart failure (SENIORS). Eur Heart J. 2005;26:215.
Van Veldhuisen DJ, Cohen-Solal A, Böhm M, et al. Beta-blockade with nebivolol in elderly heart failure patients with impaired and preserved left ventricular ejection fraction: Data From SENIORS (Study of Effects of Nebivolol Intervention on Outcomes and Rehospitalization in Seniors With Heart Failure). J Am Coll Cardiol. 2009;53:2150.
Sanders-van Wijk S, Muzzarelli S, Neuhaus M, Kiencke S, Maeder M, Estlinbaum W, et al. Safety and tolerability of intensified, N-terminal pro brain natriuretic peptide-guided compared with standard medical therapy in elderly patients with congestive heart failure: results from TIME-CHF. Eur J Heart Fail. 2013;15:910–8.
Williams B, Lacy PS, Thom SM, Cruickshank K, Stanton A, Collier D, et al. Differential impact of blood pressure-lowering drugs on central aortic pressure and clinical outcomes: principal results of the Conduit Artery Function Evaluation (CAFE) study. Circulation. 2006;113(9):1213–25.
Koumaras C, Tziomalos K, Stavrinou E, Katsiki N, Athyros VG, Mikhailidis DP, et al. Effects of renin-angiotensin-aldosterone system inhibitors and beta-blockers on markers of arterial stiffness. J Am Soc Hypertens. 2014;8:74–82.
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dekleva, M., Lazic, J.S., Soldatovic, I. et al. Improvement of Ventricular-Arterial Coupling in Elderly Patients with Heart Failure After Beta Blocker Therapy: Results from the CIBIS-ELD Trial. Cardiovasc Drugs Ther 29, 287–294 (2015). https://doi.org/10.1007/s10557-015-6590-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-015-6590-9