Abstract
Background
Extensively used lipid-lowering statins have also non-lipid-lowering, pleiotropic effects. Previous studies have demonstrated that a pre-procedural single dose of atorvastatin is associated with reduced peri-procedural myocardial injury.
Aim
The aim of the present study was to demonstrate the effect of a single high loading dose (40 mg) of rosuvastatin on peri-procedural myocardial injury.
Methods
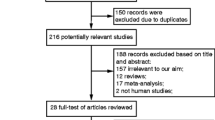
Two hundred ninety nine statin-naive patients with stable angina and de novo lesions eligible for PCI were randomized to a rosuvastatin-treatment (n = 153) and to a no-treatment (n = 146) group. A 40 mg loading dose of rosuvastatin was administrated 24 h before the PCI. CK-MB and cTnI levels were measured before and 12 h after the procedure.
Results
Baseline characteristics were fairly similar between the two arms. The incidence of a CK-MB and cTnI elevation >3× ULN in the rosuvastatin group was significantly lower compared to the control group (0.7% vs. 11.0%, p < 0.001 and 10.5% vs. 39.0%, p < 0.001, respectively). Similarly, the incidence of any CK-MB and cTnI elevation > ULN in the rosuvastatin group was significantly lower compared to the control group (10.5% vs. 34.2%, p < 0.001 and 20.9% vs. 61.6%, p < 0.001, respectively). In addition, CK-MB and cTnI values 12 h after the PCI were significantly lower in the rosuvastatin group compared to the control group (20.13 ± 7.24 U/L vs. 27.02 ± 18.64 U/L, p < 0.001 and 0.14 ± 0.34 ng/ml vs. 0.35 ± 0.40 ng/ml, p < 0.001, respectively).
Conclusion
A single high loading dose of rosuvastatin reduces the incidence of peri-procedural myocardial necrosis and infarction effectively.


Similar content being viewed by others
References
Thygesen K, Alpert JS, White HD. Joint ESC/ACCF/AHA/WHF Task Force for the Redefinition of Myocardial Infarction. Universal definition of myocardial infarction. J Am Coll Cardiol. 2007;50:2173–95.
Wu AH, Boden WE, McKay RG. Long-term follow-up of patients with increased cardiac troponin concentrations following percutaneous coronary intervention. Am J Cardiol. 2002;89:1300–2.
Ricciardi MJ, Davidson CJ, Gubernikoff G, et al. Troponin I elevation and cardiac events after percutaneous coronary intervention. Am Heart J. 2003;145:522–8.
Tardiff BE, Califf RM, Tcheng JE, et al. Clinical outcomes after detection of elevated cardiac enzymes in patients undergoing percutaneous intervention. IMPACT-II Investigators. Integrilin (eptifibatide) to Minimize Platelet Aggregation and Coronary Thrombosis-II. J Am Coll Cardiol. 1999;33:88–96.
Kong TQ, Davidson CJ, Meyers SN, et al. Prognostic implication of creatine kinase elevation following elective coronary artery interventions. JAMA. 1997;277:461–6.
Abdelmeguid AE, Topol EJ, Whitlow PL, et al. Significance of mild transient release of creatine kinase-MB fraction after percutaneous coronary interventions. Circulation. 1996;94:1528–36.
Abdelmeguid AE, Ellis SG, Sapp SK, et al. Defining the appropriate threshold of creatine kinase elevation after percutaneous coronary interventions. Am Heart J. 1996;131:1097–105.
Davignon J. Beneficial cardiovascular pleiotropic effects of statins. Circulation. 2004;109:III39–43.
Pasceri V, Patti G, Nusca A. et al; ARMYDA Investigators. Randomized trial of atorvastatin for reduction of myocardial damage during coronary intervention: results from the ARMYDA (Atorvastatin for Reduction of MYocardial Damage during Angioplasty) study. Circulation. 2004;110:674–8.
Patti G, Pasceri V, Colonna G, et al. Atorvastatin pretreatment improves outcomes in patients with acute coronary syndromes undergoing early percutaneous coronary intervention: results of the ARMYDA ACS randomized trial. J Am Coll Cardiol. 2007;49:1272–8.
Di Sciascio G, Patti G, Pasceri V, et al. Efficacy of atorvastatin reload in patients on chronic statin therapy undergoing percutaneous coronary intervention: results of the ARMYDA-RECAPTURE (Atorvastatin for Reduction of Myocardial Damage During Angioplasty) Randomized Trial. J Am Coll Cardiol. 2009;54:558–65.
Briguori C, Visconti G, Focaccio A, et al. Novel Approaches for Preventing or Limiting Events (Naples) II Trial Impact of a Single High Loading Dose of Atorvastatin on Periprocedural Myocardial Infarction. J Am Coll Cardiol. 2009 Aug 3.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502.
Bell RM, Yellon DM. Atorvastatin, administrated at the onset of reperfusion, and independent of lipid lowering, protects the myocardium by up-regulating a pro-survival pathway. J Am Coll Cardiol. 2003;41:508–15.
Mannacio VA, Iorio D, De Amicis V, Di Lello F, Musumeci F. Effect of rosuvastatin pretreatment on myocardial damage after coronary surgery: a randomized trial. J Thorac Cardiovasc Surg. 2008;136:1541–8.
Bellosta S. Direct vascular effects of HMG-CoA reductase inhibitors. Atherosclerosis. 1998;137:S101–9.
Essig M. 3-Hydroxy-3-methylglutaryl coenzyme A reductase inhibitors increase fibrinolytic activity in rat aortic endothelial cells. Role of geranylgeranylation and Rho proteins. Circ Res. 1998;83:683–90.
Colli S. Vastatins inhibit tissue factor in cultured human macrophages. A novel mechanism of protection against atherothrombosis. Arterioscler Thromb Vasc Biol. 1997;17:265–72.
Stalker T, Lefer A, Scalia R. A new HMG-CoA reductase inhibitor, rosuvastatin, exerts anti inflammatory effects on the microvascular endothelium: the role of mevalonic acid. Br J Pharmacol. 2001;133:406–12.
Laheta V, Goicoechea M, Garcia de Vinuesa S, et al. Endothelial dysfunction, oxidative stress and inflammation in atherosclerosis: beneficial effects of statins. Curr Med Chem. 2007;14:243–8.
Laufs U, La Fata V, Plutzky J, et al. Upregulation of endothelial nitric oxide synthase by HMG CoA reductase inhibitors. Circulation. 1998;97:1129–35.
Undas A, Brummel KE, Musial J, et al. Simvastatin depresses blood clotting by inhibiting activation of prpthrombin, factor V, and factor XIII and by enhancing factor Va inactivation. Circulation. 2001;103:2248–53.
Meijer P, Oyen WJ, Dekker D, et al. Rosuvastatin increases extracellular adenosine formation in humans in vivo: a new perspective on cardiovascular protection. Arterioscler Thromb Vasc Biol. 2009;29:963–8.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cay, S., Cagirci, G., Sen, N. et al. Prevention of Peri-procedural Myocardial Injury Using a Single High Loading Dose of Rosuvastatin. Cardiovasc Drugs Ther 24, 41–47 (2010). https://doi.org/10.1007/s10557-010-6224-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-010-6224-1