Abstract
Objective
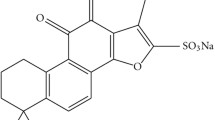
C-reactive protein (CRP) is considered a risk factor for coronary artery disease. In addition to its lipid-lowering properties, statin decreases the level of CRP. Abrupt cessation of statin therapy during treatment could increase CRP level independently of the elevation of serum lipids and the incidence of cardiac events in patients with atherosclerotic heart disease. Xuezhikang (XZK), an extract of cholestin, has a marked modulating effect on lipid and CRP concentrations in different study time course. However, no attention has been paid to the changes of lipid profile and CRP concentrations after withdrawal of XZK treatment. This study was designed to explore short-term time course effects on lipid profile and CRP concentrations after withdrawal of XZK treatment in coronary heart disease patients.
Materials and methods
Seventy-five consecutive patients with documented coronary heart disease were randomly divided into three groups: 1. Pretreatment with XZK 1,200 mg daily for 6 weeks and then replaced by placebo (XZK discontinued group; n = 25); 2. Treatment with XZK 1,200 mg daily throughout the study (XZK continued group; n = 25); or 3. Placebo (no XZK group; n = 25). Lipid levels (total cholesterol, HDL-C, LDL-C and triglycerides) and CRP were assessed before receiving the XZK therapy, 1 day before discontinuation of XZK, and on days 1, 2, 3, 7 and 14 after discontinuation of XZK, respectively.
Results
After 6-week XZK treatment, the fasting total cholesterol, LDL-C, triglyceride and median hs-CRP concentrations decreased, whereas HDL-C concentration increased significantly (p < 0.001, respectively). At day 14 after discontinuation of XZK therapy, total cholesterol (15%), LDL-C (17%) and triglyceride (20%) significantly increased (p < 0.001, respectively), whereas HDL-C level (15%) significantly decreased (p < 0.05). The median level of CRP increased by 11, 65, 128, 103 and 101% on the first, second, third, seventh, and fourteenth day after withdrawal of XZK therapy (p > 0.05, <0.05, <0.001, <0.001, <0.001, compared with 1 day before withdrawal of XZK therapy, respectively). There was a prominent rebound of CRP concentration 3 days after discontinuation of XZK therapy. At this time point, hs-CRP concentration was higher than in the placebo group (p < 0.05). Seven to 14 days after discontinuation of XZK therapy, the hs-CRP concentration declined to a similar level as in the placebo group. No significant correlation was seen between the changes in hs-CRP and lipid profile at all time points.
Conclusions
The level of hs-CRP increases on the second day after withdrawal of XZK and there is a prominent rebound 3 days after discontinuation of XZK therapy. The increase of CRP ends within 7 days, where lipids increase at 14 days after discontinuation of XZK therapy. The results may be clinically important for patients with coronary artery disease.
Similar content being viewed by others
References
Pedersen TR, Kjekshus J, Berg K, Haghfelt T, Faergeman O, Faergeman G, Pyorala K, Miettinen T, Wilhelmsen L, Olsson AG, Wedel H. Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). 1994. Atheroscler Suppl 2004;5:81–7.
The Long-Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. N Engl J Med 1998;339:1349–57.
Sacks FM, Pfeffer MA, Moye LA, Rouleau JL, Rutherford JD, Cole TG, Brown L, Warnica JW, Arnold JM, Wun CC, Davis BR, Braunwald E. The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N Engl J Med 1996;335:1001–9.
Rosenson RS, Tangney CC. Antiatherothrombotic properties of statins: implications for cardiovascular event reduction. JAMA 1998;279:1643–50.
Lee KT, Lai WT, Chu CS, Tsai LY, Yen HW, Voon WC, Sheu SH. Effect of withdrawal of statin on C-reactive protein. Cardiology 2004;102:166–70.
Retterstol L, Eikvar L, Bohn M, Bakken A, Erikssen J, Berg K. C-reactive protein predicts death in patients with previous premature myocardial infarction—a 10 year follow-up study. Atherosclerosis 2002;160:433–40.
Ridker PM, Rifai N, Clearfield M, Downs JR, Weis SE, Miles JS, Gotto AM Jr. Measurement of C-reactive protein for the targeting of statin therapy in the primary prevention of acute coronary events. N Engl J Med 2001;344:1959–65.
Lai WT, Lee KT, Chu CS, Voon WC, Yen HW, Tsai LY, Sheu SH. Influence of withdrawal of statin treatment on proinflammatory response and fibrinolytic activity in humans: an effect independent on cholesterol elevation. Int J Cardiol 2005;98:459–64.
Spencer FA, Allegrone J, Goldberg RJ, Gore JM, Fox KA, Granger CB, Mehta RH, Brieger D. Association of statin therapy with outcomes of acute coronary syndromes: the GRACE study. Ann Intern Med 2004;140:857–66.
Davignon J. Beneficial cardiovascular pleiotropic effects of statins. Circulation 2004;109(Suppl 1):III39–43.
Zhao SP, Liu L, Cheng YC, Shishehbor MH, Liu MH, Peng DQ, Li YL. Xuezhikang, an extract of cholestin, protects endothelial function through anti-inflammatory and lipid-lowering mechanisms in patients with coronary heart disease. Circulation 2004;110:915–20.
Jian J, Hao X, Deng C, Zhou H, Lin J. [The effects of xuezhikang on serum lipid profile, thromboxane A2 and prostacyclin in patients with hyperlipidemia]. Zhonghua Nei Ke Za Zhi 1999;38:517–9.
Heber D, Yip I, Ashley JM, Elashoff DA, Elashoff RM, Go VL. Cholesterol-lowering effects of a proprietary Chinese red-yeast-rice dietary supplement. Am J Clin Nutr 1999;69:231–6.
Zhao SP, Liu L, Cheng YC, Li YL. Effect of xuezhikang, a cholestin extract, on reflecting postprandial triglyceridemia after a high-fat meal in patients with coronary heart disease. Atherosclerosis 2003;168:375–80.
Liu L, Zhao SP, Cheng YC, Li YL. Xuezhikang decreases serum lipoprotein(a) and C-reactive protein concentrations in patients with coronary heart disease. Clin Chem 2003;49:1347–52.
Li JJ, Hu SS, Fang CH, Hui RT, Miao LF, Yang YJ, Gao RL. Effects of xuezhikang, an extract of cholestin, on lipid profile and C-reactive protein: a short-term time course study in patients with stable angina. Clin Chim Acta 2005;352:217–24.
Lu ZL. [China coronary secondary prevention study (CCSPS)]. Zhonghua Xin Xue Guan Bing Za Zhi 2005;33:109–15.
Ridker PM, Rifai N, Pfeffer MA, Sacks FM, Moye LA, Goldman S, Flaker GC, Braunwald E. Inflammation, pravastatin, and the risk of coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events (CARE) Investigators. Circulation 1998;98:839–44.
Lindahl B, Toss H, Siegbahn A, Venge P, Wallentin L. Markers of myocardial damage and inflammation in relation to long-term mortality in unstable coronary artery disease. FRISC Study Group. Fragmin during Instability in Coronary Artery Disease. N Engl J Med 2000;343:1139–47.
Heeschen C, Hamm CW, Laufs U, Snapinn S, Bohm M, White HD. Withdrawal of statins increases event rates in patients with acute coronary syndromes. Circulation 2002;105:1446–52.
Laufs U, Endres M, Custodis F, Gertz K, Nickenig G, Liao JK, Bohm M. Suppression of endothelial nitric oxide production after withdrawal of statin treatment is mediated by negative feedback regulation of rho GTPase gene transcription. Circulation 2000;102:3104–10.
Venugopal SK, Devaraj S, Yuhanna I, Shaul P, Jialal I. Demonstration that C-reactive protein decreases eNOS expression and bioactivity in human aortic endothelial cells. Circulation 2002;106:1439–41.
Verma S, Li SH, Badiwala MV, Weisel RD, Fedak PW, Li RK, Dhillon B, Mickle DA. Endothelin antagonism and interleukin-6 inhibition attenuate the proatherogenic effects of C-reactive protein. Circulation 2002;105:1890–6.
Fichtlscherer S, Rosenberger G, Walter DH, Breuer S, Dimmeler S, Zeiher AM. Elevated C-reactive protein levels and impaired endothelial vasoreactivity in patients with coronary artery disease. Circulation 2000;102:1000–6.
McGowan MP. There is no evidence for an increase in acute coronary syndromes after short-term abrupt discontinuation of statins in stable cardiac patients. Circulation 2004;110:2333–5.
Li JJ, Jiang H, Huang CX, Fang CH, Tang QZ, Xia H, Liu J, Li GS. Elevated level of plasma C-reactive protein in patients with unstable angina: its relations with coronary stenosis and lipid profile. Angiology 2002;53:265–72.
Speidl WS, Graf S, Hornykewycz S, Nikfardjam M, Niessner A, Zorn G, Wojta J, Huber K. High-sensitivity C-reactive protein in the prediction of coronary events in patients with premature coronary artery disease. Am Heart J 2002;144:449–55.
Abdelmouttaleb I, Danchin N, Ilardo C, Aimone-Gastin I, Angioi M, Lozniewski A, Loubinoux J, Le Faou A, Gueant JL. C-Reactive protein and coronary artery disease: additional evidence of the implication of an inflammatory process in acute coronary syndromes. Am Heart J 1999;137:346–51.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hu, CL., Li, YB., Tang, YH. et al. Effects of Withdrawal of Xuezhikang, an Extract of Cholestin, on Lipid Profile and C-reactive Protein: A Short-Term Time Course Study in Patients with Coronary Artery Disease. Cardiovasc Drugs Ther 20, 185–191 (2006). https://doi.org/10.1007/s10557-006-7947-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10557-006-7947-x