Summary
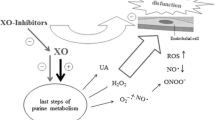
The plasma level of the uric acid is frequently elevated in heart failure, due to increased production and/or to reduced renal excretion of this antioxidant metabolite. The transformation of hypoxanthine to xanthine and the conversion of the latter into uric acid, which occur in purine catabolism, are catalysed by xanthine oxidoreductase. The constitutive xanthine dehydrogenase form of this enzyme generally uses NAD+ as an electron acceptor, whereas the post-translational xanthine oxidase form uses molecular oxygen and yields four units of reactive oxygen species per unit of transformed substrate. Allopurinol and oxypurinol inhibit xanthine oxidoreductase and thus diminish the generation of reactive species and decrease plasma uric acid. In a recent study in patients with NHYA class II-III heart failure, add-on treatment with allopurinol 300 mg/day for 3 months lowered plasma uric acid but failed to improve laboratory exercise performance or the distance walked in 6 minutes. In another recent trial, which was carried out in patients with NHYA class III-IV heart failure, add-on treatment with oxypurinol 600 mg/day for 24 weeks decreased plasma uric acid concentration but did not change a composite of patient outcome and state. These results indicate that the reduction in plasma uric acid caused by allopurinol or oxypurinol does not benefit patients with heart failure. Moreover, the hypothesis that the diminution in the renal excretion of the antioxidant uric acid caused by diuretics may be salutary in cardiac failure is strengthened by the study results considered.
Similar content being viewed by others
References
Farquharson CA, Butler R, Hill A, Belch JJ, Struthers AD. Allopurinol improves endothelial dysfunction in chronic heart failure. Circulation 2002;106:221–226.
Doehner W, Schoene N, Rauchhaus M, et al. Effects of xanthine oxidase inhibition with allopurinol on endothelial function and peripheral blood flow in hyperuricemic patients with chronic heart failure: results from 2 placebo-controlled studies. Circulation 2002;105:2619–2624.
Butler R, Morris AD, Belch JJ, Hill A, Struthers AD. Allopurinol normalizes endothelial dysfunction in type 2 diabetics with mild hypertension. Hypertension 2000;35:746–751.
Guthikonda S, Sinkey C, Barenz T, Haynes WG. Xanthine oxidase inhibition reverses endothelial dysfunction in heavy smokers. Circulation 2003;107:416–421.
Mercuro G, Vitale C, Cerquetani E, et al. Effect of hyperuricemia upon endothelial function in patients at increased cardiovascular risk. Am J Cardiol 2004;94:932–935.
Gavin AD, Struthers AD. Allopurinol reduces B-type natriuretic peptide concentrations and haemoglobin but does not alter exercise capacity in chronic heart failure. Heart 2005;91:749–753.
Freudenberger RS, Schwarz RP Jr, Brown J, et al. Rationale, design and organisation of an efficacy and safety study of oxypurinol added to standard therapy in patients with NYHA class III - IV congestive heart failure. Expert Opin Investig Drugs 2004;13:1509–1516.
Cardiome Pharma Corp. Cardiome Press Release. Cardiome reports clinical results from OPT-CHF Study [cited 2005 Aug 23]. Available from: http://www.cardiome.com/wordpress/index.php?cat=2
Ferrari R, Guardigli G, Mele D, Percoco GF, Ceconi C, Curello S. Oxidative stress during myocardial ischaemia and heart failure. Curr Pharm Des 2004;10:1699–1711.
Giordano FJ. Oxygen, oxidative stress, hypoxia and heart failue. J Clin Invest 2005;115:500–508.
Hare JM, Stamler JS. NO/redox desequilibrium in the failing heart and cardiovascular system. J Clin Invest 2005;115;509–517.
Regoli F, Winston GW. Quantification of total oxidant scavenging capacity of antioxidants for peroxynitrite, peroxyl radicals, and hydroxyl radicals. Toxicol Appl Pharmacol 1999;156:96–105.
Kuzkaya N, Weissmann N, Harrison DG, Dikalov S. Interactions of peroxynitrite with uric acid in the presence of ascorbate and thiols: Implications for uncoupling endothelial nitric oxide synthase. Biochem Pharmacol 2005;70:343–354.
Trostchansky A, Ferrer-Sueta G, Batthyany C, et al. Peroxynitrite flux-mediated LDL oxidation is inhibited by manganese porphyrins in the presence of uric acid. Free Radic Biol Med 2003;35:1293–1300.
Maxwell SR, Thomason H, Sandler D, et al. Antioxidant status in patients with uncomplicated insulin-dependent and non-insulin-dependent diabetes mellitus. Eur J Clin Invest 1997;27:484–490.
Antolini F, Valente F, Ricciardi D, Fagugli RM. Normalization of oxidative stress parameters after kidney transplant is secondary to full recovery of renal function. Clin Nephrol 2004;62:131–137.
Landmesser U, Spiekermann S, Dikalov S, et al. Vascular oxidative stress and endothelial dysfunction in patients with chronic heart failure: Role of xanthine-oxidase and extracellular superoxide dismutase. Circulation 2002;106:3073–3078.
Garattini E, Mendel R, Romão RJ, Wright R, Terao M. Mammalian molibdo-flavoenzymes, an expanding family of proteins: Structure, genetics, regulation, function and pathophysiology. Biochem J 2003;372:15–32.
Berry CE, Hare JM. Xanthine oxidoreductase and cardiovascular disease – molecular mechanisms and pathophysiologic implications. J Physiol 2004;555:589–606.
Li JM, Shah AM. Endothelial cell superoxide generation: Regulation and relevance for cardiovascular pathophysiology. Am J Physiol Regul Integr Comp Physiol 2004;287:R1014–R1030.
Madamanchi NR, Vendrov A, Runge MS. Oxidative stress and vascular disease. Arterioscler Thromb Vasc Biol 2005;25:29–38.
Sachidanandam K, Fagan SC, Erdul A. Oxidative stress and cardiovascular disease: Antioxidants and unresolved issues. Cardiovasc Drugs Rev 2005;23:115–132.
Reyes AJ. The increase in serum uric acid concentration caused by diuretics might be beneficial in heart failure. Eur J Heart Fail 2005;7: 461–467.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Reyes, A.J., Leary, W.P. Allopurinol or Oxypurinol in Heart Failure Therapy – a Promising New Development or End of Story?. Cardiovasc Drugs Ther 19, 311–313 (2005). https://doi.org/10.1007/s10557-005-4971-1
Issue Date:
DOI: https://doi.org/10.1007/s10557-005-4971-1