Abstract
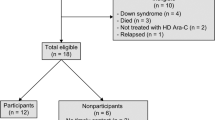
Childhood cancer survivors are at higher risk of developing neurocognitive deficits due to the intensive treatment they received at an early age. Most studies on childhood cancer survivorship have so far focused on the Western populations. Due to the ethnic, genetic, environmental, and cultural differences, clinical data of the Western populations may not be representative of Asian countries. This scoping review systematically summarized the existing clinical evidence of the neurocognitive impairment of Asian childhood cancer survivors. We searched the Embase and Medline databases for studies assessing the neurocognitive functions of survivors in Asia, who were diagnosed with cancer before the age of 19 and completed active treatment. The literature search identified 13 studies involving 2212 participants from five Asian countries: South Korea (n = 4, 30.8%), Taiwan (n = 3, 23.1%), Japan (n = 3, 23.1%), Hong Kong (n = 2, 15.4%), and Thailand (n = 1, 7.7%). The included studies focused on CNS tumors (n = 10, 76.9%), hematological malignancies (n = 7, 53.8%), or heterogeneous cancer diagnoses (n = 3, 23.1%). Collectively, mild-to-moderate impairment in intelligence was observed in 10.0 to 42.8% of survivors, which seemed higher than the reported rate in Western survivors. We speculate that the ethnic and genetic variations in drug responses and susceptibility to adverse chronic toxicities may have contributed to the differences in the prevalence and severity of neurocognitive impairment between these two populations. To better understand the effects of culturally relevant and region-specific environmental risk factors on the post-treatment neurocognitive development in cancer survivors, a holistic approach that addresses the complex interactions between biological, physical, and psychosocial factors is needed. This will aid the development of effective intervention strategies to improve the functional and psychosocial outcomes of cancer survivors in Asian societies.


Similar content being viewed by others
References
Steliarova-Foucher, E., Colombet, M., Ries, L. A. G., Moreno, F., Dolya, A., Bray, F., et al. (2017). International incidence of childhood cancer, 2001-10: a population-based registry study. The Lancet Oncology. https://doi.org/10.1016/S1470-2045(17)30186-9.
Rodriguez-Galindo, C., Friedrich, P., Alcasabas, P., Antillon, F., Banavali, S., Castillo, L., et al. (2015). Toward the cure of all children with cancer through collaborative efforts: pediatric oncology as a global challenge. Journal of Clinical Oncology. https://doi.org/10.1200/JCO.2014.60.6376.
Gelband, H., Jha, P., Sankaranarayanan, R., Horton, S., & Washington. (2017). Treating childhood cancers in low- and middle-income countries. Disease Control Priorities (third edition): Volume 3. Cancer. https://doi.org/10.1097/JDN.0000000000000342.
Park, H. J., Moon, E., Yoon, J. Y., Oh, C., Jung, K., Park, B. K., et al. (2016). Incidence and survival of childhood cancer in Korea. Cancer Research and Treatment. https://doi.org/10.4143/crt.2015.290.
Nakata, K., Ito, Y., Magadi, W., Bonaventure, A., Stiller, C. A., Katanoda, K., et al. (2018). Childhood cancer incidence and survival in Japan and England: a population-based study (1993-2010). Cancer Science. https://doi.org/10.1111/cas.13457.
Wiangnon, S., Jetsrisuparb, A., Komvilaisak, P., & Suwanrungruang, K. (2014). Childhood cancer incidence and survival 1985-2009, Khon Kaen, Thailand. Asian Pacific Journal of Cancer Prevention. https://doi.org/10.7314/apjcp.2014.15.18.7989.
Arora, R. S., Eden, T. O. B., & Kapoor, G. (2009). Epidemiology of childhood cancer in India. Indian Journal of Cancer. https://doi.org/10.4103/0019-509X.55546.
Zheng, R., Peng, X., Zeng, H., Zhang, S., Chen, T., Wang, H., et al. (2015). Incidence, mortality and survival of childhood cancer in China during 2000-2010 period: a population-based study. Cancer Letters. https://doi.org/10.1016/j.canlet.2015.04.021.
Aung, L., Khyne, T., Yeoh, A. E. J., Quah, T. C., & Tan, A. M. (2009). A report from the Singapore childhood cancer survivor study (SG-CCSS): a multi-institutional collaborative study on long-term survivors of childhood cancer, initial analysis reporting for the SG-CCSS. Annals of the Academy of Medicine of Singapore, 38(8), 684–689.
Howard, S. C., Zaidi, A., Cao, X., Weil, O., Bey, P., Patte, C., et al. (2018). The my child matters programme: effect of public–private partnerships on paediatric cancer care in low-income and middle-income countries. The Lancet Oncology. https://doi.org/10.1016/S1470-2045(18)30123-2.
Landier, W., Armenian, S., & Bhatia, S. (2015). Late effects of childhood cancer and its treatment. Pediatric Clinics of North America. https://doi.org/10.1016/j.pcl.2014.09.017.
Brennan, B. M., Rahim, A., Adams, J. A., Eden, O. B., & Shalet, S. M. (1999). Reduced bone mineral density in young adults following cure of acute lymphoblastic leukaemia in childhood. British Journal of Cancer., 79, 1859–1863. https://doi.org/10.1038/sj.bjc.6690296.
Nottage, K., Lanctot, J., Li, Z., Neglia, J. P., Bhatia, S., Hammond, S., et al. (2011). Long-term risk for subsequent leukemia after treatment for childhood cancer: a report from the Childhood Cancer Survivor Study. Blood. https://doi.org/10.1182/blood-2011-02-335158.
Neglia, J. P., Friedman, D. L., Yasui, Y., Mertens, A. C., Hammond, S., Stovall, M., et al. (2001). Second malignant neoplasms in five-year survivors of childhood cancer: childhood cancer survivor study. Journal of the National Cancer Institute. https://doi.org/10.1093/jnci/93.8.618.
Garmey, E. G., Liu, Q., Sklar, C. A., Meacham, L. R., Mertens, A. C., Stovall, M. A., et al. (2008). Longitudinal changes in obesity and body mass index among adult survivors of childhood acute lymphoblastic leukemia: a report from the Childhood Cancer Survivor Study. Journal of Clinical Oncology. https://doi.org/10.1200/JCO.2008.16.3527.
Oeffinger, K. C. (2008). Are survivors of acute lymphoblastic leukemia (ALL) at increased risk of cardiovascular disease? Pediatric Blood & Cancer. https://doi.org/10.1002/pbc.21410.
Bowers, D. C., Liu, Y., Leisenring, W., McNeil, E., Stovall, M., Gurney, J. G., et al. (2006). Late-occurring stroke among long-term survivors of childhood leukemia and brain tumors: a report from the Childhood Cancer Survivor Study. Journal of Clinical Oncology. https://doi.org/10.1200/JCO.2006.07.2884.
Phillips, S. M., Padgett, L. S., Leisenring, W. M., Stratton, K. K., Bishop, K., Krull, K. R., et al. (2015). Survivors of childhood cancer in the United States: prevalence and burden of morbidity. Cancer Epidemiology, Biomarkers & Prevention. https://doi.org/10.1158/1055-9965.EPI-14-1418.
Christiansen, H. L., Bingen, K., Hoag, J. A., Karst, J. S., Velázquez-Martin, B., & Barakat, L. P. (2015). Providing children and adolescents opportunities for social interaction as a standard of care in pediatric oncology. Pediatric Blood & Cancer. https://doi.org/10.1002/pbc.25774.
Wenninger, K., Helmes, A., Bengel, J., Lauten, M., Völkel, S., & Niemeyer, C. M. (2013). Coping in long-term survivors of childhood cancer: relations to psychological distress. Psycho-Oncology. https://doi.org/10.1002/pon.3073.
Lown, E. A., Phillips, F., Schwartz, L. A., Rosenberg, A. R., & Jones, B. (2015). Psychosocial follow-up in survivorship as a standard of care in pediatric oncology. Pediatric Blood & Cancer. https://doi.org/10.1002/pbc.25783.
Schrag, N. M., McKeown, R. E., Jackson, K. L., Cuffe, S. P., & Neuberg, R. W. (2008). Stress-related mental disorders in childhood cancer survivors. Pediatric Blood & Cancer. https://doi.org/10.1002/pbc.21285.
Lown, E. A., Hijiya, N., Zhang, N., Srivastava, D. K., Leisenring, W. M., Nathan, P. C., et al. (2016). Patterns and predictors of clustered risky health behaviors among adult survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Cancer. https://doi.org/10.1002/cncr.30106.
Wengenroth L., Rueegg CS., Michel G., Gianinazzi ME., Essig S., von der Weid., et al. (2015). Concentration, working speed and memory: cognitive problems in young childhood cancer survivors and their siblings. Pediatric Blood & Cancer. doi: https://doi.org/10.1002/pbc.25396.
Ellenberg, L., Liu, Q., Gioia, G., Yasui, Y., Packer, R. J., Mertens, A., et al. (2009). Neurocognitive status in long-term survivors of childhood CNS malignancies. Neuropsychology. https://doi.org/10.1037/a0016674.
Goss, P. E., Strasser-Weippl, K., Lee-Bychkovsky, B. L., Fan, L., Li, J., Chavarri-Guerra, Y., et al. (2014). Challenges to effective cancer control in China, India, and Russia. The Lancet Oncology. https://doi.org/10.1016/S1470-2045(14)70029-4.
Working Together to Address Complex health Challenges. Association of Southeast Asian Nations. In: ASEAN | ONE VISION ONE IDENTITY ONE COMMUNITY. https://asean.org/asean-socio-cultural/asean-health-ministers-meeting-ahmm/overview-2/. Accessed 18 Oct 2019.
SIOP Asia (International Society of Paediatric Oncology) Asia. https://siop-online.org/sp_cb/asia/. Accessed 18 Oct 2019.
Childhood Cancer International (2015) Asia. https://www.childhoodcancerinternational.org/cci-global-network/asia/. Accessed 18 Oct 2019.
Poon, L. H. J., Yu, C., Peng, L., Ewig, C. L., Zhang, H., Li, C., et al. (2019). Clinical ascertainment of health outcomes in Asian survivors of childhood cancer: a systematic review. Journal of Cancer Survivorship., 13, 374–396. https://doi.org/10.1007/s11764-019-00759-9.
Study quality assessment tool for observational cohort and cross-sectional studies. National Herat, Lung and Blood Institute. https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools. Accessed 13 Sept 2019.
Connolly, M. P., Haitsma, G., Hernández, A. V., & Vidal, J. E. (2017). Systematic review and meta-analysis of secondary prophylaxis for prevention of HIV-related toxoplasmic encephalitis relapse using trimethoprim-sulfamethoxazole. Pathogens and Global Health. https://doi.org/10.1080/20477724.2017.1377974.
Protogerou, C., & Hagger, M. S. (2018). A case for a study quality appraisal in survey studies in psychology. Frontiers in Psychology. https://doi.org/10.3389/fpsyg.2018.02788.
Ketsuwan, S., Surayuthpreecha, K., Chuthapisith, Anurathapan, U., Pakakasama, S., Numthavaj, P., et al. (2019). The adverse effect of intellectual outcome in childhood cancer survivors. Journal of the Medical Association of Thailand, 102(8), 841–847.
Chiou, S., Lin, P., Liao, Y., & Yang, P. (2019). A cross-sectional follow-up study of physical morbidities, neurocognitive function, and attention problems in post-treatment childhood acute lymphoblastic leukemia survivors. The Kaohsiung Journal of Medical Sciences. https://doi.org/10.1002/kjm2.12061.
Tso, W. W. Y., Liu, A. P. Y., Lee, T. M. C., Cheuk, K. L., Shing, M. K., Luk, C. W., Ling, S. C., Ku, D. T. L., Li, K., Yung, A. W. Y., Fung, C. W., Chan, S. H. S., Ho, A. C. C., Ho, F. K. W., Ip, P., & Chan, G. C. F. (2019). Neurocognitive function, performance status, and quality of life in pediatric intracranial germ cell tumor survivors. Journal of Neuro-oncology., 141, 393–401. https://doi.org/10.1007/s11060-018-03045-3.
Kim, M. A., Park, J. H., Park, H. J., Yi, J., Ahn, E., Kim, S. Y., et al. (2018). Experiences of peer exclusion and victimization, cognitive functioning, and depression among adolescent cancer survivors in South Korea. American Journal of Orthopsychiatry. https://doi.org/10.1037/ort0000292.
Oh, Y., Seo, H., Sung, K. W., & Joung, Y. S. (2017). The effects of attention problems on psychosocial functioning in childhood brain tumor survivors: a 2-Year postcraniospinal irradiation follow-up. Journal of Pediatric Hematology/ Oncology. https://doi.org/10.1097/MPH.0000000000000766.
Yoo, H. J., Kim, H., Park, H. J., Kim, D. S., Ra, Y. S., & Shin, H. Y. (2016). Neurocognitive function and health-related quality of life in pediatric Korean survivors of medulloblastoma. Journal of Korean Medical Science. https://doi.org/10.3346/jkms.2016.31.11.1726.
Kim, S. J., Park, M. H., Lee, J. W., Chung, N. G., Cho, B., Lee, I. G., et al. (2015). Neurocognitive outcome in survivors of childhood acute lymphoblastic keukemia: experience at a tertiary care hospital in Korea. Journal of Korean Medical Science. https://doi.org/10.3346/jkms.2015.30.4.463.
Sato, I., Higuchi, A., Yanagisawa, T., Murayama, S., Kumabe, T., Sugiyama, K., et al. (2014). Impact of late effects on health-related quality of life in survivors of pediatric brain tumors: motility disturbance of limb(s), seizure, ocular/visual impairment, endocrine abnormality, and higher brain dysfunction. Cancer Nursing. https://doi.org/10.1097/NCC.0000000000000110.
Odagiri, K., Omura, M., Hata, M., Aida, N., Niwa, T., Goto, H., Ito, S., Adachi, M., Yoshida, H., Yuki, H., & Inoue, T. (2014). Treatment outcomes and late toxicities in patients with embryonal central nervous system tumors. Radiation Oncology, 9, 1–12. https://doi.org/10.1186/1748-717X-9-201.
Liang, S., Yang, T., Chen, Y., Liang, M., Chen, H., Chang, K., et al. (2013). Neuropsychological functions and quality of life in survived patients with intracranial germ cell tumors after treatment. Neuro-oncology. https://doi.org/10.1093/neuonc/not127.
Ishida, Y., Sakamoto, N., Kamibeppu, K., Kakee, N., Iwai, T., Ozono, S., et al. (2010). Late effects and quality of life of childhood cancer survivors: part 2. Impact of radiotherapy. International Journal of Hematology. doi. https://doi.org/10.1007/s12185-010-0611-z.
Chiou, S., Jang, R., Liao, Y., & Yang, P. (2010). Health-related quality of life and cognitive outcomes among child and adolescent survivors of leukemia. Supportive Care in Cancer, 18, 1581–1587. https://doi.org/10.1007/s00520-009-0781-5.
Khong, P., Leung, L. H. T., Fung, A. S. M., Fong, D. Y. T., Qiu, D., Kwong, D. L. W., et al. (2006). White matter anisotropy in post-treatment childhood cancer survivors: preliminary evidence of association with neurocognitive function. Journal of Clinical Oncology. https://doi.org/10.1200/JCO.2005.02.4505.
Conklin, H. M., Krull, K. R., Reddick, W. E., Pei, D., Cheng, C., & Pui, C. H. (2012). Cognitive outcomes following contemporary treatment without cranial irradiation for childhood acute lymphoblastic leukemia. Journal of the National Cancer Institute. https://doi.org/10.1093/jnci/djs344.
Krull, K. R., Hardy, K. K., Kahalley, L. S., Schuitema, I., & Kesler, S. R. (2018). Neurocognitive outcomes and interventions in long-term survivors of childhood cancer. Journal of Clinical Oncology : official journal of the American Society of Clinical Oncology. https://doi.org/10.1200/JCO.2017.76.4696.
Ehrhardt, M. J., Mulrooney, D. A., Li, C., Baassiri, M. J., Bjornard, K., Sandlund, J. T., et al. (2018). Neurocognitive, psychosocial, and quality-of-life outcomes in adult survivors of childhood non-Hodgkin lymphoma. Cancer. https://doi.org/10.1002/cncr.31019.
Beechinor, R. J., Thompson, P. A., Hwang, M. F., Vargo, R. C., Bomgaars, L. R., Gerhart, J. G., et al. (2019). The population pharmacokinetics of high-dose methotrexate in infants with acute lymphoblastic leukemia highlight the need for bedside individualized dose adjustment: a report from the children’s oncology group. Clinical Pharmacokinetics. https://doi.org/10.1007/s40262-018-00734-0.
Krull, K. R., Cheung, Y. T., Liu, W., Fellah, S., Reddick, W. E., Brinkman, T. M., et al. (2016). Chemotherapy pharmacodynamics and neuroimaging and neurocognitive outcomes in long-term survivors of childhood acute lymphoblastic leukemia. Journal of Clinical Oncology. https://doi.org/10.1200/JCO.2015.65.4574.
Cheung, Y. T., Brinkman, T. M., Li, C., Mzayek, Y., Srivastava, D., Ness, K. K., et al. (2018). Chronic health conditions and neurocognitive function in aging survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Journal of the National Cancer Institute. https://doi.org/10.1093/jnci/djx224.
Zeltzer, L. K., Recklitis, C., Buchbinder, D., Zebrack, B., Casillas, J., Tsao, J. C. I., et al. (2009). Psychological status in childhood cancer survivors: a report from the Childhood Cancer Survivor Study. Journal of Clinical Oncology. https://doi.org/10.1200/JCO.2008.21.1433.
Ueshima, H., Sekikawa, A., Miura, K., Turin, T. C., Takashima, N., Kita, Y., et al. (2008). Cardiovascular disease and risk factors in Asia: a selected review. Circulation. https://doi.org/10.1161/CIRCULATIONAHA.108.790048.
Pechtel, P., & Pizzagalli, D. (2011). Effects of early life stress on cognitive and affective function: an integrated review of human literature. Psychopharmacology. https://doi.org/10.1007/s00213-010-2009-2.
Glass, J. M., Buu, A., Adams, K. M., Nigg, J. T., Puttler, L. I., Jester, J. M., et al. (2009). Effects of alcoholism severity and smoking on executive neurocognitive function. Addiction. https://doi.org/10.1111/j.1360-0443.2008.02415.x.
Stillman, C. M., Cohen, J., Lehman, M. E., & Erickson, K. I. (2016). Mediators of physical activity on neurocognitive function: a review at multiple levels of analysis. Frontiers in Human Neuroscience. https://doi.org/10.3389/fnhum.2016.00626.
Ho, K. Y., Li, W. H. C., Lam, K. W. K., Wei, X., Chiu, S. Y., Chan, C. G., et al. (2019). Relationships among fatigue, physical activity, depressive symptoms, and quality of life in Chinese children and adolescents surviving cancer. European Journal of Oncology Nursing. https://doi.org/10.1016/j.ejon.2018.11.007.
Cheung, Y. T., Brinkman, T. M., Mulrooney, D. A., Mzayek, Y., Liu, W., Banerjee, P., et al. (2017). Impact of sleep, fatigue, and systemic inflammation on neurocognitive and behavioral outcomes in long-term survivors of childhood acute lymphoblastic leukemia. Cancer. https://doi.org/10.1002/cncr.30742.
Biddle, G. J. H., Edwardson, C. L., Rowlands, A. V., Davies, M. J., Bodicoat, D. H., Hardeman, W., Eborall, H., Sutton, S., Griffin, S., Khunti, K., & Yates, T. (2019). Differences in objectively measured physical activity and sedentary behaviour between white Europeans and South Asians recruited from primary care: cross-sectional analysis of the PROPELS trial. BMC Public Health, 19, 1–12. https://doi.org/10.1186/s12889-018-6341-5.
Liu, J., & Lewis, G. (2014). Environmental toxicity and poor cognitive outcomes in children and adults. Journal of Environmental Health, 76(6), 130–138.
Armstrong, G. T., Sklar, C. A., Hudson, M. M., & Robison, L. L. (2007). Long-term health status among survivors of childhood cancer: does sex matter? Journal of Clinical Oncology.
Cheung, Y. T., Sabin, N. D., Reddick, W. E., Bhojwani, D., Liu, W., Brinkman, T. M., et al. (2016). Leukoencephalopathy and long-term neurobehavioral, neurocognitive and brain imaging outcomes in survivors of childhood acute lymphoblastic leukemia treated with chemotherapy: a longitudinal analysis. The Lancet. Haematology. https://doi.org/10.1016/S2352-3026(16)30110-7.
Cheung, Y. T., & Krull, K. R. (2015). Neurocognitive outcomes in long-term survivors of childhood acute lymphoblastic leukemia treated on contemporary treatment protocols: a systematic review. Neuroscience & Biobehavioral Reviews. https://doi.org/10.1016/j.neubiorev.2015.03.016.
Spiegler, B. J., Kennedy, K., Maze, R., Greenberg, M. L., Weitzman, S., Hitzler, J. K., et al. (2006). Comparison of long-term neurocognitive outcomes in young children with acute lymphoblastic leukemia treated with cranial radiation or high-dose or very high-dose intravenous methotrexate. Journal of Clinical Oncology. https://doi.org/10.1200/JCO.2006.05.9055.
Edelmann, M. N., Krull, K. R., Liu, W., Glass, J. O., Ji, Q., Ogg, R. J., et al. (2014). Diffusion tensor imaging and neurocognition in survivors of childhood acute lymphoblastic leukaemia. Brain. https://doi.org/10.1093/brain/awu230.
Harila, M. J., Winqvist, S., Lanning, M., Bloigu, R., & Harila-Saari, A. H. (2009). Progressive neurocognitive impairment in young adult survivors of childhood acute lymphoblastic leukemia. Pediatric Blood & Cancer. https://doi.org/10.1002/pbc.21992.
Lee, J. W., Aminkeng, F., Bhavsar, A. P., Shaw, K., Carleton, B. C., Hayden, M. R., et al. (2014). The emerging era of pharmacogenomics: current successes, future potential, and challenges. Clinical Genetics. https://doi.org/10.1111/cge.12392.
Suthandiram, S., Gan, G., Zain, S. M., Bee, P., Lian, L., Chang, K., et al. (2014). Effect of polymorphisms within methotrexate pathway genes on methotrexate toxicity and plasma levels in adults with hematological malignancies. Pharmacogenomics. https://doi.org/10.2217/pgs.14.97.
Oeffinger, K. C., Mertens, A. C., Sklar, C. A., Kawashima, T., Hudson, M. M., Meadows, A. T., et al. (2006). Chronic health conditions in adult survivors of childhood cancer. The New England Journal of Medicine. https://doi.org/10.1056/NEJMsa060185.
Vassilaki, M., Aakre, J. A., Cha, R. H., Kremers, W. K., St Sauver, J. L., Mielke, M. M., et al. (2015). Multimorbidity and risk of mild cognitive impairment. Journal of the American Geriatrics Society. https://doi.org/10.1111/jgs.13612.
Iyer, N. S., Balsamo, L. M., Bracken, M. B., & Kadan-Lottick, N. S. (2015). Chemotherapy-only treatment effects on long-term neurocognitive functioning in childhood ALL survivors: a review and meta-analysis. Blood. https://doi.org/10.1182/blood-2015-02-627414.
Ness, K. K., Armenian, S. H., Kadan-Lottick, N., & Gurney, J. G. (2011). Adverse effects of treatment in childhood acute lymphoblastic leukemia: general overview and implications for long-term cardiac health. Expert Review of Hematology. https://doi.org/10.1586/ehm.11.8.
Kesler, S., Janelsins, M., Koovakkattu, D., Palesh, O., Mustian, K., Morrow, G., et al. (2013). Reduced hippocampal volume and verbal memory performance associated with interleukin-6 and tumor necrosis factor-alpha levels in chemotherapy-treated breast cancer survivors. Brain, Behavior, and Immunity. https://doi.org/10.1016/j.bbi.2012.05.017.
Pomykala, K. L., Ganz, P. A., Bower, J. E., Kwan, L., Castellon, S. A., Mallam, S., et al. (2013). The association between pro-inflammatory cytokines, regional cerebral metabolism, and cognitive complaints following adjuvant chemotherapy for breast cancer. Brain Imaging and Behavior. https://doi.org/10.1007/s11682-013-9243-2.
Janelsins, M. C., Mustian, K. M., Palesh, O. G., Mohile, S. G., Peppone, L. J., Sprod, L. K., et al. (2012). Differential expression of cytokines in breast cancer patients receiving different chemotherapies: implications for cognitive impairment research. Supportive Care in Cancer. https://doi.org/10.1007/s00520-011-1158-0.
Cheung, Y. T., Edelmann, M. N., Mulrooney, D. A., Green, D. M., Chemaitilly, W., John, N., et al. (2016). Uric acid and neurocognitive function in survivors of childhood acute lymphoblastic leukemia treated with chemotherapy only. Cancer Epidemiology, Biomarkers & Prevention : a Publication of the American Association for Cancer Research, cosponsored by the American Society of Preventive Oncology. https://doi.org/10.1158/1055-9965.EPI-16-0118.
Mladěnka, P., Applová, L., Patočka, J., Costa, V. M., Remiao, F., Pourová, J., et al. (2018). Comprehensive review of cardiovascular toxicity of drugs and related agents. Medical Research Reviews. https://doi.org/10.1002/med.21476.
Lee, T. K., Huang, Z. S., Ng, S. K., Chan, K. W., Wang, Y. S., Liu, H. W., et al. (1995). Impact of alcohol consumption and cigarette smoking on stroke among the elderly in Taiwan. Stroke. https://doi.org/10.1161/01.str.26.5.790.
Zakhari, S. (1997). Alcohol and the cardiovascular system: molecular mechanisms for beneficial and harmful action. Alcohol Health and Research World, 21(1), 21–29.
GHO | World Health Statistics data visualizations dashboard | Data tables - Country data. WHO. World Health Organization. http://apps.who.int/gho/data/view.sdg.3-a-data-ctry?lang=en. Accessed 8 Nov 2019.
Dixon, S. B., Li, N., Yasui, Y., Bhatia, S., Casillas, J. N., Gibson, T. M., et al. (2019). Racial and ethnic disparities in neurocognitive, emotional, and quality-of-life outcomes in survivors of childhood cancer: a report from the Childhood Cancer Survivor Study. Cancer. https://doi.org/10.1002/cncr.32370.
Sun, J., Dunne, M. P., Hou, X., & Xu, A. (2013). Educational stress among Chinese adolescents: individual, family, school and peer influences. Educational Review. https://doi.org/10.1080/00131911.2012.659657.
Chen, X., & Glaude, M. W. (1997). Academic stress among Chinese adolescents: can psychological stress theory explain this tragedy? International Journal of Humanities and Social Sciences, 7(2), 17–25.
Ferguson, K. T., Cassells, R. C., MacAllister, J. W., & Evans, G. W. (2013). The physical environment and child development: an international review. International Journal of Psychology. https://doi.org/10.1080/00207594.2013.804190.
Brockmeyer, S., & D’Angiulli, A. (2016). How air pollution alters brain development: the role of neuroinflammation. Translational Neuroscience. https://doi.org/10.1515/tnsci-2016-0005.
Bhang S., Yoon J., Sung J., Yoo C., Sim C., Lee C., et al. (2018). Comparing attention and cognitive function in school children across noise conditions: a quasi-experimental study. Psychiatry investigation. doi: https://doi.org/10.30773/pi.2018.01.15.
Fowler, P. J., McGrath, L. M., Henry, D. B., Schoeny, M., Chavira, D., Taylor, J. J., et al. (2015). Housing mobility and cognitive development: change in verbal and nonverbal abilities. Child Abuse & Neglect. https://doi.org/10.1016/j.chiabu.2015.06.002.
Fry, C. E., Langley, K., & Shelton, K. H. (2019). Executive functions in homeless young people: working memory impacts on short-term housing outcomes. Child Neuropsychology. https://doi.org/10.1080/09297049.2019.1628930.
Wong, C. S. M., Wong, T. Y., Chan, W. C., Lam, L. C. W., Law, W. Y., Tang, W. Y., et al. (2016). Living environment and psychological distress in the general population of Hong Kong. Procedia Environmental Sciences. https://doi.org/10.1016/j.proenv.2016.09.016.
Funding
This study is funded by the Hong Kong Research Grant Council (ref no: 24614818), awarded to Yin Ting Cheung.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study does not involve human or animals as subjects.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Peng, L., Yam, P.PY., Yang, L.S. et al. Neurocognitive impairment in Asian childhood cancer survivors: a systematic review. Cancer Metastasis Rev 39, 27–41 (2020). https://doi.org/10.1007/s10555-020-09857-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10555-020-09857-y