Abstract
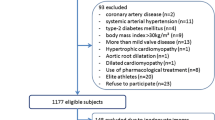
Cardiac power output (CPO), which combines pressure and flow capacities, directly measures the heart’s pumping capability. It is proposed as a superior alternative to ejection fraction in assessing cardiac function. However, there is a lack of data on CPO in healthy individuals, prompting a study to determine the cardiac power output in healthy adults in the Iranian population. This cross-sectional descriptive study investigated cardiac power in a sample of healthy individuals. Participants were recruited from healthy individuals referred to the Echocardiography department using convenience sampling. In this study, we examined the echocardiographic parameters in 173 individuals, of which 52% were men. Men exhibited significantly higher values for stroke volume, cardiac output, and cardiac power output (CPO) in both ventricles, as well as larger body surface area (BSA) and systemic mean arterial pressure (MAP), compared to women. Individuals under the age of 40 had significantly higher BSA and right ventricular cardiac output compared to those aged 40 or above. Multivariate analysis revealed that MAP, left ventricular (LV) cardiac output, LVCPO, pulmonary MAP, right ventricular (RV) CPO, and RV cardiac power index (CPI) were significant predictors of LVCPI changes. Our findings emphasize the importance of cardiac power output as a comprehensive measure of cardiac function, complementing the traditional use of ejection fraction. Further research is warranted to validate these results, establish accurate reference ranges, and explore the clinical implications of cardiac power output in various patient populations.





Similar content being viewed by others
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Corsini A, Cercenelli L, Zecchi M, Marcelli E, Corazza I (2022) Chapter 30—basic hemodynamic parameters. In: Karimov JH, Fukamachi K, Gillinov M (eds) Advances in cardiovascular technology. Academic Press, pp 463–474
Calvert JW, Lefer DJ (2012) Chapter 6—overview of cardiac muscle physiology. In: Hill JA, Olson EN (eds) Muscle. Academic Press, Boston/Waltham, pp 57–66
Gopalan C, Kirk E (2022) Chapter 2—the blood vessels. In: Gopalan C, Kirk E (eds) Biology of cardiovascular and metabolic diseases. Academic Press, Cambridge, pp 35–51
Hryvniak D, Wilder RP, Jenkins J, Statuta SM (2021) 15—therapeutic exercise. In: Cifu DX (ed) Braddom’s physical medicine and rehabilitation, 6th edn. Elsevier, Philadelphia, pp 291-315e4
Magder SA (2012) The ups and downs of heart rate. Crit Care Med 40(1):239–245
Jakovljevic DG, George RS, Donovan G, Nunan D, Henderson K, Bougard RS et al (2010) Comparison of cardiac power output and exercise performance in patients with left ventricular assist devices, explanted (recovered) patients, and those with moderate to severe heart failure. Am J Cardiol 105(12):1780–1785
Tan L (1986) Cardiac pumping capability and prognosis in heart failure. Lancet 328(8520):1360–1363
Schlader ZJ, Mündel T, Barnes MJ, Hodges LD (2010) Peak cardiac power output in healthy, trained men. Clin Physiol Funct Imaging 30(6):480–484
Fincke R, Hochman JS, Lowe AM, Menon V, Slater JN, Webb JG et al (2004) Cardiac power is the strongest hemodynamic correlate of mortality in cardiogenic shock: a report from the SHOCK trial registry. J Am Coll Cardiol 44(2):340–348
Grodin JL, Mullens W, Dupont M, Wu Y, Taylor DO, Starling RC, Tang WH (2015) Prognostic role of cardiac power index in ambulatory patients with advanced heart failure. Eur J Heart Fail 17(7):689–696
Koskela JK, Tahvanainen A, Haring A, Tikkakoski AJ, Ilveskoski E, Viitala J et al (2013) Association of resting heart rate with cardiovascular function: a cross-sectional study in 522 Finnish subjects. BMC Cardiovasc Disord 13(1):102
Harada T, Yamaguchi M, Omote K, Iwano H, Mizuguchi Y, Amanai S et al (2022) Cardiac power output is independently and incrementally associated with adverse outcomes in heart failure with preserved ejection fraction. Circ Cardiovasc Imaging 15(2):e013495
Olivotto I, Cecchi F, Poggesi C, Yacoub MH (2012) Patterns of disease progression in hypertrophic cardiomyopathy. Circ Heart Fail 5(4):535–546
Obokata M, Reddy Yogesh NV, Borlaug Barry A (2020) Diastolic dysfunction and heart failure with preserved ejection fraction. JACC: Cardiovasc Imaging 13(1Part2):245–257
Kagami K, Obokata M, Harada T, Kato T, Wada N, Adachi T, Ishii H (2022) Diastolic filling time, chronotropic response, and exercise capacity in heart failure and preserved ejection fraction with sinus rhythm. J Am Heart Assoc 11(13):e026009
Chiba Y, Iwano H, Aoyagi H, Tamaki Y, Motoi K, Ishizaka S et al (2023) Associations of right ventricular pulsatile load and cardiac power output to clinical outcomes in heart failure: difference from systemic circulation. J Cardiol 81(4):404–412
Mitchell C, Rahko PS, Blauwet LA, Canaday B, Finstuen JA, Foster MC et al (2019) Guidelines for performing a comprehensive transthoracic echocardiographic examination in adults: recommendations from the American society of echocardiography. J Am Soc Echocardiogr 32(1):1–64
Du Bois D, Du Bois EF (1989) A formula to estimate the approximate surface area if height and weight be known. 1916. Nutrition 5(5):303–311
Lu J, Yin L (2023) Sex differences in left ventricular stroke work and cardiac power output per unit myocardium relate to blood pressure in apparently healthy adults. PLoS ONE 18(1):e0280143
Dini FL, Mele D, Conti U, Ballo P, Citro R, Menichetti F, Marzilli M (2010) Peak power output to left ventricular mass: an index to predict ventricular pumping performance and morbidity in advanced heart failure. J Am Soc Echocardiogr 23(12):1259–1265
Cotter G, Moshkovitz Y, Kaluski E, Milo O, Nobikov Y, Schneeweiss A et al (2003) The role of cardiac power and systemic vascular resistance in the pathophysiology and diagnosis of patients with acute congestive heart failure. Eur J Heart Fail 5(4):443–451
Lang CC, Karlin P, Haythe J, Lim TK, Mancini DM (2009) Peak cardiac power output, measured noninvasively, is a powerful predictor of outcome in chronic heart failure. Circ Heart Fail 2(1):33–38
Cortigiani L, Sorbo S, Miccoli M, Scali MC, Simioniuc A, Morrone D et al (2017) Prognostic value of cardiac power output to left ventricular mass in patients with left ventricular dysfunction and dobutamine stress echo negative by wall motion criteria. Eur Heart J Cardiovasc Imaging 18(2):153–158
Pugliese NR, Fabiani I, Mandoli GE, Guarini G, Galeotti GG, Miccoli M et al (2019) Echo-derived peak cardiac power output-to-left ventricular mass with cardiopulmonary exercise testing predicts outcome in patients with heart failure and depressed systolic function. Eur Heart J Cardiovasc Imaging 20(6):700–708
Anand V, Kane GC, Scott CG, Pislaru SV, Adigun RO, McCully RB et al (2020) Prognostic value of peak stress cardiac power in patients with normal ejection fraction undergoing exercise stress echocardiography. Eur Heart J 42(7):776–785
Basir MB, Schreiber T, Dixon S, Alaswad K, Patel K, Almany S et al (2018) Feasibility of early mechanical circulatory support in acute myocardial infarction complicated by cardiogenic shock: the Detroit cardiogenic shock initiative. Catheter Cardiovasc Interv 91(3):454–461
Toufan M, Mohammadzadeh Gharebaghi S, Pourafkari L, Delir Abdolahinia E (2015) Systolic longitudinal function of the left ventricle assessed by speckle tracking in heart failure patients with preserved ejection fraction. J Tehran Heart Cent 10(4):194–200
Hachicha Z, Dumesnil JG, Pibarot P (2009) Usefulness of the valvuloarterial impedance to predict adverse outcome in asymptomatic aortic stenosis. J Am Coll Cardiol 54(11):1003–1011
Zito C, Salvia J, Cusmà-Piccione M, Antonini-Canterin F, Lentini S, Oreto G et al (2011) Prognostic significance of valvuloarterial impedance and left ventricular longitudinal function in asymptomatic severe aortic stenosis involving three-cuspid valves. Am J Cardiol 108(10):1463–1469
Antonini-Canterin F, Huang G, Cervesato E, Faggiano P, Pavan D, Piazza R, Nicolosi GL (2003) Symptomatic aortic stenosis: does systemic Hypertension play an additional role? Hypertension 41(6):1268–1272
Marshall P, Al-Timman J, Riley R, Wright J, Williams S, Hainsworth R (2001) TAN L-B: randomized controlled trial of home-based exercise training to evaluate cardiac functional gains. Clin Sci 101(5):477–483
Mimran A (2006) Consequences of elevated pulse pressure on renal function. J Hypertens 24:S3–S7
St Pierre SR, Peirlinck M, Kuhl E (2022) Sex matters: a comprehensive comparison of female and male hearts. Front Physiol 13:831179
Williams SG, Ng LL, O’Brien RJ, Taylor S, Wright DJ, Tan L-B (2004) Is plasma N-BNP a good indicator of the functional reserve of failing hearts? The FRESH-BNP study. Eur J Heart Fail 6(7):891–900
Alsharqi M, Woodward W, Mumith J, Markham D, Upton R, Leeson P (2018) Artificial intelligence and echocardiography. Echo Res Pract 5(4):R115
Acknowledgements
The authors would like to acknowledge and thank Dr. Morteza Ghojazadeh, Ph.D., for his important contributions to this effort.
Funding
Tabriz University of Medical Sciences, Tabriz, Iran.
Author information
Authors and Affiliations
Contributions
Conceptualization: MT-T. Data curation: LGN, MR. Software: MR. Methodology: MT-T, EJ, LGN. Writing—original draft: MR, LGN. Writing—review & editing: MT-T, EJ. Supervision: MT-T.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This article is part of a fellowship research project in echocardiography approved by the Ethics Committee at Tabriz University of Medical Sciences (IR.TBZMED.REC.1402.025).
Consent to participate
All participants gave written consent for participation in the study.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ghahremani-Nasab, L., Toufan-Tabrizi, M., Javanshir, E. et al. Assessing cardiac power output values in a healthy adult population. Int J Cardiovasc Imaging 40, 517–526 (2024). https://doi.org/10.1007/s10554-023-03019-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-023-03019-1