Abstract
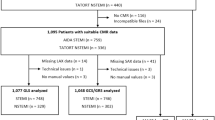
The diagnostic accuracy of exercise stress echocardiography (ESE) for myocardial ischemia requires improvement, given that it currently depends on the physicians’ experience and image quality. To address this issue, we aimed to develop artificial intelligence (AI)-based slow-motion echocardiography using inter-image interpolation. The clinical usefulness of this method was evaluated for detecting regional wall-motion abnormalities (RWMAs). In this study, an AI-based echocardiographic image-interpolation pipeline was developed using optical flow calculation and prediction for in-between images. The accuracy for detecting RWMAs and image readability among 25 patients with RWMA and 25 healthy volunteers was compared between four cardiologists using slow-motion and conventional ESE. Slow-motion echocardiography was successfully developed for arbitrary time-steps (e.g., 0.125×, and 0.5×) using 1,334 videos. The RWMA detection accuracy showed a numerical improvement, but it was not statistically significant (87.5% in slow-motion echocardiography vs. 81.0% in conventional ESE; odds ratio: 1.43 [95% CI: 0.78–2.62], p = 0.25). Interreader agreement analysis (Fleiss’s Kappa) for detecting RWMAs among the four cardiologists were 0.66 (95%CI: 0.55–0.77) for slow-motion ESE and 0.53 (95%CI: 0.42–0.65) for conventional ESE. Additionally, subjective evaluations of image readability using a four-point scale showed a significant improvement for slow-motion echocardiography (2.11 ± 0.73 vs. 1.70 ± 0.78, p < 0.001).In conclusion, we successfully developed slow-motion echocardiography using in-between echocardiographic image interpolation. Although the accuracy for detecting RWMAs did not show a significant improvement with this method, we observed enhanced image readability and interreader agreement. This AI-based approach holds promise in supporting physicians’ evaluations.



Similar content being viewed by others
Data availability
Private patient data access is limited for privacy reasons. Codes are publicly available in https://github.com/Gifu-University-Cardiology/Slow-motion-Echocardiography These codes were modified from https://github.com/avinashpaliwal/Super-SloMo.
Abbreviations
- A2C:
-
Apical-2-chamber
- A3C:
-
Apical-3-chamber
- A4C:
-
Apical-4-chamber
- AI:
-
Artificial Intelligence
- CI:
-
Confidence interval
- DICOM:
-
Digital Imaging and Communications in Medicine
- ESE:
-
Exercise stress echocardiography
- LVEF:
-
Left ventricular ejection fraction
- OR:
-
Odds ratio
- PLAX:
-
Parasternal long axis
- PSAX:
-
Parasternal short axis
- ROC:
-
Receiver operating characteristic
- RWMA:
-
Regional wall motion abnormality
References
Lindstrom M, DeCleene N, Dorsey H et al (2022) Global Burden of Cardiovascular Diseases and risks collaboration (1990–2021). J Am Coll Cardiol 80:2372–2425
Mitchell C, Rahko PS, Blauwet LA et al (2019) Guidelines for performing a comprehensive transthoracic echocardiographic examination in adults: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr 32:1–64. https://doi.org/10.1016/j.echo.2018.06.004
Woodward W, Dockerill C, McCourt A et al (2022) Real-world performance and accuracy of stress echocardiography: the EVAREST observational multi-centre study. Eur Heart J Cardiovasc Imaging 23:689–698. https://doi.org/10.1093/ehjci/jeab092
Picano E, Lattanzi F, Orlandini A, Marini C, L’Abbate A (1991) Stress echocardiography and the human factor: the importance of being expert. J Am Coll Cardiol 17:666–669. https://doi.org/10.1016/s0735-1097(10)80182-2
Anderson DR, Blissett S, O’Sullivan P, Qasim A (2021) Differences in echocardiography interpretation techniques among trainees and expert readers. J Echocardiogr 19:222–231. https://doi.org/10.1007/s12574-021-00531-y
Geleijnse ML, Krenning BJ, van Dalen BM et al (2009) Factors affecting sensitivity and specificity of diagnostic testing: dobutamine stress echocardiography. J Am Soc Echocardiogr 22:1199–1208. https://doi.org/10.1016/j.echo.2009.07.006
Johri AM, Picard MH, Newell J, Marshall JE, King ME, Hung J (2011) Can a teaching intervention reduce interobserver variability in LVEF assessment: a quality control exercise in the echocardiography lab. JACC Cardiovasc Imaging 4:821–829. https://doi.org/10.1016/j.jcmg.2011.06.004
Thavendiranathan P, Popović ZB, Flamm SD, Dahiya A, Grimm RA, Marwick TH (2013) Improved interobserver variability and accuracy of echocardiographic visual left ventricular ejection fraction assessment through a self-directed learning program using cardiac magnetic resonance images. J Am Soc Echocardiogr 26:1267–1273. https://doi.org/10.1016/j.echo.2013.07.017
Dave JK, Mc Donald ME, Mehrotra P, Kohut AR, Eisenbrey JR, Forsberg F (2018) Recent technological advancements in cardiac ultrasound imaging. Ultrasonics 84:329–340. https://doi.org/10.1016/j.ultras.2017.11.013
Ouyang D, He B, Ghorbani A et al (2020) Video-based AI for beat-to-beat assessment of cardiac function. Nature 580:252–256. https://doi.org/10.1038/s41586-020-2145-8
He B, Kwan AC, Cho JH et al (2023) Blinded, randomized trial of sonographer versus AI cardiac function assessment. Nature 616:520–524. https://doi.org/10.1038/s41586-023-05947-3
Luong CL, Behnami D, Liao Z et al (2023) Machine learning derived echocardiographic image quality in patients with left ventricular systolic dysfunction: insights on the echo views of greatest image quality. Int J Cardiovasc Imaging 39:1313–1321. https://doi.org/10.1007/s10554-023-02802-4
Tromp J, Seekings PJ, Hung CL et al (2022) Automated interpretation of systolic and diastolic function on the echocardiogram: a multicohort study. Lancet Digit Health 4:e46–e54. https://doi.org/10.1016/S2589-7500(21)00235-1
Huang MS, Wang CS, Chiang JH, Liu PY, Tsai WC (2020) Automated recognition of regional wall motion abnormalities through deep neural network interpretation of transthoracic echocardiography. Circulation 142:1510–1520. https://doi.org/10.1161/CIRCULATIONAHA.120.047530
Duffy G, Cheng PP, Yuan N et al (2022) High-throughput precision phenotyping of left ventricular hypertrophy with cardiovascular deep learning. JAMA Cardiol 7:386–395. https://doi.org/10.1001/jamacardio.2021.6059
Goto S, Mahara K, Beussink-Nelson L et al (2021) Artificial intelligence-enabled fully automated detection of cardiac amyloidosis using electrocardiograms and echocardiograms. Nat Commun 12:2726. https://doi.org/10.1038/s41467-021-22877-8
Yuan N, Kwan AC, Duffy G et al (2023) Prediction of coronary artery calcium using deep learning of echocardiograms. J Am Soc Echocardiogr 36:474–481e3. https://doi.org/10.1016/j.echo.2022.12.014
Rajpurkar P, Chen E, Banerjee O, Topol EJ (2022) AI in health and medicine. Nat Med 28:31–38. https://doi.org/10.1038/s41591-021-01614-0
Kusunose K, Abe T, Haga A et al (2020) A deep learning approach for assessment of regional wall motion abnormality from echocardiographic images. JACC Cardiovasc Imaging 13:374–381. https://doi.org/10.1016/j.jcmg.2019.02.024
Jiang H, Sun D, Jampani V, Yang M-H, Learned-Miller E, Kautz J (2018) Super slomo: high quality estimation of multiple intermediate frames for video interpolation. In: Proceedings of the IEEE conference on computer vision and pattern recognition, p 9000–9008. https://doi.org/10.1109/CVPR.2018.00938
Pellikka PA, Arruda-Olson A, Chaudhry FA et al (2020) Guidelines for performance, interpretation, and application of stress echocardiography in Ischemic Heart Disease: from the American Society of Echocardiography. J Am Soc Echocardiogr 33:1–41e8. https://doi.org/10.1016/j.echo.2019.07.001
Cerqueira MD, Weissman NJ, Dilsizian V et al (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation 105:539–542. https://doi.org/10.1161/hc0402.102975
SenGupta PP, Shrestha S, Berthon B et al (2020) Proposed requirements for cardiovascular imaging-related machine learning evaluation (PRIME): a checklist: reviewed by the American College of Cardiology healthcare innovation council. JACC Cardiovasc Imaging 13:2017–2035. https://doi.org/10.1016/j.jcmg.2020.07.015
Bossuyt PM, Reitsma JB, Bruns DE et al (2003) Towards complete and accurate reporting of studies of diagnostic accuracy: the STARD initiative. BMJ 326:41–44. https://doi.org/10.1136/bmj.326.7379.41
Elhendy A, Mahoney DW, Khandheria BK, Paterick TE, Burger KN, Pellikka PA (2002) Prognostic significance of the location of wall motion abnormalities during exercise echocardiography. J Am Coll Cardiol 40:1623–1629. https://doi.org/10.1016/s0735-1097(02)02338-0
Tseng AS, Lopez-Jimenez F, Pellikka PA (2022) Future guidelines for artificial intelligence in echocardiography. J Am Soc Echocardiogr 35:878–882. https://doi.org/10.1016/j.echo.2022.04.005
Narang A, Bae R, Hong H et al (2021) Utility of a deep-learning algorithm to guide novices to acquire echocardiograms for limited diagnostic use. JAMA Cardiol 6:624–632. https://doi.org/10.1001/jamacardio.2021.0185
Hidalgo EM, Wright L, Isaksson M, Lambert G, Marwick TH (2023) Current applications of robot-assisted ultrasound examination. JACC Cardiovasc Imaging 16:239–247. https://doi.org/10.1016/j.jcmg.2022.07.018
Plana JC, Mikati IA, Dokainish H et al (2008) A randomized cross-over study for evaluation of the effect of image optimization with contrast on the diagnostic accuracy of dobutamine echocardiography in coronary artery Disease the OPTIMIZE Trial. JACC Cardiovasc Imaging 1:145–152. https://doi.org/10.1016/j.jcmg.2007.10.014
Acknowledgements
The authors thank all the participants (patients and in-hospital volunteers) in the study and the Division of Clinical Laboratory members in Gifu University.
Funding
This study was supported by the Physician Clinical Research grant from the Japanese Circulation Society (2021) and the 34th research grant from Fukuda Foundation for Medical Technology. (T.H) This work was partly supported by JST, CREST (JPMJCR21D4), Japan.
Author information
Authors and Affiliations
Contributions
Y.S, R.T, T.H, Takuma Ishihara and H.O had full access to all of the data of the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Concept and design: Y.S, T.W, T.H, and H.O. Acquisition, analysis, or interpretation of data: Y.S, A.S, Takeshi Ishihara, E.S, T.W, H.I, M.H and, H.O. Model development: R.T, D.F, and H.T. Drafting of the manuscript: Y.S. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: Takuma Ishihara, D.W. Obtained funding: Y.S. Supervision: T.H, H.O.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Writing support
We used the services of Editage® to perform English proofreading on the final manuscript. The proofreading was conducted to ensure the accuracy and clarity of the language used in the manuscript. We did not use any Generative AI services in the writing process. All content in this manuscript was written by the authors and was manually.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplemental Fig. 1
. Histogram showing the number of ischemic segments identified during exercise stress echocardiography among patients with regional wall motion abnormalities (n = 25).
Supplemental Fig. 2
. (A) The association between loss function and the number of epochs (training and validation dataset), and (B) the association between peak signal to noise ratio (PSNR) and the number of epochs (test dataset).
Supplemental table 1
. Proposed Requirements for Cardiovascular Imaging-Related Machine Learning Evaluation (PRIME) checklist.
Supplemental table 2
. The Standards for Reporting of Diagnostic Accuracy (STARD) checklist.
Supplemental Fig. 3
. Representative comparison between the control and slow-motion video images (0.25×, 0.125× speed) in a healthy volunteer (non-stress conventional echocardiography). Slow-motion echocardiography (for example, at 0.25×) is developed by quadrupling the number of images while maintaining the same fps.
Supplemental Fig. 4
. Representative comparison between the control and artificial intelligence-based slow-motion video images (0.25×, used in the diagnostic accuracy test) in both healthy volunteer and patients with regional wall motion abnormalities (post-myocardial infarction of diagonal artery).
Supplemental Fig. 5
. Randomly selected video images from four patients in test dataset showing that the trained model successfully created slow-motion echocardiography images among a wide range of cardiovascular patients.
Supplemental Fig. 6
. Representative echocardiograms showing that both videos with high fps and low fps were successfully converted to slow-motion echocardiography videos.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sahashi, Y., Takeshita, R., Watanabe, T. et al. Development of artificial intelligence-based slow-motion echocardiography and clinical usefulness for evaluating regional wall motion abnormalities. Int J Cardiovasc Imaging 40, 385–395 (2024). https://doi.org/10.1007/s10554-023-02997-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-023-02997-6