Abstract
Purpose
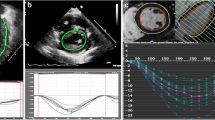
Cardiac Magnetic resonance (CMR) derived left ventricular longitudinal and circumferential strain is known to be abnormal in myocarditis. CMR strain is a useful additional tool that can identify subclinical myocardial involvement and may help with longitudinal follow-up. Right ventricular strain derived by CMR in children has not been studied. We sought to evaluate CMR derived biventricular strain in children with acute myocarditis.
Methods
Children with acute myocarditis who underwent CMR between 2016–2022 at our center were reviewed, this group included subjects with COVID-19 myocarditis. Children with no evidence of myocarditis served as controls Those with congenital heart disease and technically limited images for CMR strain analysis were excluded from final analysis. Biventricular longitudinal, circumferential, and radial peak systolic strains were derived using circle cvi42®. Data between cases and controls were compared using an independent sample t-test. One-way ANOVA with post hoc analysis was used to compare COVID-19, non-COVID myocarditis and controls.
Results
38 myocarditis and 14 controls met inclusion criteria (mean age 14.4 ± 3 years). All CMR derived peak strain values except for RV longitudinal strain were abnormal in myocarditis group. One-way ANOVA revealed that there was a statistically significant difference with abnormal RV and LV strain in COVID-19 myocarditis when compared to non-COVID-19 myocarditis and controls.
Conclusion
CMR derived right and left ventricular peak systolic strain using traditionally acquired cine images were abnormal in children with acute myocarditis. All strain measurements were significantly abnormal in children with COVID-19 even when compared to non-COVID myocarditis.



Similar content being viewed by others
Abbreviations
- CMR:
-
Cardiac Magnetic Resonance Imaging
- LV:
-
left ventricle
- RV:
-
right ventricle
- COVID-19:
-
Coronavirus disease
- MIS-C:
-
multisystem inflammatory syndrome in children
- ECG:
-
electrocardiogram
- CKMB:
-
creatine kinase myocardial band
- LGE:
-
late gadolinium enhancement
- EF:
-
ejection fraction
- BSA:
-
body surface area
- EDVi:
-
indexed end-diastolic volume
- SD:
-
standard deviation
- ms:
-
milliseconds
References
Williams JL, Jacobs HM, Lee S (2023) Pediatric Myocarditis. Cardiol Ther. https://doi.org/10.1007/s40119-023-00309-6
Ferreira VM, Schulz-Menger J, Holmvang G, Kramer CM, Carbone I, Sechtem U et al (2018) Cardiovascular magnetic resonance in nonischemic myocardial inflammation: expert recommendations. J Am Coll Cardiol 72:3158–3176. https://doi.org/10.1016/j.jacc.2018.09.072
Friedrich MG, Sechtem U, Schulz-Menger J, Holmvang G, Alakija P, Cooper LT et al (2009) Cardiovascular magnetic resonance in myocarditis: a JACC White Paper. J Am Coll Cardiol 53:1475–1487. https://doi.org/10.1016/j.jacc.2009.02.007
Law YM, Lal AK, Chen S, Čiháková D, Cooper LT, Deshpande S et al (2021) Diagnosis and management of myocarditis in children: a scientific statement from the american heart association. Circulation 144:e123–e135. https://doi.org/10.1161/CIR.0000000000001001
Weigand J, Nielsen JC, Sengupta PP, Sanz J, Srivastava S, Uppu S (2016) Feature tracking-derived peak systolic strain compared to late gadolinium enhancement in troponin-positive myocarditis: a case-control study. Pediatr Cardiol 37:696–703. https://doi.org/10.1007/s00246-015-1333-z
Howard A, Hasan A, Brownlee J, Mehmood N, Ali M, Mehta S et al (2020) Pediatric Myocarditis Protocol: an Algorithm for Early Identification and Management with Retrospective Analysis for Validation. Pediatr Cardiol 41:316–326. https://doi.org/10.1007/s00246-019-02258-1
Ali-Ahmed F, Dalgaard F, Al-Khatib SM (2020) Sudden cardiac death in patients with myocarditis: evaluation, risk stratification, and management. Am Heart J 220:29–40. https://doi.org/10.1016/j.ahj.2019.08.007
Shen WK, Edwards WD, Hammill SC, Bailey KR, Ballard DJ, Gersh BJ (1995) Sudden unexpected nontraumatic death in 54 young adults: a 30-year population-based study. Am J Cardiol 76:148–152. https://doi.org/10.1016/s0002-9149(99)80047-2
Banka P, Robinson JD, Uppu SC, Harris MA, Hasbani K, Lai WW et al (2015) Cardiovascular magnetic resonance techniques and findings in children with myocarditis: a multicenter retrospective study. J Cardiovasc Magn Reson 17:96. https://doi.org/10.1186/s12968-015-0201-6
Luetkens JA, Faron A, Isaak A, Dabir D, Kuetting D, Feisst A et al (2019) Comparison of original and 2018 lake louise criteria for diagnosis of acute myocarditis: results of a validation cohort. Radiology: Cardiothorac Imaging 1:e190010. https://doi.org/10.1148/ryct.2019190010
Gräni C, Eichhorn C, Bière L, Murthy VL, Agarwal V, Kaneko K et al (2017) Prognostic value of cardiac magnetic resonance tissue characterization in risk stratifying patients with suspected myocarditis. J Am Coll Cardiol 70:1964–1976. https://doi.org/10.1016/j.jacc.2017.08.050
Gräni C, Bière L, Eichhorn C, Kaneko K, Agarwal V, Aghayev A et al (2019) Incremental value of extracellular volume assessment by cardiovascular magnetic resonance imaging in risk stratifying patients with suspected myocarditis. Int J Cardiovasc Imaging 35:1067–1078. https://doi.org/10.1007/s10554-019-01552-6
Baccouche H, Mahrholdt H, Meinhardt G, Merher R, Voehringer M, Hill S et al (2009) Diagnostic synergy of non-invasive cardiovascular magnetic resonance and invasive endomyocardial biopsy in troponin-positive patients without coronary artery disease. Eur Heart J 30:2869–2879. https://doi.org/10.1093/eurheartj/ehp328
Mancio J, Bettencourt N, Oliveira M, Pires-Morais G, Ribeiro VG (2013) Acute right ventricular myocarditis presenting with chest pain and syncope. BMJ Case Rep. ;2013. https://doi.org/10.1136/bcr-2012-007173
Virk HUH, Munir MB (2015) Isolated right ventricular myocarditis: rarely reported pathology. Case Rep Cardiol 2015:790246. https://doi.org/10.1155/2015/790246
Abdin A, Trobo F, Chaffee R, Pietrolungo J (2017) A unique case of myocarditis causing isolated right ventricular dysfunction. Chest 152:A91. https://doi.org/10.1016/j.chest.2017.08.121
Ben Driss A, Laissy J-P (2021) Acute isolated right ventricular myocarditis: the importance of multimodality imaging. Circ Cardiovasc Imaging 14:e013046. https://doi.org/10.1161/CIRCIMAGING.121.013046
Aquaro GD, Negri F, De Luca A, Todiere G, Bianco F, Barison A et al (2018) Role of right ventricular involvement in acute myocarditis, assessed by cardiac magnetic resonance. Int J Cardiol 271:359–365. https://doi.org/10.1016/j.ijcard.2018.04.087
Luetkens JA, Petry P, Kuetting D, Dabir D, Schmeel FC, Homsi R et al (2018) Left and right ventricular strain in the course of acute myocarditis: a cardiovascular magnetic resonance study. Rofo 190:722–732. https://doi.org/10.1055/a-0585-0271
Leitman M, Lysyansky P, Sidenko S, Shir V, Peleg E, Binenbaum M et al (2004) Two-dimensional strain-a novel software for real-time quantitative echocardiographic assessment of myocardial function. J Am Soc Echocardiogr 17:1021–1029. https://doi.org/10.1016/j.echo.2004.06.019
Kempny A, Fernández-Jiménez R, Orwat S, Schuler P, Bunck AC, Maintz D et al (2012) Quantification of biventricular myocardial function using cardiac magnetic resonance feature tracking, endocardial border delineation and echocardiographic speckle tracking in patients with repaired tetralogy of Fallot and healthy controls. J Cardiovasc Magn Reson 14:32. https://doi.org/10.1186/1532-429X-14-32
Luetkens JA, Isaak A, Öztürk C, Mesropyan N, Monin M, Schlabe S et al (2021) Cardiac MRI in suspected Acute COVID-19 Myocarditis. Radiol Cardiothorac Imaging 3:e200628. https://doi.org/10.1148/ryct.2021200628
Ho JS, Sia C-H, Chan MY, Lin W, Wong RC (2020) Coronavirus-induced myocarditis: a meta-summary of cases. Heart Lung 49:681–685. https://doi.org/10.1016/j.hrtlng.2020.08.013
Esposito A, Palmisano A, Natale L, Ligabue G, Peretto G, Lovato L et al (2020) Cardiac magnetic resonance characterization of Myocarditis-Like Acute Cardiac Syndrome in COVID-19. JACC Cardiovasc Imaging 13:2462–2465. https://doi.org/10.1016/j.jcmg.2020.06.003
Huang L, Zhao P, Tang D, Zhu T, Han R, Zhan C et al (2020) Cardiac involvement in patients recovered from COVID-2019 identified using magnetic resonance imaging. JACC Cardiovasc Imaging 13:2330–2339. https://doi.org/10.1016/j.jcmg.2020.05.004
Kobayashi R, Dionne A, Ferraro A, Harrild D, Newburger J, VanderPluym C et al (2021) Detailed assessment of left ventricular function in multisystem inflammatory syndrome in children, using strain analysis. CJC Open 3:880–887. https://doi.org/10.1016/j.cjco.2021.02.012
Gibson LE, Fenza RD, Lang M, Capriles MI, Li MD, Kalpathy-Cramer J et al (2021) Right ventricular strain is common in intubated COVID-19 patients and does not reflect severity of respiratory illness. J Intensive Care Med 36:900–909. https://doi.org/10.1177/08850666211006335
Urmeneta Ulloa J, Martínez de Vega V, Salvador Montañés O, Álvarez Vázquez A, Sánchez-Enrique C, Hernández Jiménez S et al (2021) Cardiac magnetic resonance in recovering COVID-19 patients. Feature tracking and mapping analysis to detect persistent myocardial involvement. Int J Cardiol Heart Vasc 36:100854. https://doi.org/10.1016/j.ijcha.2021.100854
Tadic M, Pieske-Kraigher E, Cuspidi C, Morris DA, Burkhardt F, Baudisch A et al (2017) Right ventricular strain in heart failure: clinical perspective. Arch Cardiovasc Dis 110:562–571. https://doi.org/10.1016/j.acvd.2017.05.002
Geyer H, Caracciolo G, Abe H, Wilansky S, Carerj S, Gentile F et al (2010) Assessment of myocardial mechanics using speckle tracking echocardiography: fundamentals and clinical applications. J Am Soc Echocardiogr 23:351–369 quiz 453. https://doi.org/10.1016/j.echo.2010.02.015
Mendes LA, Dec GW, Picard MH, Palacios IF, Newell J, Davidoff R (1994) Right ventricular dysfunction: an independent predictor of adverse outcome in patients with myocarditis. Am Heart J 128:301–307. https://doi.org/10.1016/0002-8703(94)90483-9
Chen X, Hu H, Pan J, Shu J, Hu Y, Yu R (2020) Performance of cardiovascular magnetic resonance strain in patients with acute myocarditis. Cardiovasc Diagn Ther 10:725–737. https://doi.org/10.21037/cdt-20-221
Balaban Kocas B, Cetinkal G, Ser OS, Kilci H, Keskin K, Ozcan SN et al (2021) The relation between left ventricular global longitudinal strain and troponin levels in patients hospitalized with COVID-19 pneumonia. Int J Cardiovasc Imaging 37:125–133. https://doi.org/10.1007/s10554-020-02102-1
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Elisa Rhee, Harmanpreet Kaur and Santosh Uppu. Statistical analysis was performed by Julija Dobrila and Santosh Uppu. The first draft of the manuscript was written by Elisa Rhee and Santosh Uppu. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. Conference Presentation: Abstract was presented at the annual Society for Cardiovascular Magnetic Resonance conference February 2022.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved by The University of Texas Health Science Center at Houston and Memorial Hermann Institutional Review Board (HSC-MS-20-0153, March 9th, 2020) and waived the need for informed consent. All human studies at the University of Texas at Houston Health Science Center and Memorial Hermann hospital have to go through rigorous review by the ethics committee and have therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. The subjects were deidentified as per our IRB guidelines. Due to the retrospective nature, this study does not require contacting subjects as such a waiver of consent was requested and was approved by the IRB.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rhee, E., Dobrila, J., Kaur, H. et al. Right and left ventricular cardiac magnetic resonance imaging derived peak systolic strain is abnormal in children with myocarditis. Int J Cardiovasc Imaging 40, 139–147 (2024). https://doi.org/10.1007/s10554-023-02975-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-023-02975-y