Abstract
Purpose
We assessed the impact of bicuspid aortic valve (BAV), aortic stenosis (AS), and regurgitation (AR) on the metrics of left ventricular (LV) remodeling, as measured by electrocardiogram (ECG), transthoracic echocardiography (TTE), and cardiac magnetic resonance (CMR).
Methods
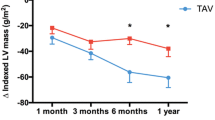
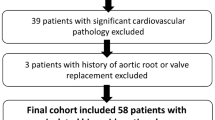
This retrospective CMR study included 11 patients with both AS and AR (BAV-ASR), 30 with AS (BAV-AS), 28 with AR (BAV-AR), 47 with neither AS nor AR (BAV-no_AS/AR), and 40 with trileaflet aortic valve (TAV-no_AS/AR). CMR analysis included the LV end-diastolic volume index (LVEDVi), mass index (LVMi), and extracellular volume fraction (ECV). The Sokolow-Lyon and Cornell products by ECG and TTE-derived E/e’ were measured.
Results
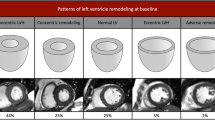
There were no differences in the ECG, TTE, and CMR parameters between BAV-no_AS/AR and TAV-no_AS/AR. However, the presence of aortic valve dysfunction resulted in an elevated Sokolow-Lyon product for BAV-ASR (p = 0.017) and BAV-AR (p = 0.001), as well as increased Cornell product (p = 0.04) and E/e’ (p < 0.001) for BAV-AS compared with BAV-no_AS/AR. LVEDVi and LVMi were elevated in patients with BAV-ASR and BAV-AR compared with those with BAV-no_AS/AR (LVEDVi: 101 ± 29 ml/m2 and 112 ± 32 ml/m2 vs. 74 ± 15 ml/m2, p = 0.005 and p < 0.001, LVMi: 75 ± 7 g/m2 and 64 ± 14 g/m2 vs. 47 ± 9 g/m2, respectively; p < 0.001). There was no difference in ECV between the BAV and TAV-no_AS/AR subgroups.
Conclusion
Normally functioning BAV did not result in LV remodeling. However, concomitant AV dysfunction was associated with statistically significant morphological remodeling.






Similar content being viewed by others
References
Siu SC, Silversides CK (2010) Bicuspid aortic valve disease. J Am Coll Cardiol 55:2789–2800. https://doi.org/10.1016/j.jacc.2009.12.068
Bonow RO, Carabello BA, Chatterjee K et al (2006) ACC/AHA 2006 guidelines for the management of patients with valvular heart disease: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to revise the 1998 guidelines for the management of patients with valvular heart disease) developed in collaboration with the Society of Cardiovascular Anesthesiologists endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. J Am Coll Cardiol 48:e1–e48
Campbell M (1968) Calcific aortic stenosis and congenital bicuspid aortic valves. Br Heart J 30:606–616. https://doi.org/10.1136/hrt.30.5.606
Roberts WC, Morrow AG, McIntosh CL, Jones M, Epstein SE (1981) Congenitally bicuspid aortic valve causing severe, pure aortic regurgitation without superimposed infective endocarditis. Analysis of 13 patients requiring aortic valve replacement. Am J Cardiol 47:206–209. https://doi.org/10.1016/0002-9149(81)90385-4
Sokolow M, Lyon TP (1949) The ventricular complex in left ventricular hypertrophy as obtained by unipolar precordial and limb leads. Am Heart J 37:161–186. https://doi.org/10.1016/0002-8703(49)90562-1
Okin PM, Roman MJ, Devereux RB, Kligfield P (1995) Electrocardiographic identification of increased left ventricular mass by simple voltage-duration products. J Am Coll Cardiol 25:417–423. https://doi.org/10.1016/0735-1097(94)00371-V
Nagueh SF, Middleton KJ, Kopelen HA, Zoghbi WA, Quiñones MA (1997) Doppler tissue imaging: A noninvasive technique for evaluation of left ventricular relaxation and estimation of filling pressures. J Am Coll Cardiol 30:1527–1533. https://doi.org/10.1016/S0735-1097(97)00344-6
Fernandes-Silva MM, Shah AM, Hegde S et al (2017) Race-related differences in left ventricular structural and functional remodeling in response to increased afterload: The ARIC study. JACC Heart Fail 5:157–165. https://doi.org/10.1016/j.jchf.2016.10.011
Mottram PM, Marwick TH (2005) Assessment of diastolic function: What the general cardiologist needs to know. Heart 91:681–695. https://doi.org/10.1136/hrt.2003.029413
Sado DM, Flett AS, Banypersad SM et al (2012) Cardiovascular magnetic resonance measurement of myocardial extracellular volume in health and disease. Heart 98:1436–1441. https://doi.org/10.1136/heartjnl-2012-302346
Kellman P, Wilson JR, Xue H, Ugander M, Arai AE (2012) Extracellular volume fraction mapping in the myocardium, part 1: Evaluation of an automated method. J Cardiovasc Magn Reson 14:63. https://doi.org/10.1186/1532-429X-14-63
Kellman P, Arai AE, Xue H (2013) T1 and extracellular volume mapping in the heart: Estimation of error maps and the influence of noise on precision. J Cardiovasc Magn Reson 15:56. https://doi.org/10.1186/1532-429X-15-56
Chin CWL, Everett RJ, Kwiecinski J et al (2017) Myocardial fibrosis and cardiac decompensation in aortic stenosis. JACC Cardiovasc Imaging 10:1320–1333. https://doi.org/10.1016/j.jcmg.2016.10.007
Chin CWL, Semple S, Malley T et al (2014) Optimization and comparison of myocardial T1 techniques at 3T in patients with aortic stenosis. Eur Heart J Cardiovasc Imaging 15:556–565. https://doi.org/10.1093/ehjci/jet245
Singh A, Horsfield MA, Bekele S et al (2015) Myocardial T1 and extracellular volume fraction measurement in asymptomatic patients with aortic stenosis: Reproducibility and comparison with age-matched controls. Eur Heart J Cardiovasc Imaging 16:763–770. https://doi.org/10.1093/ehjci/jev007
Gulati A, Jabbour A, Ismail TF et al (2013) Association of fibrosis with mortality and sudden cardiac death in patients with nonischemic dilated cardiomyopathy. JAMA 309:896–908. https://doi.org/10.1001/jama.2013.1363
Chan RH, Maron BJ, Olivotto I et al (2015) Significance of late gadolinium enhancement at right ventricular attachment to ventricular septum in patients with hypertrophic cardiomyopathy. Am J Cardiol 116:436–441. https://doi.org/10.1016/j.amjcard.2015.04.060
Sievers HH, Schmidtke C (2007) A classification system for the bicuspid aortic valve from 304 surgical specimens. J Thorac Cardiovasc Surg 133:1226–1233. https://doi.org/10.1016/j.jtcvs.2007.01.039
Mannacio V, Guadagno E, Mannacio L et al (2015) Comparison of left ventricular myocardial structure and function in patients with aortic stenosis and those with pure aortic regurgitation. Cardiology 132:111–118. https://doi.org/10.1159/000431283
Grotenhuis HB, Ottenkamp J, Westenberg JJM et al (2007) Reduced aortic elasticity and dilatation are associated with aortic regurgitation and left ventricular hypertrophy in nonstenotic bicuspid aortic valve patients. J Am Coll Cardiol 49:1660–1665. https://doi.org/10.1016/j.jacc.2006.12.044
Geiger J, Rahsepar AA, Suwa K et al (2018) 4D flow MRI, cardiac function, and T 1 -mapping: Association of valve-mediated changes in aortic hemodynamics with left ventricular remodeling. J Magn Reson Imaging 48:121–131. https://doi.org/10.1002/jmri.25916
Konno T, Nagata Y, Teramoto R et al (2016) Usefulness of electrocardiographic voltage to determine myocardial fibrosis in hypertrophic cardiomyopathy. Am J Cardiol 117:443–449. https://doi.org/10.1016/j.amjcard.2015.11.015
Hein S, Arnon E, Kostin S et al (2003) Progression from compensated hypertrophy to failure in the pressure-overloaded human heart: Structural deterioration and compensatory mechanisms. Circulation 107:984–991. https://doi.org/10.1161/01.CIR.0000051865.66123.B7
Elias N, Tarasoutchi F, Spina GS et al (2009) Myocardial fibrosis and ventricular remodeling in severe chronic aortic regurgitation. Arq Bras Cardiol 92:63–67. https://doi.org/10.1590/S0066-782X2009000100010
Park J, Chang HJ, Choi JH et al (2014) Late gadolinium enhancement in cardiac MRI in patients with severe aortic stenosis and preserved left ventricular systolic function is related to attenuated improvement of left ventricular geometry and filling pressure after aortic valve replacement. Korean Circ J 44:312–319. https://doi.org/10.4070/kcj.2014.44.5.312
Barone-Rochette G, Piérard S, De Ravenstein M et al (2014) Prognostic significance of LGE by CMR in aortic stenosis patients undergoing valve replacement. J Am Coll Cardiol 64:144–154. https://doi.org/10.1016/j.jacc.2014.02.612
Azevedo CF, Nigri M, Higuchi ML et al (2010) Prognostic significance of myocardial fibrosis quantification by histopathology and magnetic resonance imaging in patients with severe aortic valve disease. J Am Coll Cardiol 56:278–287. https://doi.org/10.1016/j.jacc.2009.12.074
Sparrow P, Messroghli DR, Reid S et al (2006) Myocardial T1 mapping for detection of left ventricular myocardial fibrosis in chronic aortic regurgitation: Pilot study. AJR Am J Roentgenol 187:W630–W635. https://doi.org/10.2214/AJR.05.1264
Inoue YY, Ambale-Venkatesh B, Mewton N et al (2017) Electrocardiographic impact of myocardial diffuse fibrosis and scar: MESA (Multi-Ethnic study of atherosclerosis). Radiology 282:690–698.
Funding
This work was supported by KAMIKAWA Foundation, JSPS KAKENHI (Grant number 20277353) and the National Institutes of Health (contract Grant numbers R01 HL115828 and K25 HL119608).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Kenichiro Suwa, Amir Ali Rahsepar, and Ahmadreza Ghasemiesfe. The first draft of the manuscript was written by Kenichiro Suwa. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This retrospective study was approved by the institutional review board.
Consent to participate
The patients were enrolled with an institutional review board-approved waiver of consent.
Consent to publish
The authors affirm that human research participants provided informed consent for publication of the images in Fig. 2.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Kenichiro Suwa and Amir Ali Rahsepar These authors contributed equally to this work.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Suwa, K., Rahsepar, A.A., Geiger, J. et al. A Left ventricle remodeling in patients with bicuspid aortic valve. Int J Cardiovasc Imaging 39, 391–399 (2023). https://doi.org/10.1007/s10554-022-02727-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-022-02727-4