Abstract
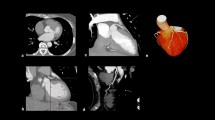
Signal intensity (SI) drop has been proposed as an indirect stenosis assessment in non-contrast coronary MRA (NC-MRCA) but it uses unproven assumptions. We aimed to clarify the mechanisms that govern the SI in vitro and develop a stenosis detection method in vivo. Flow phantom tubes with/without stenosis were scanned under two spatial resolutions (0.5/1.0 mm3) on a 3.0 T MRI. Thirty-two coronary arteries from 11 volunteers were prospectively scanned with an EKG- and respiratory-gated 3D NC-MRCA with a resolution of 1.0 mm3, with coronary computed tomography angiography (CTA) as reference. The normalized SI along the centerline of the tubes or the coronary arteries was assessed against the distance from the orifice using a linear regression model. Its coefficient (SI decay slope) and goodness-of-fit (R2) were extracted to assess the effect of flow velocity and stenosis on the SI profile curve. The R2 was utilized for the stenosis detection. Phantom study: A slow flow velocity caused a steep SI decay slope. The SI drop revealed only at the inlet and outlet of stenosis due to the flow turbulence/vortex and yielded low R2, in which shape changed by the resolution. Clinical study: The R2 cutoff to detect ≥ 50% stenosis for the left and right coronary arteries were 0.64 and 0.20 with a sensitivity/specificity of 71.5/71.5 and 66.7/100 (%), respectively. The SI drop did not reflect the actual stenosis position and not suitable for the stenosis localization. The R2 cutoff represents an alternative method to detect stenoses on NC-MRCA at vessel level.
Trial registration: ClinicalTrials.gov; NCT03768999, registered on December 7, 2018.





Similar content being viewed by others
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Benjamin EJ, Muntner P, Alonso A et al (2019) Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation 139:e56–e66. https://doi.org/10.1161/CIR.0000000000000659
Foley DP, Escaned J, Strauss BH et al (1994) Quantitative coronary angiography (QCA) in interventional cardiology: clinical application of QCA measurements. Prog Cardiovasc Dis 36:363–384. https://doi.org/10.1016/S0033-0620(05)80027-1
Miller JM, Rochitte CE, Dewey M et al (2008) Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med 359:2324–2336. https://doi.org/10.1056/NEJMoa0806576
Gulati M, Levy PD, Mukherjee D et al (2021) 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation 144:e368–e454. https://doi.org/10.1161/CIR.0000000000001029
Bech GJ, De Bruyne B, Pijls NH et al (2001) Fractional flow reserve to determine the appropriateness of angioplasty in moderate coronary stenosis: a randomized trial. Circulation 103:2928–2934. https://doi.org/10.1161/01.CIR.103.24.2928
Pijls NHJ, van Schaardenburgh P, Manoharan G et al (2007) Percutaneous coronary intervention of functionally nonsignificant stenosis: 5-year follow-up of the DEFER Study. J Am Coll Cardiol 49:2105–2111. https://doi.org/10.1016/j.jacc.2007.01.087
Tonino PAL, De Bruyne B, Pijls NHJ et al (2009) Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med 360:213–224. https://doi.org/10.1056/NEJMoa0807611
Rochitte CE, George RT, Chen MY et al (2014) Computed tomography angiography and perfusion to assess coronary artery stenosis causing perfusion defects by single photon emission computed tomography: the CORE320 study. Eur Heart J 35:1120–1130. https://doi.org/10.1093/eurheartj/eht488
Kishi S, Giannopoulos AA, Tang A et al (2018) Fractional flow reserve estimated at coronary CT angiography in intermediate lesions: comparison of diagnostic accuracy of different methods to determine coronary flow distribution. Radiology 287:76–84. https://doi.org/10.1148/radiol.2017162620
Lardo AC, Rahsepar AA, Seo JH et al (2015) Estimating coronary blood flow using CT transluminal attenuation flow encoding: formulation, preclinical validation, and clinical feasibility. J Cardiovasc Comput Tomogr 9:559–566. https://doi.org/10.1016/j.jcct.2015.03.018
Wong DTL, Ko BS, Cameron JD et al (2013) Transluminal attenuation gradient in coronary computed tomography angiography is a novel noninvasive approach to the identification of functionally significant coronary artery stenosis: a comparison with fractional flow reserve. J Am Coll Cardiol 61:1271–1279. https://doi.org/10.1016/j.jacc.2012.12.029
Choi JH, Min JK, Labounty TM et al (2011) Intracoronary transluminal attenuation gradient in coronary CT angiography for determining coronary artery stenosis. JACC Cardiovasc Imaging 4:1149–1157. https://doi.org/10.1016/j.jcmg.2011.09.006
Kato Y, Ambale-Venkatesh B, Kassai Y et al (2020) Non-contrast coronary magnetic resonance angiography: current frontiers and future horizons. MAGMA 33:591–612. https://doi.org/10.1007/s10334-020-00834-8
Hajhosseiny R, Bustin A, Munoz C et al (2020) Coronary magnetic resonance angiography: technical innovations leading us to the promised land? JACC Cardiovasc Imaging 13:2653–2672. https://doi.org/10.1016/j.jcmg.2020.01.006
Nakamura M, Kido T, Kido T et al (2018) Non-contrast compressed sensing whole-heart coronary magnetic resonance angiography at 3T: a comparison with conventional imaging. Eur J Radiol 104:43–48. https://doi.org/10.1016/j.ejrad.2018.04.025
Feng L, Coppo S, Piccini D et al (2018) 5D whole-heart sparse MRI. Magn Reson Med 79:826–838. https://doi.org/10.1002/mrm.26745
Haris K, Hedström E, Bidhult S et al (2017) Self-gated fetal cardiac MRI with tiny golden angle iGRASP: a feasibility study. J Magn Reson Imaging 46:207–217. https://doi.org/10.1002/jmri.25599
Pang J, Sharif B, Fan Z et al (2014) ECG and navigator-free four-dimensional whole-heart coronary MRA for simultaneous visualization of cardiac anatomy and function. Magn Reson Med 72:1208–1217. https://doi.org/10.1002/mrm.25450
Prieto C, Doneva M, Usman M et al (2015) Highly efficient respiratory motion compensated free-breathing coronary MRA using golden-step Cartesian acquisition. J Magn Reson Imaging 41:738–746. https://doi.org/10.1002/jmri.24602
Bastiaansen JAM, Piccini D, Di Sopra L et al (2020) Natively fat-suppressed 5D whole-heart MRI with a radial free-running fast-interrupted steady-state (FISS) sequence at 1.5T and 3T. Magn Reson Med 83:45–55. https://doi.org/10.1002/mrm.27942
Bastiaansen JAM, van Heeswijk RB, Stuber M, Piccini D (2019) Noncontrast free-breathing respiratory self-navigated coronary artery cardiovascular magnetic resonance angiography at 3 T using lipid insensitive binomial off-resonant excitation (LIBRE). J Cardiovasc Magn Reson 21:38. https://doi.org/10.1186/s12968-019-0543-6
Isogawa K, Ida T, Shiodera T, Takeguchi T (2018) Deep shrinkage convolutional neural network for adaptive noise reduction. IEEE Signal Process Lett 25:224–228. https://doi.org/10.1109/LSP.2017.2782270
Hajhosseiny R, Rashid I, Bustin A et al (2021) Clinical comparison of sub-mm high-resolution non-contrast coronary CMR angiography against coronary CT angiography in patients with low-intermediate risk of coronary artery disease: a single center trial. J Cardiovasc Magn Reson 23:1–14. https://doi.org/10.1186/s12968-021-00758-9
Nederkoorn PJ, Van der Graaf Y, Eikelboom BC et al (2002) Time-of-flight MR angiography of carotid artery stenosis: Does a flow void represent severe stenosis? Am J Neuroradiol 23:1779–1784
Heiserman JE, Zabramski JM, Drayer BP, Keller PJ (1996) Clinical significance of the flow gap in carotid magnetic resonance angiography. J Neurosurg 85:384–387. https://doi.org/10.3171/jns.1996.85.3.0384
Yonezawa M, Nagata M, Kitagawa K et al (2014) Quantitative analysis of 1.5-T whole-heart coronary MR angiograms obtained with 32-channel cardiac coils: a comparison with conventional quantitative coronary angiography. Radiology 271:356–364. https://doi.org/10.1148/radiol.13122491
Pennell DJ, Bogren HG, Keegan J et al (1996) Assessment of coronary artery stenosis by magnetic resonance imaging. Heart 75:127–133. https://doi.org/10.1136/hrt.75.2.127
Kidoh M, Shinoda K, Kitajima M et al (2019) Deep learning based noise reduction for brain MR imaging: tests on phantoms and healthy volunteers. Magn Reson Med Sci. https://doi.org/10.2463/mrms.mp.2019-0018
Kato Y, Ambale-venkatesh B, Kassai Y, et al (2019) Application of deep learning reconstruction for denoising of compressed sensing non-contrast coronary MRA images to achieve improved Diagnostic Confidence. ISMRM 2019 Abstr
Kato Y, Kapoor K, Ortman J, et al (2020) Comparison of Diagnostic Confidence score and calculation-based image quality scores on MRCA with different Compressed Sensing (CS) and Deep Learning Reconstruction (DLR) levels . SCMR 2020 Abstr
Heer T, Reiter S, Trißler M et al (2017) Effect of nitroglycerin on the performance of MR coronary angiography. J Magn Reson Imaging 45:1419–1428. https://doi.org/10.1002/jmri.25483
Parker DL, Yuan C, Blatter DD (1991) MR angiography by multiple thin slab 3D acquisition. Magn Reson Med 17:434–451. https://doi.org/10.1002/mrm.1910170215
Zhang Q, Chen Z, Chen S et al (2020) Angiographic contrast mechanism comparison between Simultaneous Non-contrast Angiography and intraPlaque hemorrhage (SNAP) sequence and Time of Flight (TOF) sequence for intracranial artery. Magn Reson Imaging 66:199–207. https://doi.org/10.1016/j.mri.2019.09.001
Dodge JT, Brown BG, Bolson EL, Dodge HT (1992) Lumen diameter of normal human coronary arteries: influence of age, sex, anatomic variation, and left ventricular hypertrophy or dilation. Circulation 86:232–246. https://doi.org/10.1161/01.CIR.86.1.232
Ofili EO, Labovitz AJ, Kern MJ (1993) Coronary flow velocity dynamics in normal and diseased arteries. Am J Cardiol. https://doi.org/10.1016/0002-9149(93)90128-Y
Steigner ML, Mitsouras D, Whitmore AG et al (2010) Iodinated contrast opacification gradients in normal coronary arteries imaged with prospectively ECG-gated single heart beat 320-detector row computed tomography. Circ Cardiovasc Imaging 3:179–186. https://doi.org/10.1161/CIRCIMAGING.109.854307
Park EA, Lee W, Park SJ et al (2016) Influence of coronary artery diameter on intracoronary transluminal attenuation gradient during CT angiography. JACC Cardiovasc Imaging 9:1074–1083. https://doi.org/10.1016/j.jcmg.2015.10.028
Park E-A, Lee W (2016) The authors reply. JACC Cardiovasc Imaging 9:1360–1361. https://doi.org/10.1016/j.jcmg.2016.09.008
Sharif D, Sharif-Rasslan A, Shahla C et al (2015) Differences in coronary artery blood velocities in the setting of normal coronary angiography and normal stress echocardiography. Heart Int 10:e6–e11. https://doi.org/10.5301/heartint.5000221
Anderson HV, Stokes MJ, Leon M et al (2000) Coronary artery flow velocity is related to lumen area and regional left ventricular mass. Circulation 102:48–54. https://doi.org/10.1161/01.CIR.102.1.48
Mahalingam A, Gawandalkar UU, Kini G et al (2016) Numerical analysis of the effect of turbulence transition on the hemodynamic parameters in human coronary arteries. Cardiovasc Diagn Ther 6:208–220. https://doi.org/10.21037/cdt.2016.03.08
Acknowledgements
The authors thank Jaclyn Sesso, our research nurse, for the participant recruitment and for providing care for the participants; Jennifer Wagner, our research collaborator from Canon Medical Systems, for supporting the MRI scans; Karan Kapoor, our cardiologist, for attending the clinical MRI scans; and Ryan Stewart, our collaborator from Johns Hopkins Biomedical Engineering, for 3D-printing the phantom. This study was supported by Canon Medical Systems Corporation, grant # 16–00632.
Funding
This study was supported by Canon Medical Systems Corporation, grant # 16–00632.
Author information
Authors and Affiliations
Contributions
Each author’s contribution was as follows: YK: Conceptualization, methodology, formal analysis, investigation, data curation, writing- draft, writing-review and editing. CN: Investigation, writing- review and editing. BA-V: Conceptualization, writing-review and editing. JMO: Investigation, resources, writing-review and editing. YK: Software, resources, writing-review and editing. JACL: Supervision, writing-review and editing. C-YL: Conceptualization, methodology, investigation, supervision, writing-review and editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
Conflicts of interest/Competing interests: This work represents ongoing R&D between our group at Johns Hopkins Hospital and Canon Medical Systems. This study was supported by Canon Medical Systems Corporation, grant # 16–00632. Dr. Lima is the recipient of the grant. Drs Kassai and Liu are Canon Medical Systems employees in research and development roles, are members of the joint research group. We have been particularly careful at eliminating any perception of bias. Other co-authors have no conflict of interest. The authors have full control of all primary data and agree to allow the journal to review the data if requested.
Conflicts of interest
This work represents ongoing R&D between our group at Johns Hopkins Hospital and Canon Medical Systems. This study was supported by Canon Medical Systems Corporation, grant # 16–00632. Dr. Lima is the recipient of the grant. Drs Kassai and Liu are Canon Medical Systems employees in research and development roles, are members of the joint research group. We have been particularly careful at eliminating any perception of bias. Other co-authors have no conflict of interest. The authors have full control of all primary data and agree to allow the journal to review the data if requested.
Ethical approval
The study complied with the World Medical Association's Declaration of Helsinki. This study is registered with ClinicalTrials.gov, number NCT03768999. The Johns Hopkins School of Medicine institutional review board (IRB) approved the study protocol on Feb 17, 2020 with application number IRB00196000.
Consent to participate
Informed consent to participate was obtained from all individual participants included in the study.
Consent to publish
Informed consent for publication was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kato, Y., Noda, C., Ambale-Venkatesh, B. et al. The mechanisms of arterial signal intensity profile in non-contrast coronary MRA (NC-MRCA): a 3D printed phantom investigation and clinical translations. Int J Cardiovasc Imaging 39, 209–220 (2023). https://doi.org/10.1007/s10554-022-02700-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-022-02700-1