Abstract
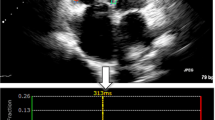
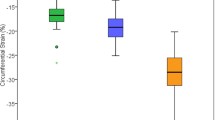
3-Dimensional (3D) myocardial deformation analysis (3D-MDA) enables novel descriptions of geometry-independent principal strain (PS). Applied to routine 2D cine cardiovascular magnetic resonance (CMR), this provides unique measures of myocardial biomechanics for disease diagnosis and prognostication. However, healthy reference values remain undefined. This study describes age- and sex-stratified reference values from CMR-based 3D-MDA, including 3D PS. One hundred healthy volunteers were prospectively recruited following institutional ethics approval and underwent CMR imaging. 3D-MDA was performed using validated software. Age- and sex-stratified global and segmental strain measures were derived for conventional geometry-dependent [circumferential (CS), longitudinal (LS), and radial (RS)] and geometry-independent [minimum (minPS) and maximum principal (maxPS)] directions of deformation. Layer-specific contraction angle interactions were determined using local minPS vectors. The average age was 43 ± 15 years and 55% were women. Strain measures were higher in women versus men. 3D PS-based assessment of maximum tissue shortening (minPS) and maximum tissue thickening (maxPS) were greater than corresponding geometry-dependent markers of LS and RS, consistent with improved representation of local tissue deformations. Global maxPS amplitude best discriminated both age and sex. Segmental analyses showed greater strain amplitudes in apical segments. Transmural PS contraction angles were higher in females and showed a heterogeneous distribution across segments. In this study we provided age and sex-based reference values for 3D strain from CMR imaging, demonstrating improved capacity for 3D PS to document maximal local tissue deformations and to discriminate age and sex phenotypes. Novel markers of layer-specific strain angles from 3D PS were also described.








Similar content being viewed by others
Abbreviations
- 2D:
-
Two-dimensional
- 3D MDA:
-
Three-dimensional myocardial deformation analysis
- AHA:
-
American Heart Association
- ANOVA:
-
Analysis of variance
- BMI:
-
Body mass index
- CMR:
-
Cardiac magnetic resonance imaging
- DSR:
-
Diastolic strain rate
- EF:
-
Ejection fraction
- GCS:
-
Global circumferential strain
- GLS:
-
Global longitudinal strain
- GRS:
-
Global radial strain
- LV:
-
Left ventricle
- maxPS:
-
Maximum principal strain
- minPS:
-
Minimum principal strain
- RV:
-
Right ventricle
- SSR:
-
Systolic strain rate
- TRIBECA:
-
Transmural interplay between contraction angles
- TTP:
-
Time to peak
References
Pagourelias ED, Mirea O, Duchenne J, Van Cleemput J, Delforge M, Bogaert J, Kuznetsova T, Voigt JU (2017) Echo parameters for differential diagnosis in cardiac amyloidosis: a head-to-head comparison of deformation and nondeformation parameters. Circulation 10(3):1–11. https://doi.org/10.1161/CIRCIMAGING.116.005588
Pun SC, Landau HJ, Riedel ER, Jordan J, Yu AF, Hassoun H, Chen CL, Steingart RM, Liu JE (2018) Prognostic and added value of two-dimensional global longitudinal strain for prediction of survival in patients with light chain amyloidosis undergoing autologous hematopoietic cell transplantation. J Am Soc Echocardiogr 31(1):64–70. https://doi.org/10.1016/j.echo.2017.08.017
Lei C, Zhu X, Hsi DH, Wang J, Zuo L, Ta S, Yang Q, Xu L, Zhao X, Wang Y, Sun S, Liu L (2021) Predictors of cardiac involvement and survival in patients with primary systemic light-chain amyloidosis: roles of the clinical, chemical, and 3-D speckle tracking echocardiography parameters. BMC Cardiovasc Disord 21(1):43. https://doi.org/10.1186/s12872-021-01856-3
Vollema EM, Amanullah MR, Prihadi EA, Ng ACT, van der Bijl P, Sin YK, Ajmone Marsan N, Ding ZP, Généreux P, Leon MB, Ewe SH, Delgado V, Bax JJ (2020) Incremental value of left ventricular global longitudinal strain in a newly proposed staging classification based on cardiac damage in patients with severe aortic stenosis. Eur Heart J 21(11):1248–1258. https://doi.org/10.1093/ehjci/jeaa220
Uziębło-Życzkowska B, Mielniczuk M, Ryczek R, Krzesiński P (2020) Myocarditis successfully diagnosed and controlled with speckle tracking echocardiography. Cardiovasc Ultrasound 18(1):19. https://doi.org/10.1186/s12947-020-00203-4
Di Stefano C, Bruno G, Arciniegas Calle MC, Acharya GA, Fussner LM, Ungprasert P, Cooper LT, Blauwet LA, Ryu JH, Pellikka PA, Carmona Porquera EM, Villarraga HR (2020) Diagnostic and predictive value of speckle tracking echocardiography in cardiac sarcoidosis. BMC Cardiovasc Disord 20(1):21. https://doi.org/10.1186/s12872-019-01323-0
Potter E, Marwick TH (2018) Assessment of left ventricular function by echocardiography. JACC 11(2):260–274. https://doi.org/10.1016/j.jcmg.2017.11.017
Sperry BW, Sato K, Phelan D, Grimm R, Desai MY, Hanna M, Jaber WA, Popović ZB (2019) Regional variability in longitudinal strain across vendors in patients with cardiomyopathy due to increased left ventricular wall thickness. Circulation. https://doi.org/10.1161/CIRCIMAGING.119.008973
Amzulescu MS, Langet H, Saloux E, Manrique A, Slimani A, Allain P, Roy C, de Meester C, Pasquet A, Somphone O, De Craene M, Vancraeynest D, Pouleur A-C, Vanoverschelde J-L, Gerber BL (2018) Improvements of myocardial deformation assessment by three-dimensional speckle-tracking versus two-dimensional speckle-tracking revealed by cardiac magnetic resonance tagging. J Am Soc Echocardiogr 31(9):1021-1033.e1. https://doi.org/10.1016/j.echo.2018.04.009
Kawel-Boehm N, Maceira A, Valsangiacomo-Buechel ER, Vogel-Claussen J, Turkbey EB, Williams R, Plein S, Tee M, Eng J, Bluemke DA (2015) Normal values for cardiovascular magnetic resonance in adults and children. J Cardiovasc Magn Reson 17(1):1–33. https://doi.org/10.1186/s12968-015-0111-7
Peng J, Zhao X, Zhao L, Fan Z, Wang Z, Chen H, Leng S, Allen J, Tan R-S, Koh AS, Ma X, Lou M, Zhong L (2018) Normal values of myocardial deformation assessed by cardiovascular magnetic resonance feature tracking in a healthy Chinese population: a multicenter study. Front Physiol. https://doi.org/10.3389/fphys.2018.01181
Augustine D, Lewandowski AJ, Lazdam M, Rai A, Francis J, Myerson S, Noble A, Becher H, Neubauer S, Petersen SE, Leeson P (2013) Global and regional left ventricular myocardial deformation measures by magnetic resonance feature tracking in healthy volunteers: comparison with tagging and relevance of gender. J Cardiovasc Magn Reson 15(1):8. https://doi.org/10.1186/1532-429X-15-8
Stanton T, Leano R, Marwick TH (2009) Prediction of all-cause mortality from global longitudinal speckle strain. Circulation 2(5):356–364. https://doi.org/10.1161/CIRCIMAGING.109.862334
Tops LF, Delgado V, Marsan NA, Bax JJ (2017) Myocardial strain to detect subtle left ventricular systolic dysfunction. Eur J Heart Fail 19(3):307–313. https://doi.org/10.1002/ejhf.694
Kalam K, Otahal P, Marwick TH (2014) Prognostic implications of global LV dysfunction: a systematic review and meta-analysis of global longitudinal strain and ejection fraction. Heart 100(21):1673–1680. https://doi.org/10.1136/heartjnl-2014-305538
Pedrizzetti G, Sengupta S, Caracciolo G, Park CS, Amaki M, Goliasch G, Narula J, Sengupta PP (2014) Three-dimensional principal strain analysis for characterizing subclinical changes in left ventricular function. J Am Soc Echocardiogr 27(10):1041-1050.e1. https://doi.org/10.1016/j.echo.2014.05.014
Tanabe Y, Kido T, Kurata A, Sawada S, Suekuni H, Kido T, Yokoi T, Uetani T, Inoue K, Miyagawa M, Mochizuki T (2017) Three-dimensional maximum principal strain using cardiac computed tomography for identification of myocardial infarction. Eur Radiol. https://doi.org/10.1007/s00330-016-4550-9
Kaku K, Takeuchi M, Tsang W, Takigiku K, Yasukochi S, Patel AR, Mor-Avi V, Lang RM, Otsuji Y (2014) Age-related normal range of left ventricular strain and torsion using three-dimensional speckle-tracking echocardiography. J Am Soc Echocardiogr 27(1):55–64. https://doi.org/10.1016/j.echo.2013.10.002
Xia J, Xia J, Li G, Ma W, Wang Q (2014) Left ventricular strain examination of different aged adults with 3D speckle tracking echocardiography. Echocardiography 31(3):335–339. https://doi.org/10.1111/echo.12367
Muraru D, Cucchini U, Mihăilă S, Miglioranza MH, Aruta P, Cavalli G, Cecchetto A, Padayattil-Josè S, Peluso D, Iliceto S, Badano LP (2014) Left Ventricular myocardial strain by three-dimensional speckle-tracking echocardiography in healthy subjects: reference values and analysis of their physiologic and technical determinants. J Am Soc Echocardiogr 27(8):858-871.e1. https://doi.org/10.1016/j.echo.2014.05.010
Kleijn SA, Pandian NG, Thomas JD, Perez de Isla L, Kamp O, Zuber M, Nihoyannopoulos P, Forster T, Nesser H-J, Geibel A, Gorissen W, Zamorano JL (2015) Normal reference values of left ventricular strain using three-dimensional speckle tracking echocardiography: results from a multicentre study. Eur Heart J 16(4):410–416. https://doi.org/10.1093/ehjci/jeu213
Bernard A, Addetia K, Dulgheru R, Caballero L, Sugimoto T, Akhaladze N, Athanassopoulos GD, Barone D, Baroni M, Cardim N, Hagendorff A, Hristova K, Ilardi F, Lopez T, de la Morena G, Popescu BA, Penicka M, Ozyigit T, Carbonero DR, van de Veire N, Stephan Von Bardeleben R, Vinereanu D, Luis Zamorano J, Martinez C, Magne J, Cosyns B, Donal E, Habib G, Badano LP, Lang RM, Lancellotti P (2017) 3D echocardiographic reference ranges for normal left ventricular volumes and strain: results from the EACVI NORRE study. Eur Heart J 18(4):475–483. https://doi.org/10.1093/ehjci/jew284
Kovács Z, Kormányos Á, Domsik P, Kalapos A, Lengyel C, Ambrus N, Ajtay Z, Piros GÁ, Forster T, Nemes A (2019) Left ventricular longitudinal strain is associated with mitral annular fractional area change in healthy subjects—results from the three-dimensional speckle tracking echocardiographic MAGYAR-Healthy Study. Quant Imaging Med Surg 9(2):304–311. https://doi.org/10.21037/qims.2019.02.06
Ajmone Marsan N, Michalski B, Cameli M, Podlesnikar T, Manka R, Sitges M, Dweck MR, Haugaa KH (2020) EACVI survey on standardization of cardiac chambers quantification by transthoracic echocardiography. Eur Heart J 21(2):119–123. https://doi.org/10.1093/ehjci/jez297
Satriano A, Heydari B, Narous M, Exner DV, Mikami Y, Attwood MM, Tyberg JV, Lydell CP, Howarth AG, Fine NM, White JA (2017) Clinical feasibility and validation of 3D principal strain analysis from cine MRI: comparison to 2D strain by MRI and 3D speckle tracking echocardiography. Int J Cardiovasc Imaging 33(12):1979–1992. https://doi.org/10.1007/s10554-017-1199-7
Avitzur N, Satriano A, Afzal M, Narous M, Mikami Y, Hansen R, Dobko G, Flewitt J, Lydell CP, Howarth AG, Chow K, Fine NM, White JA (2018) 3D myocardial deformation analysis from cine MRI as a marker of amyloid protein burden in cardiac amyloidosis: validation versus T1 mapping. Int J Cardiovasc Imaging 34(12):1937–1946. https://doi.org/10.1007/s10554-018-1410-5
Todd A, Satriano A, Fenwick K, Merchant N, Lydell CP, Howarth AG, Friedrich MG, Anderson TJ, Fine NM, White JA (2019) Intra-thoracic adiposity is associated with impaired contractile function in patients with coronary artery disease: a cardiovascular magnetic resonance imaging study. Int J Cardiovasc Imaging. https://doi.org/10.1007/s10554-018-1430-1
Satriano A, Heydari B, Guron N, Fenwick K, Cheung M, Mikami Y, Merchant N, Lydell CP, Howarth AG, Fine NM, White JA (2019) 3-Dimensional regional and global strain abnormalities in hypertrophic cardiomyopathy. Int J Cardiovasc Imaging. https://doi.org/10.1007/s10554-019-01631-8
Satriano A, Vigmond EJ, Schwartzman DS, Di Martino ES (2018) Mechano-electric finite element model of the left atrium. Comput Biol Med 96:24–31. https://doi.org/10.1016/j.compbiomed.2018.02.010
Satriano A, Afzal Y, Sarim Afzal M, Fatehi Hassanabad A, Wu C, Dykstra S, Flewitt J, Feuchter P, Sandonato R, Heydari B, Merchant N, Howarth AG, Lydell CP, Khan A, Fine NM, Greiner R, White JA (2020) Neural-network-based diagnosis using 3-dimensional myocardial architecture and deformation: demonstration for the differentiation of hypertrophic Cardiomyopathy. Front Cardiovasc Med. https://doi.org/10.3389/fcvm.2020.584727
Schulz-Menger J, Bluemke DA, Bremerich J, Flamm SD, Fogel MA, Friedrich MG, Kim RJ, von Knobelsdorff-Brenkenhoff F, Kramer CM, Pennell DJ, Plein S, Nagel E (2020) Standardized image interpretation and post-processing in cardiovascular magnetic resonance - 2020 update. J Cardiovasc Magn Reson 22(1):19. https://doi.org/10.1186/s12968-020-00610-6
Carminati MC, Maffessanti F, Caiani EG (2014) Nearly automated motion artifacts correction between multi breath-hold short-axis and long-axis cine CMR images. Comput Biol Med 46(1):42–50. https://doi.org/10.1016/j.compbiomed.2013.12.013
Haber I, Metaxas DN, Axel L (2000) Three-dimensional motion reconstruction and analysis of the right ventricle using tagged MRI. Med Image Anal 4(4):335–355. https://doi.org/10.1016/S1361-8415(00)00028-1
Oregan DP, Shi W, Ariff B, Baksi AJ, Durighel G, Rueckert D, Cook SA (2012) Remodeling after acute myocardial infarction: mapping ventricular dilatation using three dimensional CMR image registration. J Cardiovasc Magn Reson 14(1):1–9. https://doi.org/10.1186/1532-429X-14-41
Young A, Axel L (1992) Non-rigid heart wall motion using MR tagging. In: Proceedings of the IEEE computer society conference on computer vision and pattern recognition, vol 1992, pp. 399–404
Hallquist JO (n.d.) LS-Dyna theory manual, vol 19. Livermore Software Technology Corporation, Ed.
Bonet J, Wood RD (2008) Nonlinear continuum mechanics for finite element analysis. Nonlinear continuum mechanics for finite element analysis, vol 9780521838, 2nd edn. Cambridge University Press, Cambridge
Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, Pennell DJ, Rumberger JA, Ryan T, Verani MS (2002) Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart. A statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Int J Cardiovasc Imaging 18(1):539–542. https://doi.org/10.1067/mje.2002.123374
Tavakoli V, Sahba N (2013) Assessment of age-related changes in left ventricular twist by 3-dimensional speckle-tracking echocardiography. J Ultrasound Med 32(8):1435–1441. https://doi.org/10.7863/ultra.32.8.1435
Amzulescu MS, De Craene M, Langet H, Pasquet A, Vancraeynest D, Pouleur AC, Vanoverschelde JL, Gerber BL (2019) Myocardial strain imaging: review of general principles, validation, and sources of discrepancies. Eur Heart J 20(6):605–619. https://doi.org/10.1093/ehjci/jez041
Truong VT, Phan HT, Pham KNP, Duong HNH, Ngo TNM, Palmer C, Nguyen TTH, Truong BH, Vo MA, Tretter JT, Nagueh SF, Chung ES, Mazur W (2019) Normal ranges of left ventricular strain by three-dimensional speckle-tracking echocardiography in adults: a systematic review and meta-analysis. J Am Soc Echocardiogr 32(12):1586-1597.e5. https://doi.org/10.1016/j.echo.2019.07.012
Nabeshima Y, Seo Y, Takeuchi M (2020) A review of current trends in three-dimensional analysis of left ventricular myocardial strain. Cardiovasc Ultrasound. https://doi.org/10.1186/s12947-020-00204-3
Liu B, Dardeer AM, Moody WE, Hayer MK, Baig S, Price AM, Leyva F, Edwards NC, Steeds RP (2017) Reference ranges for three-dimensional feature tracking cardiac magnetic resonance: comparison with two-dimensional methodology and relevance of age and gender. Int J Cardiovasc Imaging. https://doi.org/10.1007/s10554-017-1277-x
Satriano A, Guenther Z, White JA, Merchant N, Di Martino ES, Al-Qoofi F, Lydell CP, Fine NM (2018) Three-dimensional thoracic aorta principal strain analysis from routine ECG-gated computerized tomography: feasibility in patients undergoing transcatheter aortic valve replacement. BMC Cardiovasc Disord 18(1):1–11. https://doi.org/10.1186/s12872-018-0818-0
Satriano A, Pournazari P, Hirani N, Helmersen D, Thakrar M, Weatherald J, White JA, Fine NM (2018) Characterization of right ventricular deformation in pulmonary arterial hypertension using three-dimensional principal strain analysis. J Am Soc Echocardiogr. https://doi.org/10.1016/j.echo.2018.10.001
Addetia K, Muraru D, Badano LP, Lang RM (2019) New directions in right ventricular assessment using 3-dimensional echocardiography. JAMA Cardiol. https://doi.org/10.1001/jamacardio.2019.2424
Tsugu T, Postolache A, Dulgheru R, Sugimoto T, Tridetti J, Nguyen Trung M-L, Piette C, Moonen M, Manganaro R, Ilardi F, Chitroceanu AM, Sperlongano S, Go YY, Kacharava G, Athanassopoulos GD, Barone D, Baroni M, Cardim N, Hagendorff A, Hristova K, Lopez T, de la Morena G, Popescu BA, Penicka M, Ozyigit T, Rodrigo Carbonero JD, van de Veire N, Von Bardeleben RS, Vinereanu D, Zamorano JL, Rosca M, Calin A, Magne J, Cosyns B, Galli E, Donal E, Santoro C, Galderisi M, Badano LP, Lang RM, Lancellotti P (2020) Echocardiographic reference ranges for normal left ventricular layer-specific strain: results from the EACVI NORRE study. Eur Heart J 21(8):896–905. https://doi.org/10.1093/ehjci/jeaa050
Kawel-Boehm N, Hetzel SJ, Ambale-Venkatesh B, Captur G, Francois CJ, Jerosch-Herold M, Salerno M, Teague SD, Valsangiacomo-Buechel E, van der Geest RJ, Bluemke DA (2020) Reference ranges (“normal values”) for cardiovascular magnetic resonance (CMR) in adults and children: 2020 update. J Cardiovasc Magn Reson 22(1):87. https://doi.org/10.1186/s12968-020-00683-3
Wang TKM, Kwon DH, Griffin BP, Flamm SD, Popović ZB (2020) Defining the reference range for left ventricular strain in healthy patients by cardiac MRI measurement techniques: systematic review and meta-analysis. Am J Roentgenol. https://doi.org/10.2214/AJR.20.24264
Santoro C, Arpino G, Esposito R, Lembo M, Paciolla I, Cardalesi C, de Simone G, Trimarco B, De Placido S, Galderisi M (2017) 2D and 3D strain for detection of subclinical anthracycline cardiotoxicity in breast cancer patients: a balance with feasibility. Eur Heart J 18(8):930–936. https://doi.org/10.1093/ehjci/jex033
Lawton JS, Cupps BP, Knutsen AK, Ma N, Brady BD, Reynolds LM, Pasque MK (2011) Magnetic resonance imaging detects significant sex differences in human myocardial strain. Biomed Eng Online 10(1):76. https://doi.org/10.1186/1475-925X-10-76
Andre F, Steen H, Matheis P, Westkott M, Breuninger K, Sander Y, Kammerer R, Galuschky C, Giannitsis E, Korosoglou G, Katus HA, Buss SJ (2015) Age- and gender-related normal left ventricular deformation assessed by cardiovascular magnetic resonance feature tracking. J Cardiovasc Magn Reson 17(1):25. https://doi.org/10.1186/s12968-015-0123-3
Taylor RJ, Moody WE, Umar F, Edwards NC, Taylor TJ, Stegemann B, Townend JN, Hor KN, Steeds RP, Mazur W, Leyva F (2015) Myocardial strain measurement with feature-tracking cardiovascular magnetic resonance: normal values. Eur Heart J 16(8):871–881. https://doi.org/10.1093/ehjci/jev006
Mangion K, Clerfond G, McComb C, Carrick D, Rauhalammi SM, McClure J, Corcoran DS, Woodward R, Orchard V, Radjenovic A, Zhong X, Berry C (2016) Myocardial strain in healthy adults across a broad age range as revealed by cardiac magnetic resonance imaging at 1.5 and 3.0T: associations of myocardial strain with myocardial region, age, and sex. J Magn Reson Imaging 44(5):1197–1205. https://doi.org/10.1002/jmri.25280
Stefani L, De Luca A, Toncelli L, Pedrizzetti G, Galanti G (2014) 3D Strain helps relating LV function to LV and structure in athletes. Cardiovasc Ultrasound. https://doi.org/10.1186/1476-7120-12-33
Pedrizzetti G, Kraigher-Krainer E, De Luca A, Caracciolo G, Mangual JO, Shah A, Toncelli L, Domenichini F, Tonti G, Galanti G, Sengupta PP, Narula J, Solomon S (2012) Functional strain-line pattern in the human left ventricle. Phys Rev Lett. https://doi.org/10.1103/PhysRevLett.109.048103
Marwan M, Ammon F, Bittner D, Röther J, Mekkhala N, Hell M, Schuhbaeck A, Gitsioudis G, Feyrer R, Schlundt C, Achenbach S, Arnold M (2018) CT-derived left ventricular global strain in aortic valve stenosis patients: a comparative analysis pre and post transcatheter aortic valve implantation. J Cardiovasc Comput Tomogr. https://doi.org/10.1016/j.jcct.2018.01.010
Al Saikhan L, Park C, Hughes AD (2019) Reproducibility of left ventricular dyssynchrony indices by three-dimensional speckle-tracking echocardiography: the impact of sub-optimal image quality. Front Cardiovasc Med. https://doi.org/10.3389/fcvm.2019.00149
Evangelista A, Gabriele S, Nardinocchi P, Piras P, Puddu PE, Teresi L, Torromeo C, Varano V (2015) Non-invasive assessment of functional strain lines in the real human left ventricle via speckle tracking echocardiography. J Biomech. https://doi.org/10.1016/j.jbiomech.2014.12.028
Yoshida K, Tanabe Y, Kido T, Kurata A, Uraoka D, Kinoshita M, Uetani T, Nishimura K, Inoue K, Ikeda S, Yamaguchi O, Mochizuki T (2020) Characteristics of the left ventricular three-dimensional maximum principal strain using cardiac computed tomography: reference values from subjects with normal cardiac function. Eur Radiol. https://doi.org/10.1007/s00330-020-07001-6
Barbosa D, Claus P, Choi HF, Hristova K, Loeckx D, D’Hooge J (2009) An in-vivo study on the difference between principal and cardiac strains. Proc IEEE Ultrasonics Symp. https://doi.org/10.1109/ULTSYM.2009.5441819
Suzuki M, Uetani T, Aono J, Nagai T, Nishimura K, Inoue K, Suzuki J, Higaki J, Ikeda S (2017) Impact of three-dimensional maximum principal strain using cardiac computed tomography in aortic stenosis. J Cardiac Fail. https://doi.org/10.1016/j.cardfail.2017.08.402
Omar HA, Domingos JS, Patra A, Upton R, Leeson P, Noble JA (2018) Quantification of cardiac bull’s-eye map based on principal strain analysis for myocardial wall motion assessment in stress echocardiography. In: Proceedings—international symposium on biomedical imaging, vol 2018-April. https://doi.org/10.1109/ISBI.2018.8363785
Zhang KW, Finkelman BS, Gulati G, Narayan HK, Upshaw J, Narayan V, Plappert T, Englefield V, Smith AM, Zhang C, Hundley WG, Ky B (2018) Abnormalities in 3-dimensional left ventricular mechanics with anthracycline chemotherapy are associated with systolic and diastolic dysfunction. JACC 11(8):1059–1068. https://doi.org/10.1016/j.jcmg.2018.01.015
Labib D, Satriano A, Dykstra S, Hansen R, Mikami Y, Guzzardi D, Slavikova Z, Feutcher P, Flewitt J, Rivest S, Sandonato R, Lydell C, Howarth A, Kolman L, Clarke B, Paterson I, Oudit G, Pituskin E, Cheung W, Lee J, White JA (2021) The effect of active cancer on the cardiac phenotype: a cardiac MRI-based study of myocardial tissue health and deformation in chemotherapy-Naïve patients. J Am Heart Assoc (in press).
Gabriele S, Nardinocchi P, Varano V (2015) Evaluation of the strain-line patterns in a human left ventricle: a simulation study. Comput Methods Biomech Biomed Eng. https://doi.org/10.1080/10255842.2013.847094
Fonseca CG, Dissanayake AM, Doughty RN, Whalley GA, Gamble GD, Cowan BR, Occleshaw CJ, Young AA (2004) Three-dimensional assessment of left ventricular systolic strain in patients with type 2 diabetes mellitus, diastolic dysfunction, and normal ejection fraction. Am J Cardiol. https://doi.org/10.1016/j.amjcard.2004.07.143
Venkatesh BA, Schiros CG, Gupta H, Lloyd SG, Dell’Italia L, Denney TS (2011) Three-dimensional plus time biventricular strain from tagged MR images by phase-unwrapped harmonic phase. J Magn Reson Imaging. https://doi.org/10.1002/jmri.22665
Ghelani SJ, Brown DW, Kuebler JD, Perrin D, Shakti D, Williams DN, Marx GR, Colan SD, Geva T, Harrild DM (2018) Left atrial volumes and strain in healthy children measured by three-dimensional echocardiography: normal values and maturational changes. J Am Soc Echocardiogr. https://doi.org/10.1016/j.echo.2017.10.011
Wong KCL, Tee M, Chen M, Bluemke DA, Summers RM, Yao J (2016) Regional infarction identification from cardiac CT images: a computer-aided biomechanical approach. Int J Comput Assist Radiol Surg. https://doi.org/10.1007/s11548-016-1404-5
Hess AT, Zhong X, Spottiswoode BS, Epstein FH, Meintjes EM (2009) Myocardial 3D strain calculation by combining cine Displacement Encoding with Stimulated Echoes (DENSE) and cine strain encoding (SENC) imaging. Magn Reson Med 62(1):77–84. https://doi.org/10.1002/mrm.21984
Neizel M, Lossnitzer D, Korosoglou G, Schäufele T, Peykarjou H, Steen H, Ocklenburg C, Giannitsis E, Katus HA, Osman NF (2009) Strain-encoded MRI for evaluation of left ventricular function and transmurality in acute myocardial infarction. Circulation 2(2):116–122. https://doi.org/10.1161/CIRCIMAGING.108.789032
Shi J, Pan C, Kong D, Cheng L, Shu X (2016) Left ventricular longitudinal and circumferential layer-specific myocardial strains and their determinants in healthy subjects. Echocardiography 33(4):510–518. https://doi.org/10.1111/echo.13132
Nagata Y, Wu VC-C, Otsuji Y, Takeuchi M (2017) Normal range of myocardial layer-specific strain using two-dimensional speckle tracking echocardiography. PLoS ONE 12(6):e0180584. https://doi.org/10.1371/journal.pone.0180584
Omar AMS, Vallabhajosyula S, Sengupta PP (2015) Left ventricular twist and torsion. Circulation. https://doi.org/10.1161/CIRCIMAGING.115.003029
Goffinet C, Chenot F, Robert A, Pouleur A-C, de Waroux J-B, Vancrayenest D, Gerard O, Pasquet A, Gerber BL, Vanoverschelde J-L (2009) Assessment of subendocardial vs subepicardial left ventricular rotation and twist using two-dimensional speckle tracking echocardiography: comparison with tagged cardiac magnetic resonance. Eur Heart J 30(5):608–617. https://doi.org/10.1093/eurheartj/ehn511
Ozawa K, Funabashi N, Takaoka H, Kamata T, Kanaeda A, Saito M, Nomura F, Kobayashi Y (2015) Characteristic myocardial strain identified in hypertrophic cardiomyopathy subjects with preserved left ventricular ejection fraction using a novel multi-layer transthoracic echocardiography technique. Int J Cardiol 184:237–243. https://doi.org/10.1016/j.ijcard.2015.01.070
Ozawa K, Funabashi N, Kobayashi Y (2016) Left ventricular myocardial strain gradient using a novel multi-layer transthoracic echocardiography technique positively correlates with severity of aortic stenosis. Int J Cardiol 221:218–226. https://doi.org/10.1016/j.ijcard.2016.06.275
Xu L, Pagano JJ, Haykowksy MJ, Ezekowitz JA, Oudit GY, Mikami Y, Howarth A, White JA, Dyck JRB, Anderson T, Paterson DI, Thompson RB (2020) Layer-specific strain in patients with heart failure using cardiovascular magnetic resonance: not all layers are the same. J Cardiovasc Magn Reson 22(1):81. https://doi.org/10.1186/s12968-020-00680-6
Sarvari SI, Haugaa KH, Zahid W, Bendz B, Aakhus S, Aaberge L, Edvardsen T (2013) Layer-specific quantification of myocardial deformation by strain echocardiography may reveal significant CAD in patients with non–ST-segment elevation acute coronary syndrome. JACC 6(5):535–544. https://doi.org/10.1016/j.jcmg.2013.01.009
Neubauer S, Kolm P, Ho CY, Kwong RY, Desai MY, Dolman SF, Appelbaum E, Desvigne-Nickens P, DiMarco JP, Friedrich MG, Geller N, Harper AR, Jarolim P, Jerosch-Herold M, Kim DY, Maron MS, Schulz-Menger J, Piechnik SK, Thomson K, Zhang C, Watkins H, Weintraub WS, Kramer CM (2019) Distinct subgroups in hypertrophic cardiomyopathy in the NHLBI HCM registry. J Am Coll Cardiol 74(19):2333–2345. https://doi.org/10.1016/j.jacc.2019.08.1057
D’Ascenzi F, Solari M, Mazzolai M, Cameli M, Lisi M, Andrei V, Focardi M, Bonifazi M, Mondillo S (2016) Two-dimensional and three-dimensional left ventricular deformation analysis: a study in competitive athletes. Int J Cardiovasc Imaging 32(12):1697–1705. https://doi.org/10.1007/s10554-016-0961-6
Guedes H, Moreno N, dos Santos RP, Marques L, Seabra D, Pereira A, Andrade A, Pinto P (2018) Importance of three-dimensional speckle tracking in the assessment of left atrial and ventricular dysfunction in patients with myotonic dystrophy type 1. Rev Port Cardiol 37(4):333–338. https://doi.org/10.1016/j.repc.2017.10.011
Fang X, Pan C, Chen Y, Sun M, Zhang Z, Jiang L, Wang X, Shu X (2017) Assessment of subclinical left ventricular changes in essential hypertensive patients with hyperuricemia: a three-dimensional speckle-tracking echocardiography study. Clin Exp Hypertens 39(1):93–99. https://doi.org/10.1080/10641963.2016.1210626
Acknowledgements
The authors thank Dr. Gianni Pedrizzetti for his assistance with the graphical representation of principal directions.
Funding
This study was funded in part by the Canadian Institutes for Health Research (CIHR, Project# 10020327).
Author information
Authors and Affiliations
Contributions
AS and JAW contributed to conception and design of the study. AS is developer of the 3D MDA software. DG contributed to data analysis and writing the manuscript. DL performed 3D MDA analysis. SD contributed to data analysis. JF provided study coordination. PF performed MR scans. RS contributed to recruitment. AGH, CPL, NMF, and RG contributed to critical manuscript revision. All authors provided approval for publication of the manuscript.
Corresponding author
Ethics declarations
Competing interest
JAW receives research support from Siemens Healthineers, Circle Cardiovascular Inc, and Pfizer Inc. and is chief medical officer and a shareholder of Cohesic Inc. AGH is a shareholder of Cohesic Inc. AS is a shareholder in and receives consulting fees from Vitaa Medical Solutions Inc.
Consent to publish
Not applicable.
Ethical approval and consent to participate
The study design was approved by the Conjoint Health Research Ethics Board at the University of Calgary and all subjects provided written informed consent. All research activities were performed in accordance with the Declaration of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Guzzardi, D.G., White, J.A., Labib, D. et al. Normative healthy reference values for global and segmental 3D principal and geometry dependent strain from cine cardiac magnetic resonance imaging. Int J Cardiovasc Imaging 39, 115–134 (2023). https://doi.org/10.1007/s10554-022-02693-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-022-02693-x