Abstract
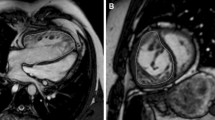
Treatment of D- transposition of great arteries (DTGA) involves the Arterial Switch Operation (ASO), which can create PA branch stenosis (PABS) and alter PA blood flow energetics. This altered PA flow may contribute to elevated right ventricular (RV) afterload more significantly than stenosis alone. Our aim was to correlate RV afterload and PA flow characteristics using 4D flow cardiac magnetic resonance (CMR) imaging of a mock circulatory system (MCS) incorporating 3D printed replicas. CMR imaging and clinical characteristics were analyzed from 22 ASO patients (age 11.9 ± 8.7 years, 68% male). Segmentation was performed to create 3D printed PA replicas that were mounted in an MRI-compatible MCS. Pressure drop across the PA replica was recorded and 4D flow CMR acquisitions were analyzed for blood flow inefficiency (energy loss, vorticity). In post-ASO patients, there is no difference in RV mass (p = 0.07), nor RV systolic pressure (p = 0.26) in the presence or absence of PABS. 4D flow analysis of MCS shows energy loss is correlated to RV mass (p = 0.01, r = 0.67) and MCS pressure differential (p = 0.02, r = 0.57). Receiver operating characteristic curve shows energy loss detects elevated RV mass above 30 g/m2 (p = 0.02, AUC 0.88) while index of PA dimensions (Nakata) does not (p = 0.09, AUC 0.79). PABS alone does not account for differences in RV mass or afterload in post-ASO patients. In MCS simulations, energy loss is correlated with both RV mass and PA pressure, and can moderately detect elevated RV mass. Inefficient PA flow may be an important predictor of RV afterload in this population.





Similar content being viewed by others
Data availability
The datasets generated and analyzed during the current study are not publicly available in order to protect subject anonymity, but are available from the corresponding author on reasonable request.
References
Reller MD, Strickland MJ, Riehle-Colarusso T, Mahle WT, Correa A (2008) Prevalence of congenital heart defects in metropolitan Atlanta, 1998–2005. J Pediatr 153:807–813
Gerberding J, Snider D, Popović T, Solomon S (2006) Improved national prevalence estimates for 18 selected major birth defects—United States, 1999–2001. MMWR Morb Mortal Wkly Rep 54:1301–5
Hutter P, Kreb D, Mantel S, Hitchcock J, Meijboom E, Bennink G (2002) Twenty-five years’ experience with the arterial switch operation. J Thorac Cardiovasc Surg 124:790–797
Hörer J, Schreiber C, Cleuziou J, Vogt M, Prodan Z, Busch R, Holper K, Lange R (2009) Improvement in long-term survival after hospital discharge but not in freedom from reoperation after the change from atrial to arterial switch for transposition of the great arteries. J Thorac Cardiovasc Surg 137:347–354
Prêtre R, Tamisier D, Bonhoeffer P, Mauriat P, Pouard P, Sidi D, Vouhé P (2001) Results of the arterial switch operation in neonates with transposed great arteries. The Lancet 357:1826–1830
Jatene A, Fontes VF, Paulista P, Souza L, Neger F, Galantier M, Sousa J (1976) Anatomic correction of transposition of the great vessels. J Thorac Cardiovasc Surg 72:364–370
Kirzner J, Pirmohamed A, Ginns J, Singh HS (2018) Long-term management of the arterial switch patient. Curr Cardiol Rep 20:68
Klitsie LM, Roest AA, Kuipers IM, Hazekamp MG, Blom NA, Ten Harkel AD (2014) Left and right ventricular performance after arterial switch operation. J Thorac Cardiovasc Surg 147:1561–1567
Grotenhuis HB, Kroft LJ, van Elderen SG, Westenberg JJ, Doornbos J, Hazekamp MG, Vliegen HW, Ottenkamp J, de Roos A (2007) Right ventricular hypertrophy and diastolic dysfunction in arterial switch patients without pulmonary artery stenosis. Heart 93:1604–1608
Loke Y-H, Capuano F, Mandell J, Cross RR, Cronin I, Mass P, Balaras E, Olivieri LJ (2019) Abnormal pulmonary artery bending correlates with increased right ventricular afterload following the arterial switch operation. World J Pediatr Congenit Heart Surg 10:572–581
Capuano F, Loke Y-H, Cronin I, Olivieri LJ, Balaras E (2019) Computational study of pulmonary flow patterns after repair of transposition of great arteries. J Biomechan Eng 141:051008
Morgan CT, Mertens L, Grotenhuis H, Yoo SJ, Seed M, Grosse-Wortmann L (2017) Understanding the mechanism for branch pulmonary artery stenosis after the arterial switch operation for transposition of the great arteries. Eur Heart J Cardiovasc Imaging 18:180–185
Khairy P, Clair M, Fernandes SM, Blume ED, Powell AJ, Newburger JW, Landzberg MJ, Mayer JE (2013) Cardiovascular outcomes after the arterial switch operation for D-transposition of the great arteries. Circulation 127:331–339
Geiger J, Hirtler D, Bürk J, Stiller B, Arnold R, Jung B, Langer M, Markl M (2014) Postoperative pulmonary and aortic 3D haemodynamics in patients after repair of transposition of the great arteries. Eur Radiol 24:200–208
Ntsinjana HN, Capelli C, Biglino G, Cook AC, Tann O, Derrick G, Taylor AM, Schievano S (2014) 3D morphometric analysis of the arterial switch operation using in vivo MRI data. Clin Anat 27:1212–1222
Breinholt JP, John S (2019) Management of the adult with arterial switch. Methodist Debakey Cardiovasc J 15:133
Tang T, Chiu S, Chen H-C, Cheng K-Y, Chen S-J (2001) Comparison of pulmonary arterial flow phenomena in spiral and Lecompte models by computational fluid dynamics. J Thorac Cardiovasc Surg 122:529–534
Yan W, Li J, Wang W, Wei L, Wang S (2021) A fluid-structure interaction study of different bicuspid aortic valve phenotypes throughout the cardiac cycle. Front Physiol 12:716015
Olivieri LJ, de Zélicourt DA, Haggerty CM, Ratnayaka K, Cross RR, Yoganathan AP (2011) Hemodynamic modeling of surgically repaired coarctation of the aorta. Cardiovasc Eng Technol 2:288–295
Fratz S, Chung T, Greil GF, Samyn MM, Taylor AM, Valsangiacomo Buechel ER, Yoo SJ, Powell AJ (2013) Guidelines and protocols for cardiovascular magnetic resonance in children and adults with congenital heart disease: SCMR expert consensus group on congenital heart disease. J Cardiovasc Magnetic Reson 15:51
Olivieri LJ, Jiang J, Hamann K, Loke YH, Campbell-Washburn A, Xue H, McCarter R, Cross R (2020) Normal right and left ventricular volumes prospectively obtained from cardiovascular magnetic resonance in awake, healthy, 0–12 year old children. J Cardiovasc Magnetic Reson 22:11
Knobel Z, Kellenberger CJ, Kaiser T, Albisetti M, Bergsträsser E, Buechel ER (2011) Geometry and dimensions of the pulmonary artery bifurcation in children and adolescents: assessment in vivo by contrast-enhanced MR-angiography. Int J Cardiovasc Imaging 27:385–396
Nakata S, Imai Y, Takanashi Y, Kurosawa H, Tezuka K, Nakazawa M, Ando M, Takao A (1984) A new method for the quantitative standardization of cross-sectional areas of the pulmonary arteries in congenital heart diseases with decreased pulmonary blood flow. J Thorac Cardiovasc Surg 88:610–619
Karaca-Altintas Y, Laux D, Gouton M, Bensemlali M, Roussin R, Hörer J, Raisky O, Bonnet D (2020) Nakata index above 1500 mm2/m2 predicts death in absent pulmonary valve syndrome. Eur J Cardio-Thoracic Surg 57:46–53
Sandoval JP, Chaturvedi RR, Benson L, Morgan G, Van Arsdell G, Honjo O, Caldarone C, Lee KJ (2016) Right ventricular outflow tract stenting in tetralogy of fallot infants with risk factors for early primary repair. Circ Cardiovasc interv. https://doi.org/10.1161/CIRCINTERVENTIONS.116.003979
Yeung E, Inoue T, Matsushita H, Opfermann J, Mass P, Aslan S, Johnson J, Nelson K, Kim B, Olivieri L, Krieger A, Hibino N (2020) In vivo implantation of 3-dimensional printed customized branched tissue engineered vascular graft in a porcine model. J Thorac Cardiovasc Surg 159:1971-1981.e1
Mandell JG, Loke YH, Mass PN, Opfermann J, Cleveland V, Aslan S, Hibino N, Krieger A, Olivieri LJ (2020) Aorta size mismatch predicts decreased exercise capacity in patients with successfully repaired coarctation of the aorta. J Thorac Cardiovasc Surg. https://doi.org/10.1016/j.jtcvs.2020.09.103
Knoops PG, Biglino G, Hughes AD, Parker KH, Xu L, Schievano S, Torii R (2017) A mock circulatory system incorporating a compliant 3d-printed anatomical model to investigate pulmonary hemodynamics. Artif Organs 41:637–646
Zambrano BA, McLean NA, Zhao X, Tan JL, Zhong L, Figueroa CA, Lee LC, Baek S (2018) Image-based computational assessment of vascular wall mechanics and hemodynamics in pulmonary arterial hypertension patients. J Biomech 68:84–92
Canstein C, Cachot P, Faust A, Stalder A, Bock J, Frydrychowicz A, Küffer J, Hennig J, Markl M (2008) 3D MR flow analysis in realistic rapid-prototyping model systems of the thoracic aorta: comparison with in vivo data and computational fluid dynamics in identical vessel geometries. Magn Reson Med 59:535–546
Biglino G, Giardini A, Baker C, Figliola RS, Hsia T-Y, Taylor AM, Schievano S (2012) In vitro study of the Norwood palliation: a patient-specific mock circulatory system. ASAIO J 58:25–31
Nyns EC, Dragulescu A, Yoo SJ, Grosse-Wortmann L (2016) Evaluation of knowledge-based reconstruction for magnetic resonance volumetry of the right ventricle after arterial switch operation for dextro-transposition of the great arteries. Int J Cardiovasc Imaging 32:1415–1423
Vonk-Noordegraaf A, Haddad F, Chin KM, Forfia PR, Kawut SM, Lumens J, Naeije R, Newman J, Oudiz RJ, Provencher S, Torbicki A, Voelkel NF, Hassoun PM (2013) Right heart adaptation to pulmonary arterial hypertension: physiology and pathobiology. J Am Coll Cardiol 62:D22-33
Thattaliyath BD, Forsha DE, Stewart C, Barker PC, Campbell MJ (2015) Evaluation of right ventricular myocardial mechanics using velocity vector imaging of cardiac MRI cine images in transposition of the great arteries following atrial and arterial switch operations. Congenit Heart Dis 10:371–379
Sanz J, Sánchez-Quintana D, Bossone E, Bogaard HJ, Naeije R (2019) Anatomy, function, and dysfunction of the right ventricle: JACC state-of-the-art review. J Am Coll Cardiol 73:1463–1482
Ou P, Celermajer DS, Jolivet O, Buyens F, Herment A, Sidi D, Bonnet D, Mousseaux E (2008) Increased central aortic stiffness and left ventricular mass in normotensive young subjects after successful coarctation repair. Am Heart J 155:187–193
Dawes TJ, Gandhi A, de Marvao A, Buzaco R, Tokarczuk P, Quinlan M, Durighel G, Diamond T, Monje Garcia L, de Cesare A, Cook SA, O’Regan DP (2016) Pulmonary artery stiffness is independently associated with right ventricular mass and function: a cardiac MR imaging study. Radiology 280:398–404
Aziz KU, Nanton MA, Kidd L, Moes CA, Rowe RD (1976) Variation in the size and distensibility of the pulmonary arteries in d-transposition of the great arteries. Am J Cardiol 38:452–457
Murakami T, Nakanishi T, Nakazawa M, Momma K, Imai Y (1998) The spectrum of pulmonary input impedance in children with complete transposition after the arterial switch operation. Cardiol Young 8:180–186
Yu CM, Sanderson JE, Chan S, Yeung L, Hung YT, Woo KS (1996) Right ventricular diastolic dysfunction in heart failure. Circulation 93:1509–1514
Liu X, Sun A, Fan Y, Deng X (2015) Physiological significance of helical flow in the arterial system and its potential clinical applications. Ann Biomed Eng 43:3–15
Bächler P, Pinochet N, Sotelo J, Crelier G, Irarrazaval P, Tejos C, Uribe S (2013) Assessment of normal flow patterns in the pulmonary circulation by using 4D magnetic resonance velocity mapping. Magn Reson Imaging 31:178–188
Capuano F, Loke Y-H, Balaras E (2019) Blood flow dynamics at the pulmonary artery bifurcation. Fluids 4:190
Riesenkampff E, Nordmeyer S, Al-Wakeel N, Kropf S, Kutty S, Berger F, Kuehne T (2014) Flow-sensitive four-dimensional velocity-encoded magnetic resonance imaging reveals abnormal blood flow patterns in the aorta and pulmonary trunk of patients with transposition. Cardiol Young 24:47–53
Rickers C, Kheradvar A, Sievers HH, Falahatpisheh A, Wegner P, Gabbert D, Jerosch-Herold M, Hart C, Voges I, Putman LM, Kristo I, Fischer G, Scheewe J, Kramer HH (2016) Is the Lecompte technique the last word on transposition of the great arteries repair for all patients? A magnetic resonance imaging study including a spiral technique two decades postoperatively. Interact Cardiovasc Thorac Surg 22:817–825
Villafañe J, Lantin-Hermoso MR, Bhatt AB, Tweddell JS, Geva T, Nathan M, Elliott MJ, Vetter VL, Paridon SM, Kochilas L (2014) D-transposition of the great arteries: the current era of the arterial switch operation. J Am Coll Cardiol 64:498–511
Fricke TA, d’Udekem Y, Richardson M, Thuys C, Dronavalli M, Ramsay JM, Wheaton G, Grigg LE, Brizard CP, Konstantinov IE (2012) Outcomes of the arterial switch operation for transposition of the great arteries: 25 years of experience. Ann Thorac Surg 94:139–145
Vukicevic M, Chiulli JA, Conover T, Pennati G, Hsia TY, Figliola RS (2013) Mock circulatory system of the Fontan circulation to study respiration effects on venous flow behavior. ASAIO J 59:253–60
Biglino G, Verschueren P, Zegels R, Taylor AM, Schievano S (2013) Rapid prototyping compliant arterial phantoms for in-vitro studies and device testing. J Cardiovasc Magn Reson 15:2
de Zélicourt DA, Pekkan K, Wills L, Kanter K, Forbess J, Sharma S, Fogel M, Yoganathan AP (2005) In vitro flow analysis of a patient-specific intraatrial total cavopulmonary connection. Ann Thorac Surg 79:2094–2102
Gehron J, Zirbes J, Bongert M, Schäfer S, Fiebich M, Krombach G, Böning A, Grieshaber P (2019) Development and validation of a life-sized mock circulatory loop of the human circulation for fluid-mechanical studies. ASAIO J 65:788–797
Acknowledgements
The authors would like to acknowledge Nicholas Mouzakis, the cardiovascular magnetic resonance technologist for assistance in scanning in vitro experiments.
Funding
This project was supported by Award Number R38AI140298 from the NIH National Center of Allergy and Infectious Diseases. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Center of Allergy and Infectious Diseases or the National Institutes of Health.
Author information
Authors and Affiliations
Contributions
VC and PM made substantial contributions to experiment execution and engineering iterative design. FC provided technical oversight and guidance in optimizing patient-specific parameters of experimental setup. YL, JM, and LO provided scientific guidance and cardiology imaging expertise throughout and directly contributed to the study conception and execution. LO also served as the primary mentor and principal investigator for this research and contributed significantly to manuscript editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interests.
Ethical approval
This study was approved by the Children’s National Hospital Institutional Review Board.
Consent for publication
Not applicable, as no individual-level data has been presented in this manuscript.
Consent for publication
Not applicable, as no individual-level data has been presented in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Delaney, M., Cleveland, V., Mass, P. et al. Right ventricular afterload in repaired D-TGA is associated with inefficient flow patterns, rather than stenosis alone. Int J Cardiovasc Imaging 38, 653–662 (2022). https://doi.org/10.1007/s10554-021-02436-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-021-02436-4