Abstract
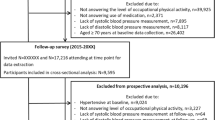
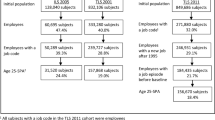
To investigate cross-sectional associations between heavy occupational lifting and cardiac structure and function. Participants from the 5th round of the Copenhagen City Heart Study, aged < 65 years old, answering a questionnaire regarding occupational physical activity, heavy occupational lifting, use of anti-hypertensive and heart medication, and data on blood pressure, cardiac structure and function, from an echocardiographic examination, were included. Adjusted linear regressions and logistic regressions were applied to estimate the cross-sectional association between heavy occupational lifting and cardiac structure and function across all included participants and in groups stratified by hypertension status, and the risk for having abnormal values of cardiac structure and function. 2511 participants were included. The cross-sectional standardized associations between heavy occupational lifting and measures of cardiac structure and function showed a trends for raised left ventricular mass index (LVMi) (β 0.14, 99% CI − 0.03 to 0.31). The standardized associations stratified by hypertensive status showed significant associations between exposure to heavy occupational lifting and LVMi (β 0.20, 99% CI − 0.002 to 0.40) and a trend of a raised end-diastolic interventricular septal thickness (IVSd) (β 0.15, 99% CI − 0.03 to 0.33) among normotensives. Exposure to heavy occupational lifting increased the odds for an abnormal IVSd (OR 1.42, 99% CI 1.07–1.89). This cross-sectional study shows heavy occupational lifting to associate with indices of abnormal cardiac structure and function among normotensives, indicating an increased risk for cardiovascular disease.


Similar content being viewed by others
Availability of data and material
Requests for data should be applied to the steering group for the Copenhagen City Heart Study, which can be reached by contact to either Peter Schnohr or Jacob Louis Marott.
Code availability
Availability of coding for the statistical analysis can be delivered by request to Mette Korshøj.
References
Coenen P, Huysmans MA, Holtermann A, Krause N, Van Mechelen W, Straker LM et al (2018) Do highly physically active workers die early? A systematic review with meta-analysis of data from 193 696 participants. Br J Sports Med 52(20):1320–1326
Kristensen TS (1989) Cardiovascular diseases and the work environment. A critical review of the epidemiologic literature on nonchemical factors. Scand J Work Environ Health 15(3):165–79
Holtermann A, Krause N, van der Beek AJ, Straker L (2018) The physical activity paradox: six reasons why occupational physical activity (OPA) does not confer the cardiovascular health benefits that leisure time physical activity does. Br J Sports Med 52(3):149–150. https://doi.org/10.1136/bjsports-2017-097965
MacDougall JD, Tuxen D, Sale DG, Moroz JR, Sutton JR (1985) Arterial blood pressure response to heavy resistance exercise. J Appl Physiol 58(3):785–90
Clays E, De BD, Van HK, De BG, Kittel F, Holtermann A (2012) Occupational and leisure time physical activity in contrasting relation to ambulatory blood pressure. BMCPublic Health 12:1002
Fransson E, De FU, Ahlbom A, Reuterwall C, Hallqvist J, Alfredsson L (2004) The risk of acute myocardial infarction: interactions of types of physical activity. Epidemiology 15(5):573–582
Nde F, Nebo J, Ngatchou W, Tchatchoua C, Sone AM, De Brouwer C (2014) Impact of heavy load activity on cardiovascular system: echocardiographic assessment of informal construction workers heart in Cameroon. Pan Afr Med J 17:79
Pedersen LR, Kristensen AMD, Petersen SS, Vaduganathan M, Bhatt DL, Juel J et al (2020) Prognostic implications of left ventricular hypertrophy diagnosed on electrocardiogram vs echocardiography. J Clin Hypertens 22(9):1647–1658
Cain PA, Ahl R, Hedstrom E, Ugander M, Allansdotter-Johnsson A, Friberg P et al (2007) Physiological determinants of the variation in left ventricular mass from early adolescence to late adulthood in healthy subjects. Clin Physiol Funct Imaging 27(4):254–262
Gyimes Z, Pavlik G, Simor T (2004) Morphological and functional differences in cardiac parameters between power and endurance athletes: a magnetic resonance imaging study. Acta Physiol Hung 91(1):49–57
Saltin B, Grimby G (1968) Physiological analysis of middle-aged and old former athletes. Comparison with still active athletes of the same ages. Circulation 38(6):1104–15
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 16(3):233–271
Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I et al (1986) Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 57(6):450–458
D’Oronzio U, Senn O, Biaggi P, Gruner C, Jenni R, Tanner FC et al (2012) Right heart assessment by echocardiography: gender and body size matters. J Am Soc Echocardiogr 25(12):1251–1258
Quan H, Chen G, Walker RL, Wielgosz A, Dai S, Tu K et al (2013) Incidence, cardiovascular complications and mortality of hypertension by sex and ethnicity. Heart 99(10):715–721
Kronborg CN, Hallas J, Jacobsen IA (2009) Prevalence, awareness, and control of arterial hypertension in Denmark. J Am SocHypertens 3(1):19–24
Maffessanti F, Muraru D, Esposito R, Gripari P, Ermacora D, Santoro C et al (2013) Age-, body size-, and sex-specific reference values for right ventricular volumes and ejection fraction by three-dimensional echocardiography: a multicenter echocardiographic study in 507 healthy volunteers. Circ Cardiovasc Imaging 6(5):700–710. https://doi.org/10.1161/circimaging.113.000706
Papathanasiou G, Zerva E, Zacharis I, Papandreou M, Papageorgiou E, Tzima C et al (2015) Association of high blood pressure with body mass index, smoking and physical activity in healthy young adults. OpenCardiovascMedJ 9:5–17
Saladini F, Benetti E, Fania C, Mos L, Casiglia E, Palatini P (2016) Effects of smoking on central blood pressure and pressure amplification in hypertension of the young. VascMed 21(5):422–428
Moreira HT, Armstrong AC, Nwabuo CC, Vasconcellos HD, Schmidt A, Sharma RK et al (2020) Association of smoking and right ventricular function in middle age: CARDIA study. Open Heart 7(1):e001270. https://doi.org/10.1136/openhrt-2020-001270
Tang KL, Rashid R, Godley J, Ghali WA (2016) Association between subjective social status and cardiovascular disease and cardiovascular risk factors: a systematic review and meta-analysis. BMJ Open 6(3):e010137
Holtermann A, Marott JL, Gyntelberg F, Søgaard K, Mortensen OS, Prescott E et al (2015) Self-reported cardiorespiratory fitness: prediction and classification of risk of cardiovascular disease mortality and longevity—a prospective investigation in the Copenhagen City Heart Study. J Am Heart Assoc 4(1):e001495. https://doi.org/10.1161/jaha.114.001495
Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M et al (2014) 2013 ESH/ESC practice guidelines for the management of arterial hypertension. Blood Press 23(1):3–16
Fitzgerald DJ, O’Callaghan WG, O’Malley K, O’Brien ET (1981) Accuracy of the London School of Hygiene and Remler M2000 sphygmomanometers. Clin Sci (Lond) 61(Suppl 7):399s–401s
Prescott E, Holst C, Grønbæk M, Schnohr P, Jensen G, Barefoot J (2003) Vital exhaustion as a risk factor for ischaemic heart disease and all-cause mortality in a community sample. A prospective study of 4084 men and 5479 women in the Copenhagen City Heart Study. IntJ Epidemiol 32(6):990–7
Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP (1990) Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med 322(22):1561–1566
Haykowsky MJ, Dressendorfer R, Taylor D, Mandic S, Humen D (2002) Resistance training and cardiac hypertrophy. Sports Med 32(13):837–849
Diaz T, Pencina MJ, Benjamin EJ, Aragam J, Fuller DL, Pencina KM et al (2009) Prevalence, clinical correlates, and prognosis of discrete upper septal thickening on echocardiography: the Framingham Heart Study. Echocardiography (Mount Kisco, NY) 26(3):247–253
Grossman W, Jones D, McLaurin L (1975) Wall stress and patterns of hypertrophy in the human left ventricle. J Clin Invest 56(1):56–64
Krause N, Brand RJ, Kaplan GA, Kauhanen J, Malla S, Tuomainen TP et al (2007) Occupational physical activity, energy expenditure and 11-year progression of carotid atherosclerosis. Scand J Work Environ Health 33(6):405–424
Pluim BM, Zwinderman AH, van der Laarse A, van der Wall EE (2000) The athlete’s heart: a meta-analysis of cardiac structure and function. Circulation 101(3):336–344
Arnold N, Deiseroth A, Hahad O, Diestelmeier S, Schulz A, Daubenbüchel A et al (2021) Domains of physical activity in relation to stiffness index in the general population. J Am Heart Assoc 10(16):e020930
Quinn TD, Kline CE, Nagle E, Radonovich LJ, Alansare A, Gibbs BB (2021) Cardiovascular responses to physical activity during work and leisure. Occup Environ Med. https://doi.org/10.1136/oemed-2021-107551
Makai P, IntHout J, Deinum J, Jenniskens K, van der Wilt GJ (2017) A network meta-analysis of clinical management strategies for treatment-resistant hypertension: making optimal use of the evidence. J Gen Intern Med 32(8):921–930
Klabunde R (2011) Cardiovascular physiology concepts. Lippincott Williams & Wilkins, Philadelphia
Li CY, Sung FC (1999) A review of the healthy worker effect in occupational epidemiology. Occup Med (Lond) 49(4):225–229
Robinson BF (1967) Relation of heart rate and systolic blood pressure to the onset of pain in angina pectoris. Circulation 35(6):1073–1083
Cuspidi C, Rescaldani M, Sala C, Negri F, Grassi G, Mancia G (2012) Prevalence of electrocardiographic left ventricular hypertrophy in human hypertension: an updated review. J Hypertens 30(11):2066–2073. https://doi.org/10.1097/HJH.0b013e32835726a3
Sixth European Working Conditiona Survey 2015. https://www.eurofound.europa.eu/surveys/european-working-conditions-surveys/sixth-european-working-conditions-survey-2015 (2015). Accessed 2020.
Arbejde og Helbred. https://at.dk/arbejdsmiljoe-i-tal/analyser-og-publikationer/arbejdsmiljoe-og-helbred-2012-2018/ (2018). Accessed.
Rubak TS, Svendsen SW, Andersen JH, Haahr JPL, Kryger A, Jensen LD et al (2014) An expert-based job exposure matrix for large scale epidemiologic studies of primary hip and knee osteoarthritis: the Lower Body JEM. BMC Musculoskelet Disord 15(1):204
Stock SR, Fernandes R, Delisle A, Vezina N (2005) Reproducibility and validity of workers’ self-reports of physical work demands. Scand J Work Environ Health 31(6):409–437
Acknowlegdements
The authors would like to thank Harald Hannerz and Andreas Holtermann for raising the initial idea of investigating occupational lifting as a risk factor for cardiovascular disease in the Copenhagen City Heart Study, leading to this investigation of cardiac structure and function in relation to heavy occupational lifting. The project is funded by the Danish taxpayers, via the Danish Work Environment Research Foundation, Grant Number 20150067515.
Funding
The project is funded by the Danish taxpayers, via the Danish Work Environment Research Foundation, Grant Number 20150067515.
Author information
Authors and Affiliations
Contributions
MK designed the study, applied for and recieved funding. MK performed the statistical analyses and drafted the manuscript. KGS, MCHL and NDJ performed the data processing from raw material to data for statistical analyses. JLM merged the data and contributed to the statistical analyses. PS commented on the design for the study and the manuscript, as well as lead the initial data collection. TBS contributed to the drafting of the manuscript and supervised the interpretation of the statistical analyses.
Corresponding author
Ethics declarations
Conflict of interest
Nothing to disclose.
Ethical approval
The Danish Data Protection Agency approved the Copenhagen City Heart Study (Approval No.: 2001-54-0280; 2007-58-0015, 2012-58-0004, HEH-2015-045, Isuite 03741), as well as the National Committee on Health Research Ethics approved the data collection (Approval No.: VEK: H-KF 01–144/01 31104).
Consent to participate
All participation was voluntary and conducted in agreement with the Declaration of Helsinki, and written consent from all participants were colledted prior to data collection.
Consent for publication
COI for all authors are attached.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Korshøj, M., Skaarup, K.G., Lassen, M.C.H. et al. Association between exposure to heavy occupational lifting and cardiac structure and function: a cross-sectional analysis from the Copenhagen City Heart Study. Int J Cardiovasc Imaging 38, 521–532 (2022). https://doi.org/10.1007/s10554-021-02420-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-021-02420-y