Abstract
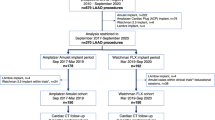
Purpose: To bridge neo-endothelialization (NE) of implanted left atrial appendage closure (LAA/LAAC) devices, dual antiplatelet therapy is prescribed. Cardiac computed tomography angiography (cCTA) has been proposed for the evaluation of interventional LAAC. This prospective longitudinal observational study applied a standardized imaging protocol to detect progression of NE of LAAC devices 6 months after implantation. Methods: Consecutive cCTA datasets of patients six months after LAAC were acquired and the standardized multi-planar reconstruction LAA occluder view for post-implantation evaluation (LOVE) algorithm was used. Residual flow of contrast agent inside the LAA without a peri-device leak (PDL) was defined as incomplete neo-endothelialization. Absence of residual flow was defined as complete neo-endothelialization. Since PDL allows residual flow in the LAA, irrespective of neoendothelialization, PDL were excluded from this study. Diabetes mellitus, liver disease, body-mass-index, age, device sizes and type will be assessed as predictors for incomplete NE. Results: 53 consecutive patients were recruited for cCTA imaging. 36 (68%) showed no PDL and were included in the study (median age 77 years, 19% female). At median follow-up of 6 months (median 180 days, IQR 178–180), 44% of patients showed complete NE compared to 56% with NE still incomplete. Age, BMI, device type and size as well as prevalence of diabetes mellitus and liver disease did not show significant correlation with the completeness of NE. Conclusion: This pilot study showed that neo-endothelialization is still incomplete in a majority of patients at mid-term follow-up of 6 months after successful LAAC therapy. Further investigation on the consequences of incomplete endothelialization is needed to guide antiplatelet therapy schedules.






Similar content being viewed by others
References
Blackshear JL, Odell JA (1996) Appendage obliteration to reduce stroke in cardiac surgical patients with atrial fibrillation. Ann Thorac Surg 61(2):755–759
Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH et al (2012) 2012 focused update of the ESC guidelines for the management of atrial fibrillation: an update of the 2010 ESC guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J 33(21):2719–47
Noseworthy PA, Yao X, Gersh BJ, Hargraves I, Shah ND, Montori VM (2017) Long-term stroke and bleeding risk in patients with atrial fibrillation treated with oral anticoagulants in contemporary practice: providing evidence for shared decision-making. Int J Cardiol 245:174–177
Yu YB, Liu J, Fu GH, Fang RY, Gao F, Chu HM (2018) Comparison of dabigatran and warfarin used in patients with non-valvular atrial fibrillation: Meta-analysis of random control trial. Medicine (Baltimore) 97(46):e12841
Reddy VY, Doshi SK, Sievert H, Buchbinder M, Neuzil P, Huber K et al (2013) Percutaneous left atrial appendage closure for stroke prophylaxis in patients with atrial fibrillation: 2.3-Year Follow-up of the PROTECT AF (Watchman Left Atrial Appendage System for Embolic Protection in Patients with Atrial Fibrillation) Trial. Circulation. 127(6):720–9
Schwartz RS, Holmes DR, Van Tassel RA, Hauser R, Henry TD, Mooney M et al (2010) Left atrial appendage obliteration: mechanisms of healing and intracardiac integration. JACC Cardiovasc Interv 3(8):870–877
Massarenti L, Yilmaz A (2012) Incomplete endothelialization of left atrial appendage occlusion device 10 months after implantation. J Cardiovasc Electrophysiol 23(12):1384–1385
Schiettekatte S, Czapla J, Nijs J, La Meir M (2014) Unmasking a naked left atrial appendage closure device: a case of a silent embolic threat. Heart Rhythm 11(12):2314–2315
Granier M, Laugaudin G, Massin F, Cade S, Winum PF, Freitag C et al (2018) Occurrence of incomplete endothelialization causing residual permeability after left atrial appendage closure. J Invasive Cardiol 30(7):245–250
Behnes M, Akin I, Sartorius B, Fastner C, El-Battrawy I, Borggrefe M et al (2016) –LAA Occluder View for post-implantation Evaluation (LOVE)–standardized imaging proposal evaluating implanted left atrial appendage occlusion devices by cardiac computed tomography. BMC Med Imaging 16:25
Lindner S, Behnes M, Wenke A, Sartorius B, Dieker W, Ansari U, et al. Relation of left atrial appendage closure devices to topographic neighboring structures using standardized imaging by cardiac computed tomography angiography. Clin Cardiol (2018).
Lindner S, Behnes M, Wenke A, Sartorius B, Ansari U, Akin M, et al. Assessment of peri-device leaks after interventional left atrial appendage closure using standardized imaging by cardiac computed tomography angiography. Int J Cardiovasc Imaging (2018).
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B et al (2016) 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J 37(38):2893–2962
Fastner C, Behnes M, Sartorius B, Yildiz M, Mashayekhi K, El-Battrawy I et al (2016) Left atrial appendage morphology, echocardiographic characterization, procedural data and in-hospital outcome of patients receiving left atrial appendage occlusion device implantation: a prospective observational study. BMC Cardiovasc Disord 16:25
KDIGO (2012) Clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int 3(1):1–150
Qamar SR, Jalal S, Nicolaou S, Tsang M, Gilhofer T, Saw J (2019) Comparison of cardiac computed tomography angiography and transoesophageal echocardiography for device surveillance after left atrial appendage closure. EuroIntervention 15(8):663–670
Cochet H, Iriart X, Sridi S, Camaioni C, Corneloup O, Montaudon M et al (2018) Left atrial appendage patency and device-related thrombus after percutaneous left atrial appendage occlusion: a computed tomography study. Eur Heart J Cardiovasc Imaging 19(12):1351–1361
Dieker W, Behnes M, Fastner C, Sartorius B, Wenke A, Sing-Gill I et al (2018) Impact of left atrial appendage morphology on thrombus formation after successful left atrial appendage occlusion: assessment with cardiac-computed-tomography. Sci Rep 8(1):1670
Barth C, Behnes M, Borggrefe M, Akin I (2018) Peri-interventional embolization of left atrial appendage occlusion devices: two manoeuvers of successful retrieval. European Heart Journal – Case Reports 2(1):1–3
Mahesh M, Cody DD (2007) Physics of cardiac imaging with multiple-row detector CT. Radiographics 27(5):1495–1509
Xu L, Zhang Z (2010) Coronary CT angiography with low radiation dose. Int J Cardiovasc Imaging 26(Suppl 1):17–25
Weininger M, Barraza JM, Kemper CA, Kalafut JF, Costello P, Schoepf UJ (2011) Cardiothoracic CT angiography: current contrast medium delivery strategies. AJR Am J Roentgenol 196(3):W260–W272
Funding
This study was not supported by any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study has been approved by the Institutional Review Board (IRB).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Consent for publication
Consent for publication was obtained for every individual person’s data included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lindner, S., Behnes, M., Wenke, A. et al. Incomplete neo-endothelialization of left atrial appendage closure devices is frequent after 6 months: a pilot imaging study. Int J Cardiovasc Imaging 37, 2291–2298 (2021). https://doi.org/10.1007/s10554-021-02192-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-021-02192-5