Abstract
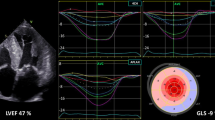
Left atrial (LA) mechanics assessed by two-dimensional speckle tracking echocardiography (2D-STE) have not been extensively studied and clearly characterized in patients with moderate aortic stenosis (AS). Accordingly, we aimed to evaluate the usefulness of LA reservoir strain for risk stratification of asymptomatic patients with moderate AS. This retrospective study included all consecutive asymptomatic patients with moderate AS who underwent transthoracic echocardiography implemented with 2D-STE analysis of LA myocardial strain and strain rate indices at our Institution, between February 2011 and September 2019. During the follow-up period, we evaluated the occurrence of any of the following: (1) CV hospitalization; (2) The recourse to AS surgery; (3) Cardiac death or sudden death. A total of 186 patients (mean age 71.9 ± 12.7 years, 61.8% men) were included in the present study. During a mean follow-up of 2.3 ± 1.9 years, no patients died and 63 adverse CV events were recorded: 48 patients were hospitalized because of heart failure (28 patients), acute coronary syndrome (10 patients), arrhythmias (10 patients) and 15 patients underwent AS surgery. At the multivariate Cox regression analysis, type 2 diabetes mellitus (OR 1.87, 95%CI 1.05–3.34, p = 0.03), NT-proBNP (OR average 1.14, 95%CI 1.02–1.27, p = 0.02), average E/e′ ratio (OR 1.07, 95%CI 1.01–1.15, p = 0.04) and most of all left atrial positive global strain (LA-GSA+) (OR 0.85, 95%CI 0.81–0.90, p < 0.0001) were independently associated with the outcome. LA-GSA+ (optimal cut-off ≤ 19%, AUC = 0.94, 87% sensitivity, 99% specificity, positive predictive value 99%, negative predictive value 88%) showed the highest diagnostic performance. An impaired LA reservoir strain can contribute to identify a subset of asymptomatic patients with moderate AS at higher risk, who may benefit from closer echocardiographic follow-up and/or early surgery.




Similar content being viewed by others
Abbreviations
- 2D:
-
Two-dimensional
- ACS:
-
Acute coronary syndrome
- AF:
-
Atrial fibrillation
- AS:
-
Aortic stenosis
- AUC:
-
Area under the curve
- AVA:
-
Aortic valve area
- BP:
-
Blood pressure
- BSA:
-
Body surface area
- CAD:
-
Coronary artery disease
- CHF:
-
Congestive heart failure
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- CV:
-
Cardiovascular
- EaI:
-
Arterial elastance index
- ECG:
-
Electrocardiogram
- eGFR:
-
Estimated glomerular filtration rate
- ESP:
-
End-systolic pressure
- GSA+:
-
Positive global atrial strain
- GSA−:
-
Negative global atrial strain
- GSR+:
-
Positive global strain rate
- GSRE:
-
Global early-diastolic strain rate
- GSRL:
-
Global late-diastolic strain rate
- HR:
-
Heart rate
- ICC:
-
Intraclass correlation coefficient
- LDL:
-
Low-density lipoprotein
- LA:
-
Left atrial
- LAVi:
-
Left atrial volume index
- LV:
-
Left ventricular
- LVEDVi:
-
Left ventricular end-diastolic volume index
- LVEF:
-
Left ventricular ejection fraction
- LVFP:
-
Left ventricular filling pressure
- LVMi:
-
Left ventricular mass index
- LVOT:
-
Left ventricular outflow tract
- MR:
-
Mitral regurgitation
- MTPG:
-
Mean transaortic pressure gradient
- NT-proBNP:
-
N-terminal pro–B-type natriuretic peptide
- PH:
-
Pulmonary hypertension
- RVIT:
-
Right ventricular inflow tract
- ROC:
-
Receiver operating characteristics
- SPAP:
-
Systolic pulmonary artery pressure
- SR:
-
Strain rate
- STE:
-
Speckle tracking echocardiography
- SVi:
-
Stroke volume index
- TAPSE:
-
Tricuspid annular plane systolic excursion
- TAVR:
-
Transcatheter aortic valve replacement
- TRV:
-
Tricuspid regurgitation velocity
- TTE:
-
Transthoracic echocardiography
References
Turina J, Hess O, Sepulcri F, Krayenbuehl HP (1987) Spontaneous course of aortic valve disease. Eur Heart J 8:471–483
Horstkotte D, Loogen F (1988) The natural history of aortic valve stenosis. Eur Heart J 9:57–64
Delesalle G, Bohbot Y, Rusinaru D, Delpierre Q, Maréchaux S, Tribouilloy C (2019) Characteristics and prognosis of patients with moderate aortic stenosis and preserved left ventricular ejection fraction. J Am Heart Assoc 8:e011036
Rosenhek R, Klaar U, Schemper M et al (2004) (2004) Mild and moderate aortic stenosis: natural history and risk stratification by echocardiography. Eur Heart J 25:199–205
Kennedy KD, Nishimura RA, Holmes DR Jr, Bailey KR (1991) Natural history of moderate aortic stenosis. J Am Coll Cardiol 17:313–319
Otto CM, Burwash IG, Legget ME et al (1997) Prospective study of asymptomatic valvular aortic stenosis. Clinical, echocardiographic, and exercise predictors of outcome. Circulation 95:2262–2270
Yechoor P, Blaustein AS, Bakaeen FG et al (2013) The natural history of moderate aortic stenosis in a veteran population. J Thorac Cardiovasc Surg 145:1550–1553
Cioffi G, Faggiano P, Vizzardi E et al (2011) Prognostic effect of inappropriately high left ventricular mass in asymptomatic severe aortic stenosis. Heart 97:301–307
Messika-Zeitoun D, Bielak LF, Peyser PA et al (2007) Aortic valve calcification: determinants and progression in the population. Arterioscler Thromb Vasc Biol 27:642–648
Rosenhek R, Binder T, Porenta G et al (2000) Predictors of outcome in severe, asymptomatic aortic stenosis. N Engl J Med 343:611–617
Lancellotti P, Lebois F, Simon M, Tombeux C, Chauvel C, Pierard LA (2005) Prognostic importance of quantitative exercise Doppler echocardiography in asymptomatic valvular aortic stenosis. Circulation 112:I377–I382
Zlotnick DM, Ouellette ML, Malenka DJ et al (2013) Effect of preoperative pulmonary hypertension on outcomes in patients with severe aortic stenosis following surgical aortic valve replacement. Am J Cardiol 112:1635–1640
Lancellotti P, Magne J, Donal E et al (2012) Determinants and prognostic significance of exercise pulmonary hypertension in asymptomatic severe aortic stenosis. Circulation 126:851–859
Bergler-Klein J, Klaar U, Heger M et al (2004) Natriuretic peptides predict symptom-free survival and postoperative outcome in severe aortic stenosis. Circulation 109:2302–2308
Galli E, Fournet M, Chabanne C et al (2015) Prognostic value of left atrial reservoir function in patients with severe aortic stenosis: a 2D speckle-tracking echocardiographic study. Eur Heart J Cardiovasc Imaging 17:533–41
Todaro MC, Carerj S, Khandheria B et al (2016) Usefulness of atrial function for risk stratification in asymptomatic severe aortic stenosis. J Cardiol 67:71–79
Marques-Alves P, Marinho AV, Teixeira R et al (2019) Going beyond classic echo in aortic stenosis: left atrial mechanics, a new marker of severity. BMC Cardiovasc Disord 19:215
Antonini-Canterin F, Di Nora C, Cervesato E et al (2018) Value of ejection fraction/velocity ratio in the prognostic stratification of patients with asymptomatic aortic valve stenosis. Echocardiography 35:1909–1914
Ito S, Miranda WR, Nkomo VT et al (2020) Prognostic risk stratification of patients with moderate aortic stenosis. J Am Soc Echocardiogr. https://doi.org/10.1016/j.echo.2020.10.012
Baumgartner H, Hung J, Bermejo J et al (2017) Recommendations on the echocardiographic assessment of aortic valve stenosis: a focused update from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. J Am Soc Echocardiogr 30:372–392
Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D (1999) A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of diet in renal disease study group. Ann Intern Med 130:461–470
Lang RM, Badano LP, Mor-Avi V et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28:1-39.e14
Nagueh SF, Smiseth OA, Appleton CP et al (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 29:277–314
Devereux RB, Alonso DR, Lutas EM et al (1986) Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 57:450–458
Rudski LG, Lai WW, Afilalo J et al (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23:685–713
Redfield MM, Jacobsen SJ, Borlaug BA et al (2005) Age- and gender-related ventricular-vascular stiffening: a community-based study. Circulation 112:2254–2262
Chen CH, Fetics B, Nevo E et al (2001) Noninvasive single-beat determination of left ventricular end-systolic elastance in humans. J Am Coll Cardiol 38:2028–2034
Kusunose K, Yamada H, Nishio S et al (2012) Index-beat assessment of left ventricular systolic and diastolic function during atrial fibrillation using myocardial strain and strain rate. J Am Soc Echocardiogr 25:953–959
Thomas L, McKay T, Byth K, Marwick TH (2007) Abnormalities of left atrial function after cardioversion: an atrial strain rate study. Heart 93:89–95
Lin JD, Chen YL, Wu CZ et al (2016) Identification of normal blood pressure in different age group. Medicine (Baltimore) 95:e3188
Wetzels JF, Kiemeney LA, Swinkels DW, Willems HL, den Heijer M (2007) Age- and gender-specific reference values of estimated GFR in Caucasians: the Nijmegen Biomedical Study. Kidney Int 72:632–637
Catapano AL, Graham I, De Backer G et al (2016) 2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur Heart J 37:2999–3058
Hughes D, Talwar S, Squire IB, Davies JE, Ng LL (1999) An immunoluminometric assay for N-terminal pro-brain natriuretic peptide: development of a test for left ventricular dysfunction. Clin Sci (Lond) 96:373–380
Antonini-Canterin F, Poli S, Vriz O, Pavan D, Bello VD, Nicolosi GL (2013) The ventricular-arterial coupling: from basic pathophysiology to clinical application in the echocardiography laboratory. J Cardiovasc Echogr 23:91–95
Sugimoto T, Robinet S, Dulgheru R et al (2018) Echocardiographic reference ranges for normal left atrial function parameters: results from the EACVI NORRE study. Eur Heart J Cardiovasc Imaging 19:630–638
Baumgartner H, Falk V, Bax JJ et al (2017) 2017 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J 38:2739–2791
Nishimura RA, Otto CM, Bonow RO et al (2014) 2014 AHA/ACC guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 129:2440–2492
Faggiano P, Antonini-Canterin F, Erlicher A et al (2003) Progression of aortic valve sclerosis to aortic stenosis. Am J Cardiol 91:99–101
van Gils L, Clavel MA, Vollema EM et al (2017) Prognostic implications of moderate aortic stenosis in patients with left ventricular systolic dysfunction. J Am Coll Cardiol 69:2383–2392
Cameli M, Mandoli GE, Loiacono F et al (2016) Left atrial strain: a new parameter for assessment of left ventricular filling pressure. Heart Fail Rev 21:65–76
Lin J, Ma H, Gao L et al (2020) Left atrial reservoir strain combined with E/E′ as a better single measure to predict elevated LV filling pressures in patients with coronary artery disease. Cardiovasc Ultrasound 25(18):11
Fan JL, Su B, Zhao X et al (2020) Correlation of left atrial strain with left ventricular end-diastolic pressure in patients with normal left ventricular ejection fraction. Int J Cardiovasc Imaging 36:1659–1666
Longobardo L, Todaro MC, Zito C et al (2014) Role of imaging in assessment of atrial fibrosis in patients with atrial fibrillation: state-of-the-art review. Eur Heart J Cardiovasc Imaging 15:1–5
Zaid RR, Barker CM, Little SH, Nagueh SF (2013) Pre- and post-operative diastolic dysfunction in patients with valvular heart disease: diagnosis and therapeutic implications. J Am Coll Cardiol 62:1922–1930
Chin CWL, Everett RJ, Kwiecinski J et al (2017) Myocardial fibrosis and cardiac decompensation in aortic stenosis. JACC Cardiovasc Imaging 10:1320–1333
Aalaei-Andabili SH, Bavry AA (2019) Left ventricular diastolic dysfunction and transcatheter aortic valve replacement outcomes: a review. Cardiol Ther 8:21–28
Salas-Pacheco JL, Ávila-Vanzzini N, Eugenia REM, Arias-Godínez JA (2016) Left atrium function by 2D speckle tracking in aortic valve disease. Echocardiography 33:1828–1834
Calin A, Mateescu AD, Rosca M et al (2017) Left atrial dysfunction as a determinant of pulmonary hypertension in patients with severe aortic stenosis and preserved left ventricular ejection fraction. Int J Cardiovasc Imaging 33:1939–1947
Kamalesh M, Ng C, El Masry H et al (2009) Does diabetes accelerate progression of calcific aortic stenosis? Eur J Echocardiogr 10:723–725
Natorska J, Wypasek E, Grudzien G et al (2012) Does diabetes accelerate the progression of aortic stenosis through enhanced inflammatory response within aortic valves? Inflammation 3:834–840
Larsson S, Wallin A, Hakansson N et al (2018) Type 1 and type 2 diabetes and incidence of seven cardiovascular diseases. Int J Cardiol 262:66–70
Messika-Zeitoun D, Aubry MC, Detaint D et al (2004) Evaluation and clinical implications of aortic valve calcification measured by electron-beam computed tomography. Circulation 110:356–362
D’Ascenzi F, Cameli M, Henein M et al (2013) Left atrial remodelling in patients undergoing transcatheter aortic valve implantation: a speckle-tracking prospective, longitudinal study. Int J Cardiovasc Imaging 29:1717–1724
Sonaglioni A, Vincenti A, Baravelli M et al (2019) Prognostic value of global left atrial peak strain in patients with acute ischemic stroke and no evidence of atrial fibrillation. Int J Cardiovasc Imaging 35:603–613
Voigt JU, Pedrizzetti G, Lysyansky P et al (2015) Definitions for a common standard for 2D speckle tracking echocardiography: consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging 16:1–11
Acknowledgements
This work has been supported by Italian Ministry of Health Ricerca Corrente—IRCCS MultiMedica.
Author information
Authors and Affiliations
Contributions
AS: Conceptualization; Data curation; Investigation; Methodology; Software; Visualization; Writing—original draft. GLN: Conceptualization; Data curation; Methodology; Writing—review & editing. ER: Conceptualization; Data curation; Methodology; Writing—review & editing. ML: Conceptualization; Supervision; Validation; Writing—review & editing.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflicts of interest associated with this publication.
Ethical approval
All procedures performed in the present study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sonaglioni, A., Nicolosi, G.L., Rigamonti, E. et al. Incremental prognostic role of left atrial reservoir strain in asymptomatic patients with moderate aortic stenosis. Int J Cardiovasc Imaging 37, 1913–1925 (2021). https://doi.org/10.1007/s10554-021-02175-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-021-02175-6