Abstract
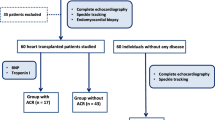
Cardiac allograft vasculopathy (CAV) is an obliterative and diffuse type of coronaropathy that develops in the transplanted human heart, representing a major cause of graft failure and mortality. Nowadays the gold standard for the diagnosis of CAV is coronary angiography (CA). Non-invasive CAV detection, especially in the early stages of the disease, is still challenging. Our study aimed to investigate the role of speckle tracking echocardiography (STE), in particular three-layer STE, in predicting CAV at early stages, and if other traditional echocardiographic, clinical or biochemical parameters could relate to CAV. The study population was composed of a total of 33 heart transplanted patients, divided accordingly to the presence or absence of CAV (12 CAV+ , 22 CAV−). All subjects underwent a complete transthoracic echocardiographic examination on the same day of the CA, and all conventional parameters of myocardial function were obtained, including strain values assessed by STE. Strain values were significantly reduced in presence of CAV, at each myocardial layer but in particular the endocardial-epicardial gradient (− 4.15 ± 1.6 vs − 1.7 ± 0.4% < .0001) that was also highly predictive of CAV (AUC at ROC curve 0.97). Among diastolic parameters, the E wave deceleration time (DT) and the mean E/e′ ratio were strongly positively associated with CAV. In our population, left ventricular global longitudinal strain (GLS), layer-specific GLS and the endocardial-epicardial LS gradient, E wave DT and E/e′ ratio were the best independent non-invasive predictors of CAV.


Similar content being viewed by others
References
Chang DH, Kobashigawa JA (2015) Current diagnostic and treatment strategies for cardiac allograft vasculopathy. Expert Rev Cardiovasc Ther 13:1147–1154
Sipahi I, Starling RC (2007) Cardiac allograft vasculopathy: an update. Heart Fail Clin 3:87–95
Morisco C, Barbato E (2019) From microvascular impairment to cardiac allograft vasculopathy: a disease continuum. Int J Cardiol 290:33
Mehra MR, Crespo-Leiro MG, Dipchand A et al (2010) International Society for Heart and Lung Transplantation working formulation of a standardized nomenclature for cardiac allograft vasculopathy–2010. J Heart Lung Transplant 29:717–727
Costanzo MR, Dipchand A, Starling R et al (2010) The International Society of Heart and Lung Transplantation Guidelines for the care of heart transplant recipients. J Heart Lung Transplant 29:914–956
Dedieu N, Silva Vieira M, Fenton M, Wong J, Botnar R, Burch M, Greil G, Hussain T (2018) The importance of qualitative and quantitative regional wall motion abnormality assessment at rest in pediatric coronary allograft vasculopathy. Pediatr Transplant Pediatr Transplant 22:e13208
Erbel C, Mukhammadaminova N, Gleissner CA, Osman NF, Hofmann NP, Steuer C, Akhavanpoor M, Wangler S, Celik S, Doesch AO, Voss A, Buss SJ, Schnabel PA, Katus HA, Korosoglou G (2016) Myocardial perfusion reserve and strain-encoded CMR for evaluation of cardiac allograft microvasculopathy. JACC Cardiovasc Imaging 9:255–266
Shenoy C, Romano S, Hughes A, Okasha O, Nijjar PS, Velangi P, Martin CM, Akçakaya M, Farzaneh-Far A (2020) Cardiac magnetic resonance feature tracking global longitudinal strain and prognosis after heart transplantation. JACC Cardiovasc Imaging 13:1934–1942
Eleid MF, Caracciolo G, Cho EJ et al (2010) Natural history of left ventricular mechanics in transplanted hearts: relationships with clinical variables and genetic expression profiles of allograft rejection. J Am Coll Cardiol Img 3:989–1000
Sato T, Kato TS, Kamamura K et al (2011) Utility of left ventricular systolic torsion derived from 2-dimensional speckle-tracking echocardiography in monitoring acute cellular rejection in heart transplant recipients. J Heart Lung Transplant 30:536–543
Mingo-Santos S, Moñivas-Palomero V, Garcia-Lunar I et al (2015) Usefulness of two-dimensional strain parameters to diagnose acute rejection after heart transplantation. J Am Soc Echocardiogr 28:1149–1156
Clemmensen TS, Løgstrup BB, Eiskjær H, Poulsen SH (2015) Evaluation of longitudinal myocardial deformation by 2-dimensional speckle-tracking echocardiography in heart transplant recipients: relation to coronary allograft vasculopathy. J Heart Lung Transplant 34(2):195–203
Clemmensen TS, Eiskjær H, Løgstrup BB, Tolbod LP, Harms HJ, Bouchelouche K, Hoff C, Frøkiær J, Poulsen SH (2016) Noninvasive detection of cardiac allograft vasculopathy by stress exercise echocardiographic assessment of myocardial deformation. J Am Soc Echocardiogr 29:480–490
Ghali MCZ, Stewart R, Ghali GZ, Blitzer W (2020) Two dimensional speckle tracking echocardiography detects cardiac allograft stage III vasculopathy in recipients of heart transplants with preserved systolic function. Acta Cardiol 31:1–11
Dandel M, Lehmkuhl H, Knosalla C, Grauhan O, Weng Y, Pasic M, Hetzer R (2008) Echocardiographic 2D-strain imaging for early detection of patients with focal coronary stenoses after heart transplantation. J Heart Lung Transplant 27(2 Suppl 1):S95-96
Logstrup BB, Hofsten DE, Christophersen TB et al (2012) Correlation between left ventricular global and regional longitudinal systolic strain and impaired microcirculation in patients with acute myocardial infarction. Echocardiography 10:1181–1190
Mizuguchi Y, Oishi Y, Miyoshi H, Iuchi A, Nagase N, Oki T (2008) The functional role of longitudinal, circumferential, and radial myocardial deformation for regulating the early impairment of left ventricular contraction and relaxation in patients with cardiovascular risk factors: a study with two-dimensional strain imaging. J Am Soc Echocardiogr 21:1138–1144
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T, Lancellotti P, Muraru D, Picard MH, Rietzschel ER, Rudski L, Spencer KT, Tsang W, Voigt JU (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28(1):1-39.e14
Olymbios M, Kwiecinski J, Berman DS, Kobashigawa JA (2018) Imaging in heart transplant patients. JACC Cardiovasc Imaging 11(10):1514–1530
Cohn JM, Wilensky RL, O’Donnell JA, Bourdillon PDV, Dillon JC, Feigenbaum H (1996) Exercise echocardiography, angiography, and intracoronary ultrasound after cardiac transplantation. Am J Cardiol 77:1216–1219
Akosah KO, Mohanty PK, Funai JT et al (1994) Noninvasive detection of transplant coronary artery disease by dobutamine stress echocardiography. J Heart Lung Transplant 13:1024–1038
Derumeaux G, Redonnet M, Soyer R, Cribier A, Letac B (1998) Assessment of the progression of cardiac allograft vasculopathy by dobutamine stress echocardiography. J Heart Lung Transplant 17:259–267
Chirakarnjanakorn S, Starling RC, Popovic ZB, Griffin BP, Desai MY (2015) Dobutamine stress echocardiography during follow-up surveillance in heart transplant patients: diagnostic accuracy and predictors of outcomes. J Heart Lung Transplant 34:710–717
Clerkin KJ, Farr MA, Restaino SW, Ali ZA, Mancini DM (2016) Dobutamine stress echocardiography is inadequate to detect early cardiac allograft vasculopathy. J Heart Lung Transplant 35:1040–1041
Dandel M, Hetzer R (2017) Post-transplant surveillance for acute rejection and allograft vasculopathy by echocardiography: usefulness of myocardial velocity and deformation imaging. J Heart Lung Transplant 36:117–131
Cameli M, Mandoli GE, Sciaccaluga C, Mondillo S (2019) More than 10 years of speckle tracking echocardiography: still a novel technique or a definite tool for clinical practice? Echocardiography 36(5):958–970
Choi JO, Cho SW, Song YB, Cho SJ, Song BG, Lee SC, Park SW (2009) Longitudinal 2D strain at rest predicts the presence of left main and three vessel coronary artery disease in patients without regional wall motion abnormality. Eur J Echocardiogr 10(5):695–701
Biering-Sorensen T, Hoffmann S, Mogelvang R, Zeeberg Iversen A, Galatius S, Fritz-Hansen T, Bech J, Jensen JS (2014) Myocardial strain analysis by 2-dimensional speckle tracking echocardiography improves diagnostics of coronary artery stenosis in stable angina pectoris. Circ Cardiovasc Imaging 7(1):58–65
Shimoni S, Gendelman G, Ayzenberg O, Smirin N, Lysyansky P, Edri O, Deutsch L, Caspi A, Friedman Z (2011) Differential effects of coronary artery stenosis on myocardial function: the value of myocardial strain analysis for the detection of coronary artery disease. J Am Soc Echocardiogr 24(7):748–757
Nucifora G, Schuijf JD, Delgado V, Bertini M, Scholte AJ, Ng AC, van Werkhoven JM, Jukema JW, Holman ER, van der Wall EE, Bax JJ (2010) Incremental value of subclinical left ventricular systolic dysfunction for the identification of patients with obstructive coronary artery disease. Am Heart J 159(1):148–157
Myers JH, Stirling MC, Choy M, Buda AJ, Gallagher KP (1986) Direct measurement of inner and outer wall thickening dynamics with epicardial echocardiography. Circulation 74(1):164–172
Sabbah HN, Marzilli M, Stein PD (1981) The relative role of subendocardium and subepicardium in left ventricular mechanics. Am J Physiol 240(6):H920–H926
Kim SA, Park SM, Kim MN, Shim WJ (2016) Assessment of left ventricular function by layer-specific strain and its relationship to structural remodelling in patients with hypertension. Can J Cardiol 32(2):211–216
Sarvari SI, Haugaa KH, Zahid W, Bendz B, Aakhus S, Aaberge L, Edvardsen T (2013) Layer-specific quantification of myocardial deformation by strain echocardiography may reveal significant CAD in patients with non-ST-segment elevation acute coronary syndrome. JACC Cardiovasc Imaging 6(5):535–544
Zhang L, Wu WC, Ma H, Wang H (2016) Usefulness of layer-specific strain for identifying complex CAD and predicting the severity of coronary lesions in patients with non-ST-segment elevation acute coronary syndrome: compared with Syntax score. Int J Cardiol 223:1045–1052
Leitman M, Lysiansky M, Lysyansky P, Friedman Z, Tyomkin V, Fuchs T, Adam D, Krakover R, Vered Z (2010) Circumferential and longitudinal strain in 3 myocardial layers in normal subjects and in patients with regional left ventricular dysfunction. J Am Soc Echocardiogr 23(1):64–70
Chih S, Chong AY, Mielniczuk LM, Bhatt DL, Beanlands RS (2016) Allograft vasculopathy: the Achilles’ heel of heart transplantation. J Am Coll Cardiol 68(1):80–91
Weber BN, Kobashigawa JA, Givertz MM (2017) Evolving areas in heart transplantation. JACC Heart Fail 5(12):869–878
Cameli M, Sciaccaluga C, Loiacono F, Simova I, Miglioranza MH, Nistor D, Bandera F, Emdin M, Giannoni A, Ciccone MM, Devito F, Guaricci AI, Favale S, Lisi M, Mandoli GE, Henein M, Mondillo S (2019) The analysis of left atrial function predicts the severity of functional impairment in chronic heart failure: The FLASH multicenter study. Int J Cardiol 286:87–91
Cameli M, Sciaccaluga C, Mandoli GE, D’Ascenzi F, Tsioulpas C, Mondillo S (2019) The role of the left atrial function in the surgical management of aortic and mitral valve disease. Echocardiography 36(8):1559–1565
Sciaccaluga C, D’Ascenzi F, Mandoli GE, Rizzo L, Sisti N, Carrucola C, Cameli P, Bigio E, Mondillo S, Cameli M (2020) Traditional and Novel Imaging of Right Ventricular Function in Patients with Heart Failure and Reduced Ejection Fraction. Curr Heart Fail Rep 17(2):28–33
Badano LP, Miglioranza MH, Edvardsen T et al (2015) European Association of Cardiovascular Imaging/Cardiovascular Imaging Department of the Brazilian Society of Cardiology recommendations for the use of cardiac imaging to assess and follow patients after heart transplantation. Eur Heart J Cardiovasc Imaging 16:919–948
Lopez B, Sanchez V, Delgado JF et al (2012) Accuracy of noninvasive estimation of pulmonary wedge pressure by echocardiographic indices in heart transplant recipients. Transplant Proc 44:2639–2641
Author information
Authors and Affiliations
Contributions
CS, GEM, NS, MBN, AI, DM, SV, SM, MC, MF: takes responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation. AD’, GD: takes responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation. GB: takes responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation. SB, MM: This author takes responsibility for all aspects of the reliability and freedom from bias of the data presented and their discussed interpretation.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest and that they have not received any funding grants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sciaccaluga, C., Mandoli, G.E., Sisti, N. et al. Detection of cardiac allograft vasculopathy by multi-layer left ventricular longitudinal strain in heart transplant recipients. Int J Cardiovasc Imaging 37, 1621–1628 (2021). https://doi.org/10.1007/s10554-020-02147-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-020-02147-2