Abstract
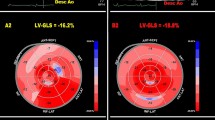
Chest shape might affect myocardial strain parameters. However, the relationship between myocardial strain parameters and chest conformation has not been previously investigated in subjects with mitral valve prolapse (MVP). Between April 2019 and May 2020, 60 healthy subjects (50.1 ± 8.6 year/old, 46.6% females) with MVP and mild-to-moderate mitral regurgitation, and 60 controls matched by age, sex, and cardiovascular risk factors were consecutively studied. Participants underwent modified Haller index (MHI) assessment (ratio of chest transverse diameter over the distance between sternum and spine), and transthoracic echocardiography implemented with 2D-speckle tracking analysis. MHI was significantly greater in MVP group than controls (2.6 ± 0.35 vs 2.1 ± 0.23, p < 0.0001). Left ventricular (LV) ejection fraction was similar in MVP and controls (63.5 ± 3.7% vs 64.3 ± 3.9%, p = 0.25). LV regional and global longitudinal (GLS), circumferential (GCS) and radial strain (GRS) parameters and LV peak twist were all significantly lower in MVP compared to controls (all p < 0.0001). MVP subjects with a tight chest (MHI > 2.5, n = 30), and those with MHI ≤ 2.5 (n = 30) were then separately analyzed. A significant impairment in myocardial strain parameters and LV peak twist was documented in MVP subjects with MHI > 2.5, but not in those with MHI ≤ 2.5. MHI showed a strong inverse correlation with LV-GLS (r = − 0.85), GCS (r = − 0.84), GRS (r = − 0.84) and LV peak twist (r = − 0.94). In MVP subjects, impairment of myocardial strain parameters is not due to intrinsic reduction of cardiac contractility function, but it appears to be related to the degree of chest deformity.




Similar content being viewed by others
Abbreviations
- 2D:
-
Two-dimensional
- AFI:
-
Automated function imaging
- A-P:
-
Antero-posterior
- AVC:
-
Aortic valve closure
- BP:
-
Blood pressure
- BSA:
-
Body surface area
- CI:
-
Confidence interval
- CMR:
-
Cardiovascular magnetic resonance
- DBP:
-
Diastolic blood pressure
- ECG:
-
Electrocardiogram
- GCS:
-
Global circumferential strain
- GLS:
-
Global longitudinal strain
- GRS:
-
Global radial strain
- HR:
-
Heart rate
- ICC:
-
Intraclass correlation coefficient
- LAVi:
-
Left atrial volume index
- LBBB:
-
Left bundle branch block
- L-L:
-
Latero-lateral
- LV:
-
Left ventricular
- LVEF:
-
Left ventricular ejection fraction
- LVFP:
-
Left ventricular filling pressures
- LVMi:
-
Left ventricular mass index
- MHI:
-
Modified Haller index
- MVP:
-
Mitral valve prolapse
- MR:
-
Mitral regurgitation
- NS-STT:
-
Nonspecific ST-segment and T-wave abnormalities
- PE:
-
Pectus excavatum
- RBBB:
-
Right bundle branch block
- ROI:
-
Region of interest
- RV:
-
Right ventricular
- RVEDD:
-
Right ventricular end-diastolic diameter
- RWT:
-
Relative wall thickness
- SBP:
-
Systolic blood pressure
- SPAP:
-
Systolic pulmonary artery pressure
- SR:
-
Strain rate
- STE:
-
Speckle-tracking echocardiography
- TAPSE:
-
Tricuspid annular plane systolic excursion
- TTE:
-
Transthoracic echocardiography
- VPB:
-
Ventricular premature beats
References
Freed LA, Levy D, Levine RA et al (1999) Prevalence and clinical outcome of mitral-valve prolapse. N Engl J Med 341:1–7
Freed LA, Benjamin EJ, Levy D et al (2002) Mitral valve prolapse in the general population: the benign nature of echocardiographic features in the Framingham Heart Study. J Am Coll Cardiol 40:1298–1304
Delling FN, Vasan RS (2014) Epidemiology and pathophysiology of mitral valve prolapse: new insights into disease progression, genetics, and molecular basis. Circulation 129:2158–2170
Devereux RB, Kramer-Fox R, Shear MK, Kligfield P, Pini R, Savage DD (1987) Diagnosis and classification of severity of mitral valve prolapse: methodologic, biologic, and prognostic considerations. Am Heart J 113:1265–1280
Zuppiroli A, Rinaldi M, Kramer-Fox R, Favilli S, Roman MJ, Devereux RB (1995) Natural history of mitral valve prolapse. Am J Cardiol 75:1028–1032
Hayek E, Gring CN, Griffin BP (2005) Mitral valve prolapse. Lancet 365:507–518
Lang RM, Bierig M, Devereux RB et al (2005) Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18:1440–1463
Dandel M, Hetzer R (2009) Echocardiographic strain and strain rate imaging—clinical applications. Int J Cardiol 132:11–24
Carerj S, La Carrubba S, Antonini-Canterin F et al (2010) The incremental prognostic value of echocardiography in asymptomatic stage a heart failure. J Am Soc Echocardiogr 23:1025–1034
Carluccio E, Biagioli P, Alunni G et al (2011) Advantages of deformation indices over systolic velocities in assessment of longitudinal systolic function in patients with heart failure and normal ejection fraction. Eur J Heart Fail 13:292–302
Fukuda S, Song JK, Mahara K et al (2016) Basal left ventricular dilatation and reduced contraction in patients with mitral valve prolapse can be secondary to annular dilatation: preoperative and postoperative speckle-tracking echocardiographic study on left ventricle and mitral valve annulus interaction. Circ Cardiovasc Imaging 9:e005113
Malev E, Zemtsovsky E, Pshepiy A, Timofeev E, Reeva S, Prokudina M (2012) Evaluation of left ventricular systolic function in young adults with mitral valve prolapse. Exp Clin Cardiol 17:165–168
Sonaglioni A, Nicolosi GL, Granato A, Lombardo M, Anzà C, Ambrosio G (2020) Reduced myocardial strain parameters in subjects with pectus excavatum: impaired myocardial function or methodological limitations due to chest deformity? Semin Thorac Cardiovasc Surg S1043–0679(20):30127–30131
Sonaglioni A, Baravelli M, Vincenti A et al (2018) A New modified anthropometric haller index obtained without radiological exposure. Int J Cardiovasc Imaging 34:1505–1509
Piepoli MF, Hoes AW, Agewall S et al (2016) 2016 European guidelines on cardiovascular disease prevention in clinical practice: the sixth joint task force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J 37:2315–2381
Lang RM, Badano LP, Mor-Avi V et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28:1–39
Nagueh SF, Smiseth OA, Appleton CP et al (2016) Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 29:277–314
Parwani P, Avierinos JF, Levine RA, Delling FN (2017) Mitral valve prolapse: multimodality imaging and genetic insights. Prog Cardiovasc Dis 60:361–369
Nishimura RA, Otto CM, Bonow RO et al (2017) 2017 AHA/ACC focused update of the 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation 135:e1159–e1195
Sengupta PP, Tajik AJ, Chandrasekaran K, Khandheria BK (2008) Twist mechanics of the left ventricle: principles and application. JACC Cardiovasc Imaging 1:366–376
Sidden CR, Katz ME, Swoveland BC, Nuss D (2001) Radiologic considerations in patients undergoing the Nuss procedure for correction of pectus excavatum. Pediatr Radiol 31:429–434
Archer JE, Gardner A, Berryman F, Pynsent P (2016) The measurement of the normal thorax using the Haller index methodology at multiple vertebral levels. J Anat 229:577–581
Levy PT, Holland MR, Sekarski TJ, Hamvas A, Singh GK (2013) Feasibility and reproducibility of systolic right ventricular strain measurement by speckle-tracking echocardiography in premature infants. J Am Soc Echocardiogr 26:1201–1213
Nasu Y, Oyama K, Nakano S et al (2015) Longitudinal systolic strain of the bilayered ventricular septum during the first 72 hours of life in preterm infants. J Echocardiogr 13:90–99
Sugimoto T, Dulgheru R, Bernard A et al (2017) Echocardiographic reference ranges for normal left ventricular 2D strain: results from the EACVI NORRE study. Eur Heart J Cardiovasc Imaging 18:833–840
Scampardonis G, Yang SS, Maranhão V, Goldberg H, Gooch AS (1973) Left ventricular abnormalities in prolapsed mitral leaflet syndrome. Review of eighty-seven cases. Circulation 48:287–297
Delhomme C, Casset-Senon D, Babuty D et al (1996) Etude par tomographie cavitaire isotopique de 36 cas de prolapsus valvulaire mitral [a study of 36 cases of mitral valve prolapse by isotopic ventricular tomography]. Arch Mal Coeur Vaiss 89:1127–1135
Lumia FJ, LaManna MM, Atfeh M, Maranhao V (1989) Exercise first-pass radionuclide assessment of left and right ventricular function and valvular regurgitation in symptomatic mitral valve prolapse. Angiology 40:443–449
Casset-Senon D, Babuty D, Philippe L et al (2000) Fourier phase analysis of SPECT equilibrium radionuclide angiography in symptomatic patients with mitral valve prolapse without significant mitral regurgitation: assessment of biventricular functional abnormalities suggesting a cardiomyopathy. J Nucl Cardiol 7:471–477
Bulkley BH, Roberts WC (1975) Dilatation of the mitral anulus. A rare cause of mitral regurgitation. Am J Med 59:457–463
Chandra S, Salgo IS, Sugeng L et al (2011) Characterization of degenerative mitral valve disease using morphologic analysis of real-time three-dimensional echocardiographic images: objective insight into complexity and planning of mitral valve repair. Circ Cardiovasc Imaging 4:24–32
Han Y, Peters DC, Salton CJ et al (2008) Cardiovascular magnetic resonance characterization of mitral valve prolapse. JACC Cardiovasc Imaging 1:294–303
Basso C, Perazzolo Marra M, Rizzo S et al (2015) Arrhythmic mitral valve prolapse and sudden cardiac death. Circulation 132:556–566
Perazzolo Marra M, Basso C, De Lazzari M et al (2016) Morphofunctional abnormalities of mitral annulus and arrhythmic mitral valve prolapse. Circ Cardiovasc Imaging 9:e005030
Bui AH, Roujol S, Foppa M et al (2017) Diffuse myocardial fibrosis in patients with mitral valve prolapse and ventricular arrhythmia. Heart 103:204–209
Salomon J, Shah PM, Heinle RA (1975) Thoracic skeletal abnormalities in idiopathic mitral valve prolapse. Am J Cardiol 36:32–36
Kelly RE, Goretsky MJ, Obermeyer R et al (2010) Twenty-one years of experience with minimally invasive repair of pectus excavatum by the Nuss procedure in 1215 patients. Ann Surg 252:1072–1081
Wright CD (2017) Straight back syndrome. Thorac Surg Clin 27:133–137
Nomura K, Ajiro Y, Nakano S et al (2019) Characteristics of mitral valve leaflet length in patients with pectus excavatum: a single center cross-sectional study. PLoS ONE 14:e0212165
Dahl JS, Videbæk L, Poulsen MK et al (2012) Global strain in severe aortic valve stenosis: relation to clinical outcome after aortic valve replacement. Circ Cardiovasc Imaging 5:613–620
Mignot A, Donal E, Zaroui A et al (2010) Global longitudinal strain as a major predictor of cardiac events in patients with depressed left ventricular function: a multicenter study. J Am Soc Echocardiogr 23:1019–1024
Bertini M, Ng ACT, Antoni ML et al (2012) Global longitudinal strain predicts long-term survival in patients with chronic ischemic cardiomyopathy. Circ Cardiovasc Imaging 5:383–391
Chao CJ, Jaroszewski D, Gotway M et al (2018) Effects of pectus excavatum repair on right and left ventricular strain. Ann Thorac Surg 105:294–301
Truong VT, Li CY, Brown RL et al (2017) Occult RV systolic dysfunction detected by CMR derived RV circumferential strain in patients with pectus excavatum. PLoS ONE 12:e0189128
Lollert A, Emrich T, Eichstädt J et al (2018) Differences in myocardial strain between pectus excavatum patients and healthy subjects assessed by cardiac MRI: a pilot study. Eur Radiol 28:1276–1284
Voigt JU, Pedrizzetti G, Lysyansky P et al (2015) Definitions for a common standard for 2D speckle tracking echocardiography: consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging 16:1–11
Acknowledgement
This work has been supported by Italian Ministry of Health Ricerca Corrente—IRCCS MultiMedica.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the present study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sonaglioni, A., Nicolosi, G.L., Lombardo, M. et al. Influence of chest conformation on myocardial strain parameters in healthy subjects with mitral valve prolapse. Int J Cardiovasc Imaging 37, 1009–1022 (2021). https://doi.org/10.1007/s10554-020-02085-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-020-02085-z