Abstract
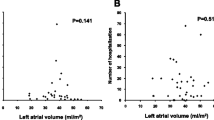
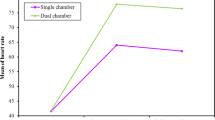
Atrial size and function are closely correlated with atrial contributions to cardiovascular performance. Therefore, in this study, we aimed to assess atrial size and function in pediatric heart transplantation (HTx) patients using three-dimensional echocardiography (3DE). We enrolled 33 clinically well pediatric HTx patients and 33 healthy controls with a similar distribution of sex and age to the HTx patients. All patients underwent two-dimensional echocardiography (2DE) and 3DE. 2DE- and 3DE-derived biatrial maximal volume (Vmax), minimal volume (Vmin), ejection volume (EV), ejection fraction (EF), volume before atrial contraciton (VpreA), passive EV, passive EF, active EV and active EF were obtained in all patients. The 3D left atrail (LA) Vmax, Vmin and VpreA increased significantly in HTx patients after being indexed by BSA, while 3D LAEV and passive EV decreased significantly (P < 0.05). Moreover, the 3D LAEF, LA passive EF, and LA active EF all decreased significantly in HTx patients (P < 0.05). The 3D right atrial (RA) Vmax, Vmin, and VpreA increased significantly in HTx patients (P < 0.05), while the 3D RAEF and RA passive EF decreased significantly in HTx patients (P < 0.05). 3DE-derived LAVmax, LAVpreA, LA passive EV, LAEF, and LA passive EF were all lower than the corresponding 2D parameters. 3DE-derived RAVpreA, RA passive EV and RAEF were all lower than the corresponding 2D parameters. Atrial sizes and function assessed by 3DE- and 2DE-derived parameters, yield significantly discordant results in pediatric HTx patients. 3DE confirms significantly enlarged atrial sizes and decreased atrial functions in pediatric HTx patients.


Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Stehlik J, Kobashigawa J, Hunt SA, Reichenspurner H, Kirklin JK (2018) Honoring 50 years of clinical heart transplantation in circulation: in-depth state-of-the-art review. Circulation 137(1):71–87. https://doi.org/10.1161/CIRCULATIONAHA.117.029753
Kindel SJ, Hsu HH, Hussain T, Johnson JN, McMahon CJ, Kutty S (2017) Multimodality noninvasive imaging in the monitoring of pediatric heart transplantation. J Am Soc Echocardiogr 30(9):859–870. https://doi.org/10.1016/j.echo.2017.06.003
Dipchand AI, Rossano JW, Edwards LB et al (2015) The Registry of the International Society for Heart and Lung Transplantation: eighteenth official pediatric heart transplantation report-2015; focus theme: early graft failure. J Heart Lung Transpl 34(10):1233–1243. https://doi.org/10.1016/j.healun.2015.08.002
Rossano JW, Cherikh WS, Chambers DC et al (2018) The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: twenty-first pediatric heart transplantation report-2018; Focus theme: multiorgan transplantation. J Heart Lung Transpl 37(10):1184–1195. https://doi.org/10.1016/j.healun.2018.07.018
Badano LP, Miglioranza MH, Edvardsen T et al (2015) European Association of Cardiovascular Imaging/Cardiovascular Imaging Department of the Brazilian Society of Cardiology recommendations for the use of cardiac imaging to assess and follow patients after heart transplantation. Eur Heart J Cardiovasc Imaging 16(9):919–948. https://doi.org/10.1093/ehjci/jev139
To AC, Flamm SD, Marwick TH, Klein AL (2011) Clinical utility of multimodality LA imaging: assessment of size, function, and structure. JACC Cardiovasc Imaging 4(7):788–798. https://doi.org/10.1016/j.jcmg.2011.02.018
Boyd AC, Thomas L (2014) Left atrial volumes: two-dimensional, three-dimensional, cardiac magnetic resonance and computed tomography measurements. Curr Opin Cardiol 29(5):408–416. https://doi.org/10.1097/HCO.0000000000000087
Taniguchi N, Miyasaka Y, Suwa Y et al (2019) Usefulness of left atrial volume as an independent predictor of development of heart failure in patients with atrial fibrillation. Am J Cardiol 124(9):1430–1435. https://doi.org/10.1016/j.amjcard.2019.07.049
Sato T, Tsujino I, Ohira H et al (2015) Right atrial volume and reservoir function are novel independent predictors of clinical worsening in patients with pulmonary hypertension. J Heart Lung Transpl 34(3):414–423. https://doi.org/10.1016/j.healun.2015.01.984
Hoit BD (2014) Left atrial size and function: role in prognosis. J Am Coll Cardiol 63(6):493–505. https://doi.org/10.1016/j.jacc.2013.10.055
Land S, Niederer SA (2018) Influence of atrial contraction dynamics on cardiac function. Int J Numer Method Biomed Eng. https://doi.org/10.1002/cnm.2931
Poutanen T, Jokinen E, Sairanen H, Tikanoja T (2003) Left atrial and left ventricular function in healthy children and young adults assessed by three dimensional echocardiography. Heart 89(5):544–549. https://doi.org/10.1136/heart.89.5.544
Anwar AM, Geleijnse ML, Soliman OI, Nemes A, ten Cate FJ (2007) Left atrial Frank–Starling law assessed by real-time, three-dimensional echocardiographic left atrial volume changes. Heart 93(11):1393–1397. https://doi.org/10.1136/hrt.2006.099366
Poutanen T, Ikonen A, Vainio P, Jokinen E, Tikanoja T (2000) Left atrial volume assessed by transthoracic three dimensional echocardiography and magnetic resonance imaging: dynamic changes during the heart cycle in children. Heart 83(5):537–542. https://doi.org/10.1136/heart.83.5.537
Jenkins C, Bricknell K, Marwick TH (2005) Use of real-time three-dimensional echocardiography to measure left atrial volume: comparison with other echocardiographic techniques. J Am Soc Echocardiogr 18(9):991–997. https://doi.org/10.1016/j.echo.2005.03.027
Linden K, Goldschmidt F, Laser KT et al (2019) (2019) Left atrial volumes and phasic function in healthy children: reference values using real-time three-dimensional echocardiography. J Am Soc Echocardiogr 32(8):1036-1045.e9. https://doi.org/10.1016/j.echo.2019.03.018
Bech-Hanssen O, Pergola V, Al-Admawi M, Fadel BM, Di Salvo G (2016) Atrial function in heart transplant recipients operated with the bicaval technique. Scand Cardiovasc J 50(1):42–51. https://doi.org/10.3109/14017431.2015.1091946
Yeh J, Aiyagari R, Gajarski RJ, Zamberlan MC, Lu JC (2015) Left atrial deformation predicts pulmonary capillary wedge pressure in pediatric heart transplant recipients. Echocardiography 32(3):535–540. https://doi.org/10.1111/echo.12679
Debonnaire P, Joyce E, Hiemstra Y et al (2017) Left atrial size and function in hypertrophic cardiomyopathy patients and risk of new-onset atrial fibrillation. Circ Arrhythm Electrophysiol 10(2):e004052. https://doi.org/10.1161/CIRCEP.116.004052
Cao S, Zhou Q, Chen JL, Hu B, Guo RQ (2016) The differences in left atrial function between ischemic and idiopathic dilated cardiomyopathy patients: a two-dimensional speckle tracking imaging study. J Clin Ultrasound 44(7):437–445. https://doi.org/10.1002/jcu.22352
Liu S, Ma C, Ren W et al (2015) Regional left atrial function differentiation in patients with constrictive pericarditis and restrictive cardiomyopathy: a study using speckle tracking echocardiography. Int J Cardiovasc Imaging 31(8):1529–1536. https://doi.org/10.1007/s10554-015-0726-7
Chowdhury SM, Butts RJ, Hlavacek AM et al (2018) ECHOCARDIOGRAPHIC detection of increased ventricular diastolic stiffness in pediatric heart transplant recipients: a pilot study. J Am Soc Echocardiogr 31(3):342-348.e1. https://doi.org/10.1016/j.echo.2017.11.010
Behera SK, Trang J, Feeley BT, Levi DS, Alejos JC, Drant S (2008) The use of Doppler tissue imaging to predict cellular and antibody-mediated rejection in pediatric heart transplant recipients. Pediatr Transpl 12(2):207–214. https://doi.org/10.1111/j.1399-3046
Savage A, Hlavacek A, Ringewald J, Shirali G (2010) Evaluation of the myocardial performance index and tissue doppler imaging by comparison to near-simultaneous catheter measurements in pediatric cardiac transplant patients. J Heart Lung Transpl 29(8):853–858. https://doi.org/10.1016/j.healun.2010.03.014
Ingvarsson A, Werther Evaldsson A, Waktare J et al (2018) Normal reference ranges for transthoracic echocardiography following heart transplantation. J Am Soc Echocardiogr 31(3):349–360. https://doi.org/10.1016/j.echo.2017.11.003
Urbano-Moral JA, Arias-Godinez JA, Ahmad R et al (2013) Evaluation of myocardial mechanics with three-dimensional speckle tracking echocardiography in heart transplant recipients: comparison with two-dimensional speckle tracking and relationship with clinical variables. Eur Heart J Cardiovasc Imaging 14(12):1167–1173. https://doi.org/10.1093/ehjci/jet065
Chinali M, Esposito C, Grutter G et al (2017) Cardiac dysfunction in children and young adults with heart transplantation: a comprehensive echocardiography study. J Heart Lung Transpl 36(5):559–566. https://doi.org/10.1016/j.healun.2016.11.007
Harrington JK, Richmond ME, Woldu KL, Pasumarti N, Kobsa S, Freud LR (2019) Serial changes in right ventricular systolic function among rejection-free children and young adults after heart transplantation. J Am Soc Echocardiogr 32(8):1027-1035.e2. https://doi.org/10.1016/j.echo.2019.04.413
Zhu SS, Sun W, Qiao WH et al (2020) Real time three-dimensional echocardiographic quantification of left atrial volume in orthotopic heart transplant recipients: comparisons with cardiac magnetic resonance imaging. Echocardiography. https://doi.org/10.1111/echo.14792
Watanabe K, Schäfer M, Cassidy C, Miyamoto SD, Jone PN (2019) Right atrial function in pediatric heart transplant patients by echocardiographic strain measurements. Pediatr Transpl 23(3):e13383. https://doi.org/10.1111/petr.13383
Lu JC, Magdo HS, Yu S et al (2016) Usefulness of diastolic strain measurements in predicting elevated left ventricular filling pressure and risk of rejection or coronary artery vasculopathy in pediatric heart transplant recipients. Am J Cardiol 117(9):1533–1538. https://doi.org/10.1016/j.amjcard.2016.02.009
Meng X, Li Y, Li H, Lv X (2018) Three-dimensional echocardiography to evaluate right atrial volume and phasic function in pulmonary hypertension. Echocardiography 35(2):153–161. https://doi.org/10.1111/echo.13761
Zhang K, Braun A, von Koeckritz F et al (2019) Right heart remodeling in patients with end-stage alcoholic liver cirrhosis: speckle tracking point of view. J Clin Med. https://doi.org/10.3390/jcm8091285
Funding
This work was supported by the National Natural Science Foundation of China [grant numbers 81922033, 81727805, 81530056, 81671705].
Author information
Authors and Affiliations
Contributions
Conception and design of the study: ML, QL, LZ, MX. Acquisition of data: ML, HL, CW. Analysis and interpretation of data: ML, SW, HL, CW. Drafting the article: ML, QL, SW. Revising the article: ML, QL, SW, ND, YL, LZ, MX. Final approval of the article: ML, QL, SW, HL, CW, ND, YL, LZ, MX.
Corresponding authors
Ethics declarations
Conflict of interest
All the authors declare that they have no conflict iof interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Li, M., Lv, Q., Wang, S. et al. Assessment of biatrial function in clinically well pediatric bicaval heart transplantation patients by three-dimensional echocardiography. Int J Cardiovasc Imaging 37, 921–929 (2021). https://doi.org/10.1007/s10554-020-02067-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-020-02067-1