Abstract
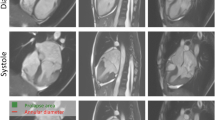
In bileaflet mitral valve prolapse (BMVP) systolic leaflet displacement creates a pocket of blood on the left ventricular (LV) side of the leaflets, but on the atrial side of the annulus. This blood is excluded from the LV end-systolic volume if the mitral valve annulus is used to determine the most basal extent of the LV. The purpose of this study is to describe the quantitative implications of defining the LV base on mitral regurgitant severity and LV systolic function in BMVP. In 30 consecutive patients (53% male, 58 ± 14 years) with BMVP, LV endocardial and epicardial borders were determined from SSFP images. The LV base at end-systole was defined by the “Functional” method (at the mitral valve annulus) or the “Anatomic” method (at the mitral valve leaflets). Regurgitant volume was the difference between the LV stroke volume and mean forward flow. LV myocardial strain measurements were determined from the short axis endocardial and epicardial borders. The “Functional” method resulted in higher regurgitant volumes (mean difference: 22 ml, range 0–40 ml) and higher ejection fractions (mean difference: 9%, range 0–21%). The correlation between LV end-diastolic volume and regurgitant volume was better with the “Functional” method (r = 0.79, p < 0.0001) than the “Anatomic” method (r = 0.67, p < 0.0001). The correlation between global myocardial radial strain and LV EF was better with the “Functional” method (r = 0.86, p < 0.0001) than the “Anatomic” method (r = 0.68, p < 0.0001). In BMVP, the base of the LV should be defined at the level of the mitral valve annulus so that regurgitant volume most accurately reflects the functional significance of the mitral valve disease and LVEF most accurately reflects global systolic LV function. Defining the basal extent of the LV at the mitral valve leaflets leads to substantially lower regurgitant volumes and lower ejection fractions that could have important clinical consequences.



Similar content being viewed by others
References
Uretsky S, Argulian E, Narula J, Wolff SD (2018) Use of cardiac magnetic resonance imaging in assessing mitral regurgitation: current evidence. J Am Coll Cardiol 71(5):547–563
Schulz-Menger J, Bluemke DA, Bremerich J, Flamm SD, Fogel MA, Friedrich MG, Kim RJ, von Knobelsdorff-Brenkenhoff F, Kramer CM, Pennell DJ et al (2013) Standardized image interpretation and post processing in cardiovascular magnetic resonance: Society for Cardiovascular Magnetic Resonance (SCMR) board of trustees task force on standardized post processing. J Cardiovasc Magn Reson 15:35
Vincenti G, Masci PG, Rutz T, De Blois J, Prsa M, Jeanrenaud X, Schwitter J, Monney P (2017) Impact of bileaflet mitral valve prolapse on quantification of mitral regurgitation with cardiac magnetic resonance: a single-center study. J Cardiovasc Magn Reson 19(1):56
Uretsky S, Gillam L, Lang R, Chaudhry FA, Argulian E, Supariwala A, Gurram S, Jain K, Subero M, Jang JJ et al (2015) Discordance between echocardiography and MRI in the assessment of mitral regurgitation severity: a prospective multicenter trial. J Am Coll Cardiol 65(11):1078–1088
Uretsky S, Supariwala A, Nidadovolu P, Khokhar SS, Comeau C, Shubayev O, Campanile F, Wolff SD (2010) Quantification of left ventricular remodeling in response to isolated aortic or mitral regurgitation. J Cardiovasc Magn Reson 12:32
Cameli M, Lisi M, Mondillo S, Padeletti M, Ballo P, Bigio E, Marchetti L, Biagioli B (2011) Prediction of stroke volume by global left ventricular longitudinal strain in patients undergoing assessment for cardiac transplantation. J Crit Care 26(4):433e413–433e420
Han Y, Peters DC, Salton CJ, Bzymek D, Nezafat R, Goddu B, Kissinger KV, Zimetbaum PJ, Manning WJ, Yeon SB (2008) Cardiovascular magnetic resonance characterization of mitral valve prolapse. JACC Cardiovasc Imaging 1(3):294–303
Uretsky S, Chaudhry FA, Gillam L, Gurram S, Bonda SL, Ponnam H, Bader E, Thota N, Cohen R, Supariwala A et al (2013) A novel technique to quantify the instantaneous mitral regurgitant rate. J Cardiovasc Magn Reson 15:74
Myerson SG, d'Arcy J, Christiansen JP, Dobson LE, Mohiaddin R, Francis JM, Prendergast B, Greenwood JP, Karamitsos TD, Neubauer S (2016) Determination of clinical outcome in mitral regurgitation with cardiovascular magnetic resonance quantitation. Circulation 133:2287–2296
Penicka M, Vecera J, Mirica DC, Kotrc M, Kockova R, Van Camp G (2018) Prognostic implications of magnetic resonance-derived quantification in asymptomatic patients with organic mitral regurgitation: comparison with doppler echocardiography-derived integrative approach. Circulation 137(13):1349–1360
Paknezhad M, Marchesseau S, Brown MS (2016) Automatic basal slice detection for cardiac analysis. J Med Imaging (Bellingham) 3(3):034004
Hundley WG, Meshack BM, Willett DL, Sayad DE, Lange RA, Willard JE, Landau C, Hillis LD, Peshock RM (1996) Comparison of quantitation of left ventricular volume, ejection fraction, and cardiac output in patients with atrial fibrillation by cine magnetic resonance imaging versus invasive measurements. Am J Cardiol 78(10):1119–1123
Uretsky S, Shah DJ, Lasam G, Horgan S, Debs D, Wolff SD (2020) Usefulness of mitral regurgitant volume quantified using magnetic resonance imaging to predict left ventricular remodeling after mitral valve "correction". Am J Cardiol 125(11):1666–1672
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28(1):1–39
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Both authors Ryan Wolff and Seth Uretsky, (1) made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data; or the creation of new software used in the work; (2) drafted the work or revised it critically for important intellectual content; (3) approved the version to be published; and (4) agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflics of interest
The authors declare that they have no conflics of interest.
Ethics approval
Waiver of consent was obtained from IRB.
Informed consent
Waiver of consent was obtained from IRB.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wolff, R., Uretsky, S. Defining the left ventricular base in mitral valve prolapse: impact on systolic function and regurgitation. Int J Cardiovasc Imaging 36, 2221–2227 (2020). https://doi.org/10.1007/s10554-020-01927-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-020-01927-0