Abstract
The healing process, occurring after intra-cardiac and intra-vascular device implantation, starts with fibrin condensation and attraction of inflammatory cells, followed by the formation of fibrous tissue that slowly covers the device. The duration of this process is variable and may be incomplete, which can lead to thrombus formation, dislodgement of the device or stenosis. To better understand this process and the neotissue formation, animal models were developed: small (rats and rabbits) and large (sheep, pigs, dogs and baboons) animal models for intra-vascular device implantation; sheep and pigs for intra-cardiac device implantation. After intra-vascular and intra-cardiac device implantation in these animal models, in vitro techniques, i.e. histology, which is the gold standard and scanning electron microscopy, were used to assess the device coverage, characterize the cell constitution and detect complications such as thrombosis. In humans, optical coherence tomography and intra-vascular ultrasounds are both invasive modalities used after stent implantation to assess the structure of the vessels, atheroma plaque and complications. Non-invasive techniques (computed tomography and magnetic resonance imaging) are in development in humans and animal models for tissue characterization (fibrosis), device remodeling evaluation and device implantation complications (thrombosis and stenosis). This review aims to (1) present the experimental models used to study this process on cardiac devices; (2) focus on the in vitro techniques and invasive modalities used currently in humans for intra-vascular and intra-cardiac devices and (3) assess the future developments of non-invasive techniques in animal models and humans for intra-cardiac devices.



Similar content being viewed by others
References
Dahan N, Sarig U, Bronshtein T, Baruch L, Karram T, Hoffman A et al (2017) Dynamic autologous reendothelialization of small-caliber arterial extracellular matrix: a preclinical large animal study. Tissue Eng Part A 23:69–79. https://doi.org/10.1089/ten.tea.2016.0126
Liu J, Peng Y, Lai J, Gao W, Song A, Zhang G (2017) Fluid upstream shear stress of rabbit aortic stenosis inhibits neointimal hyperplasia by promoting endothelization after balloon injury. BMC Cardiovasc Disord 17:273. https://doi.org/10.1186/s12872-017-0690-3
Foth R, Quentin T, Michel-Behnke I, Vogt M, Kriebel T, Kreischer A et al (2009) Immunohistochemical characterization of neotissues and tissue reactions to septal defect-occlusion devices. Circ Cardiovasc Interv 2:90–96. https://doi.org/10.1161/circinterventions.108.810507
Sigler M, Jux C (2007) Biocompatibility of septal defect closure devices. Heart 93:444–449. https://doi.org/10.1136/hrt.2006.098103
Pislaru SV, Harbuzariu A, Agarwal G, Witt T, Gulati R, Sandhu NP et al (2006) Magnetic forces enable rapid endothelialization of synthetic vascular grafts. Circulation 114:314–318. https://doi.org/10.1161/circulationaha.105.001446
Syedain Z, Reimer J, Schmidt J, Lahti M, Berry J, Bianco R et al (2015) 6-month aortic valve implantation of an off-the-shelf tissue-engineered valve in sheep. Biomaterials 73:175–184. https://doi.org/10.1016/j.biomaterials.2015.09.016
Cheneau E, John MC, Fournadjiev J, Chan RC, Kim HS, Leborgne L et al (2003) Time course of stent endothelialization after intravascular radiation therapy in rabbit iliac arteries. Circulation 107:2153–2158. https://doi.org/10.1161/01.CIR.0000062648.39025.09
Finn AV, Kolodgie FD, Harnek J, Guerrero LJ, Acampado E, Tefera K (2005) Differential response of delayed healing and persistent inflammation at sites of overlapping sirolimus- or paclitaxel-eluting stents. Circulation 112:270–278. https://doi.org/10.1161/circulationaha.104.508937
Virmani R, Kolodgie FD, Farb A, Lafont A (2003) Drug eluting stents: are human and animal studies comparable? Heart Br Card Soc 89:133–138
Takano M, Yamamoto M, Inami S, Murakami D, Seimiya K, Ohba T et al (2008) Long-term follow-up evaluation after sirolimus-eluting stent implantation by optical coherence tomography. J Am Coll Cardiol 51:968–969
Chen F, Zhao X, Zheng X, Chen S, Xu R, Qin Y (2011) Incomplete endothelialization and late dislocation after implantation of an Amplatzer septal occluder device. Circulation 124:188–189. https://doi.org/10.1161/circulationaha.110.991836
Nguyen AK, Palafox BA, Starr JP, Gates RN, Berdjis F (2016) Endocarditis and incomplete endothelialization 12 years after Amplatzer septal occluder deployment. Tex Heart Inst J 43:227–231. https://doi.org/10.14503/THIJ-14-4949
Farb A, Weber DK, Kolodgie FD, Burke AP, Virmani R (2002) Morphological predictors of restenosis after coronary stenting in humans. Circulation 105:2974–2980. https://doi.org/10.1161/01.CIR.0000019071.72887.BD
Deutsch M, Meinhart J, Vesely M, Fischlein T, Groscurth P, von Oppell U et al (1997) In vitro endothelialization of expanded polytetrafluoroethylene grafts: a clinical case report after 41 months of implantation. J Vasc Surg 25:757–763
Pendyala LK, Yin X, Li J, Chen JP, Chronos N, Hou D (2009) The first-generation drug-eluting stents and coronary endothelial dysfunction. JACC Cardiovasc Interv 2:1169–1177. https://doi.org/10.1016/j.jcin.2009.10.004
Li S, Gai L, Yang T, Zhang L, Xu X, Bai Q et al (2013) Evaluation of long-term follow-up with neointimal coverage and stent apposition after sirolimus-eluting stent implantation by optical coherence tomography. Catheter Cardiovasc Interv 81:768–775. https://doi.org/10.1002/ccd.24497
Gonzalo N, Barlis P, Serruys PW, Garcia-Garcia HM, Onuma Y, Ligthart J et al (2009) Incomplete stent apposition and delayed tissue coverage are more frequent in drug-eluting stents implanted during primary percutaneous coronary intervention for ST-segment elevation myocardial infarction than in drug-eluting stents implanted for stable/unstable angina. JACC Cardiovasc Interv 2:445–452. https://doi.org/10.1016/j.jcin.2009.01.012
Musick KM, Coffey AC, Irazoqui PP (2010) Sensor to detect endothelialization on an active coronary stent. Biomed Eng OnLine 9:67. https://doi.org/10.1186/1475-925X-9-67
Foin N, Gutierrez-Chico JL, Nakatani S, Torii R, Bourantas CV, Sen S et al (2014) Incomplete stent apposition causes high shear flow disturbances and delay in neointimal coverage as a function of strut to wall detachment distance: implications for the management of incomplete stent apposition. Circ Cardiovasc Interv 7:180–189. https://doi.org/10.1161/circinterventions.113.000931
Chan AH, Tan RP, Michael PL, Lee BS, Vanags LZ, Ng MKC et al (2017) Evaluation of synthetic vascular grafts in a mouse carotid grafting model. PLOS ONE 12:e0174773. https://doi.org/10.1371/journal.pone.0174773
Zilla P, Bezuidenhout D, Human P (2007) Prosthetic vascular grafts: wrong models, wrong questions and no healing. Biomaterials 28:5009–5027. https://doi.org/10.1016/j.biomaterials.2007.07.017
Byrom MJ, Bannon PG, White GH, Ng MKC (2010) Animal models for the assessment of novel vascular conduits. J Vasc Surg 52:176–195. https://doi.org/10.1016/j.jvs.2009.10.080
Mirza A, Hyvelin JM, Rochefort GY, Lermusiaux P, Antier D, Awede B et al (2008) Undifferentiated mesenchymal stem cells seeded on a vascular prosthesis contribute to the restoration of a physiologic vascular wall. J Vasc Surg 47:1313–1321. https://doi.org/10.1016/j.jvs.2007.12.038
Wang TJ, Yang YJ, Xu B, Zhang Q, Jin C, Tang Y et al (2012) Atorvastatin accelerates both neointimal coverage and re-endothelialization after sirolimus-eluting stent implantation in a porcine model. Circ J 76:2561–2571. https://doi.org/10.1253/circj.CJ-12-0468
Liu HT, Li F, Wang WY, Li XJ, Liu YM, Wang RA et al (2010) Rapamycin inhibits re-endothelialization after percutaneous coronary intervention by impeding the proliferation and migration of endothelial cells and inducing apoptosis of endothelial progenitor cells. Tex Heart Inst J 37:194–201
Prati F, Romagnoli E, Valgimigli M, Burzotta F, De Benedictis M, Ramondo A et al (2014) Randomized comparison between 3-month Cre8 DES vs. 1-month Vision/Multilink8 BMS neointimal coverage assessed by OCT evaluation: The DEMONSTRATE study. Int J Cardiol 176:904–909. https://doi.org/10.1016/j.ijcard.2014.08.031
Ma X, Hibbert B, Dhaliwal B, Seibert T, Chen YX, Zhao X et al (2010) Delayed re-endothelialization with rapamycin-coated stents is rescued by the addition of a glycogen synthase kinase-3β inhibitor. Cardiovasc Res 86:338–345. https://doi.org/10.1093/cvr/cvq047
Tang C, Wang G, Wu X, Li Z, Shen Y, Lee JC et al (2011) The impact of vascular endothelial growth factor-transfected human endothelial cells on endothelialization and restenosis of stainless steel stents. J Vasc Surg 53:461–471. https://doi.org/10.1016/j.jvs.2010.08.020
Toma C, Fisher A, Wang J, Chen X, Grata M, Leeman J et al (2011) Vascular endoluminal delivery of mesenchymal stem cells using acoustic radiation force. Tissue Eng Part A 17:1457–1464. https://doi.org/10.1089/ten.tea.2010.0539
Larsen K, Cheng C, Tempel D, Parker S, Yazdani S, den Dekker WK et al (2012) Capture of circulatory endothelial progenitor cells and accelerated re-endothelialization of a bio-engineered stent in human ex vivo shunt and rabbit denudation model. Eur Heart J 33:120–128. https://doi.org/10.1093/eurheartj/ehr196
Mertens ME, Koch S, Schuster P, Wehner J, Wu Z, Gremse F et al (2015) USPIO-labeled textile materials for non-invasive MR imaging of tissue-engineered vascular grafts. Biomaterials 39:155–163. https://doi.org/10.1016/j.biomaterials.2014.10.076
Koobatian MT, Row S, Smith RJ Jr, Koenigsknecht C, Andreadis ST, Swartz DD (2016) Successful endothelialization and remodeling of a cell-free small-diameter arterial graft in a large animal model. Biomaterials 76:344–358. https://doi.org/10.1016/j.biomaterials.2015.10.020
Fukunishi T, Best CA, Sugiura T, Shoji T, Yi T, Udelsman B et al (2016) Tissue-engineered small diameter arterial vascular grafts from cell-free nanofiber PCL/Chitosan scaffolds in a sheep model. PLOS ONE 11(7):158555. https://doi.org/10.1371/journal.pone.0158555.
Attizzani G, Bezerra H, Chamié D, Fujino Y, Spognardi A, Stanley J et al (2012) Serial evaluation of vascular response after implantation of a new sirolimus-eluting stent with bioabsorbable polymer [MISTENT]: an optical coherence tomography and histopathological study. J Invasive Cardiol 24(11):560–568
Ruiter MS, Doornbos A, de Waard V, de Winter RJ, Attevelt NJM, Steendam R et al (2016) Long-term effect of stents eluting 6-mercaptopurine in porcine coronary arteries. J Negat Results Biomed 15:15–20. https://doi.org/10.1186/s12952-016-0063-y
Wittchow E, Adden N, Riedmüller J, Savard C, Waksman R, Braune M (2013) Bioresorbable drug-eluting magnesium-alloy scaffold: design and feasibility in a porcine coronary model. EuroIntervention 8:1441–1450. https://doi.org/10.4244/EIJV8I12A218
Zhang B, Zheng B, Wang X, Shi Q, Jia J, Huo Y et al (2017) Polymer-free dual drug-eluting stents evaluated in a porcine model. BMC Cardiovasc Disord 17:222. https://doi.org/10.1186/s12872-017-0654-7
Koppara T, Joner M, Bayer G, Steigerwald K, Diener T, Wittchow E (2012) Histopathological comparison of biodegradable polymer and permanent polymer based sirolimus eluting stents in a porcine model of coronary stent implantation. Thromb Haemost 107:1161–1171. https://doi.org/10.1160/TH12-01-0043
Rotmans JI, Heyligers JM, Verhagen HJ, Velema E, Nagtegaal MM, Kleijn DP et al (2005) In vivo cell seeding with anti-CD34 antibodies successfully accelerates endothelialization but stimulates intimal hyperplasia in porcine arteriovenous expanded polytetrafluoroethylene grafts. Circulation 112:12–18. https://doi.org/10.1161/circulationaha.104.504407
Farooq V, Serruys PW, Heo JH, Gogas BD, Onuma Y, Perkins LE et al (2013) Intracoronary optical coherence tomography and histology of overlapping everolimus-eluting bioresorbable vascular scaffolds in a porcine coronary artery model. JACC Cardiovasc Interv 6:523–532. https://doi.org/10.1016/j.jcin.2012.12.131
Jordan SW, Haller CA, Sallach RE, Apkarian RP, Hanson SR, Chaikof EL (2007) The effect of a recombinant elastin-mimetic coating of an ePTFE prosthesis on acute thrombogenicity in a baboon arteriovenous shunt. Biomaterials 28:1191–1197. https://doi.org/10.1016/j.biomaterials.2006.09.048
Itoh M, Nakayama K, Noguchi R, Kamohara K, Furukawa K, Uchihashi K et al (2015) Scaffold-free tubular tissues created by a Bio-3D printer undergo remodeling and endothelialization when implanted in rat aortae. PLOS ONE 10:e0136681. https://doi.org/10.1371/journal.pone.0136681
Aubin H, Mas-Moruno C, Iijima M, Schütterle N, Steinbrink M, Assmann A et al. Customized interface biofunctionalization of decellularized extracellular matrix: toward enhanced endothelialization. Tissue Eng Part C Methods 22 (2016) 496–508. https://doi.org/10.1089/ten.tec.2015.0556
Clowes AW, Gown AM, Hanson SR, Reidy MA (1985) Mechanisms of arterial graft failure. Role of cellular proliferation in early healing of PTFE prostheses. Am J Pathol 118:43–54
Lin PH, Chronos NA, Marijianowski MM, Chen C, Conklin B, Bush RL et al. Carotid stenting using heparin-coated balloon-expandable stent reduces intimal hyperplasia in a baboon model. J Surg Res 112 (2003) 84–90. https://doi.org/10.1016/S0022-4804(03)00124-0
Vincentelli A, Wautot F, Juthier F, Fouquet O, Corseaux D, Marechaux S et al. In vivo autologous recellularization of a tissue-engineered heart valve: Are bone marrow mesenchymal stem cells the best candidates? J Thorac Cardiovasc Surg 134 (2007) 424–432. https://doi.org/10.1016/j.jtcvs.2007.05.005
Schmitt B, Spriestersbach H, h-Icí DO, Radtke T, Bartosch M, Peters H et al (2016) Percutaneous pulmonary valve replacement using completely tissue-engineered off-the-shelf heart valves: six-month in vivo functionality and matrix remodelling in sheep. EuroIntervention 12:62–70. https://doi.org/10.4244/EIJV12I1A12
Hof A, Raschke S, Baier K, Nehrenheim L, Selig JI, Schomaker M et al. Challenges in developing a reseeded, tissue-engineered aortic valve prosthesis. Eur J Cardiothorac Surg 50 (2016) 446–455. https://doi.org/10.1093/ejcts/ezw057
Milewski K, Fiszer R, Buszman PP, Węglarz P, Janas A, Krauze A et al (2017) Temporal healing patterns and coverage dynamics after new polish transcatheter PFO occluder implantation in a swine. Kardiol Pol 75:907–913. https://doi.org/10.5603/KP.a2017.0117
Whited BM, Hofmann MC, Lu P, Xu Y, Rylander CG, Wang G et al. Dynamic, nondestructive imaging of a bioengineered vascular graft endothelium. PLoS ONE 8 (2013) e61275. https://doi.org/10.1371/journal.pone.0061275
Melchiorri AJ, Bracaglia LG, Kimerer LK, Hibino N, Fisher JP. In vitro endothelialization of biodegradable vascular grafts via endothelial progenitor cell seeding and maturation in a tubular perfusion system bioreactor. Tissue Eng Part C Methods 22 (2016) 663–670. https://doi.org/10.1089/ten.tec.2015.0562
Hsiao ST, Spencer T, Boldock L, Prosseda SD, Xanthis I, Tovar-Lopez FJ et al. Endothelial repair in stented arteries is accelerated by inhibition of Rho-associated protein kinase. Cardiovasc Res 112 (2016) 689–701. https://doi.org/10.1093/cvr/cvw210
Eberl T, Siedler S, Schumacher B, Zilla P, Schlaudraff K (1992) R. Fasol. Experimental in vitro endothelialization of cardiac valve leaflets. Ann Thorac Surg 53:487–492
Voges I, Bräsen JH, Entenmann A, Scheid M, Scheewe J, Fischer G et al. Adverse results of a decellularized tissue-engineered pulmonary valve in humans assessed with magnetic resonance imaging. Eur J Cardiothorac Surg 44 (2013) 272–279. https://doi.org/10.1093/ejcts/ezt328
Aoki J, Serruys PW, van Beusekom H, Ong ATL, McFadden EP, Sianos G et al. Endothelial progenitor cell capture by stents coated with antibody against CD34. J Am Coll Cardiol 45 (2005) 1574–1579. https://doi.org/10.1016/j.jacc.2005.01.048
Kar S, Hou D, Jones R, Werner D, Swanson L, Tischler B et al. Impact of Watchman and Amplatzer devices on left atrial appendage adjacent structures and healing response in a canine model. JACC Cardiovasc Interv 7 (2014) 801–809. https://doi.org/10.1016/j.jcin.2014.03.003
Hoang V, Grounds J, Pham D, Virani S, Hamzeh I, Qureshi AM et al. The role of intracoronary plaque imaging with intravascular ultrasound, optical coherence tomography, and near-infrared spectroscopy in patients with coronary artery disease. Curr Atheroscler Rep 18 18 (2016) 57. https://doi.org/10.1007/s11883-016-0607-0
Vasquez A, Mistry N, Singh J. Impact of Intravascular Ultrasound in Clinical Practice. Interv Cardiol Rev.9 (2014) 156. https://doi.org/10.15420/icr.2014.9.3.156
Erglis A, Narbute I (2014) Intravascular Ultrasound-based Imaging Modalities for Tissue Characterisation. Interv Cardiol Rev 9:151. https://doi.org/10.15420/icr.2014.9.3.151
Schiele F, Meneveau N, Vuillemenot A, Zhang DD, Gupta S, Mercier M et al (1998) Impact of intravascular ultrasound guidance in stent deployment on 6-month restenosis rate: a multicenter, randomized study comparing two strategies—with and without intravascular ultrasound guidance. J Am Coll Cardiol 32:320–328
Tearney GJ, Regar E, Akasaka T, Adriaenssens T, Barlis P, Bezerra HG et al. Consensus standards for acquisition, measurement, and reporting of intravascular optical coherence tomography studies. J Am Coll Cardiol 59 (2012) 1058–1072. https://doi.org/10.1016/j.jacc.2011.09.079
Barlis P, Regar E, Serruys PW, Dimopoulos K, van der Giessen WJ, van Geuns RJ et al. An optical coherence tomography study of a biodegradable vs. durable polymer-coated limus-eluting stent: a LEADERS trial sub-study. Eur Heart J 31 (2010) 165–176. https://doi.org/10.1093/eurheartj/ehp480
Murase S, Suzuki Y, Yamaguchi T, Matsuda O, Murata A, Ito T. The relationship between re-endothelialization and endothelial function after DES implantation: Comparison between paclitaxcel eluting stent and zotarolims eluting stent. Catheter Cardiovasc Interv 83 (2014) 412–417. https://doi.org/10.1002/ccd.25140
Lehtinen T, Kiviniemi TO, Ylitalo A, Mikkelsson J, Airaksinen JKE, Karjalainen PP (2012) Early vascular healing after endothelial progenitor cell capturing stent implantation. J Invasive Cardiol 24:631–635
Bonnema GT, Cardinal KO, Williams SK, Barton JK (2008) An automatic algorithm for detecting stent endothelialization from volumetric optical coherence tomography datasets. Phys Med Biol 53:3083–3098. https://doi.org/10.1088/0031-9155/53/12/001
Kobayashi Y, Okura H, Kume T, Yamada R, Kobayashi Y, Fukuhara K et al (2014) Impact of target lesion coronary calcification on stent expansion. Circ J 78:2209–2214
Guagliumi G, Sirbu V, Musumeci G, Gerber R, Biondi-Zoccai G, Ikejima H et al (2012) Examination of the in vivo mechanisms of late drug-eluting stent thrombosis. JACC Cardiovasc Interv 5:12–20. https://doi.org/10.1016/j.jcin.2011.09.018
Gurjarpadhye AA, DeWitt MR, Xu Y, Wang G, Rylander MN, Rylander CG (2015) Dynamic assessment of the endothelialization of tissue-engineered blood vessels using an optical coherence tomography catheter-based fluorescence imaging system. Tissue Eng Part C Methods 21:758–766. https://doi.org/10.1089/ten.tec.2014.0345
Fayol D, Le Visage C, Ino J, Gazeau F, Letourneur D, Wilhelm C (2013) Design of biomimetic vascular grafts with magnetic endothelial patterning. Cell Transplant 22:2105–2118. https://doi.org/10.3727/096368912X661300
Bucciarelli-Ducci C, Baritussio A, Auricchio A. Cardiac MRI anatomy and function as a substrate for arrhythmias. EP Eur 18 (2016) 130–135. https://doi.org/10.1093/europace/euw357
Haaf P, Garg P, Messroghli DR, Broadbent DA, Greenwood JP, Plein S. Cardiac T1 mapping and extracellular volume in clinical practice: a comprehensive review. J Cardiovasc Magn Reson 18 (2017) 89. https://doi.org/10.1186/s12968-016-0308-4
Captur G, Manisty C, Moon JC. Cardiac MRI evaluation of myocardial disease. Heart 102 (2016) 1429–1435. https://doi.org/10.1136/heartjnl-2015-309077
Gyöngyösi M, Winkler J, Ramos I, Do QT, Firat H, McDonald K et al. Myocardial fibrosis: biomedical research from bench to bedside: myocardial fibrosis: biomedical research from bench to bedside. Eur J Heart Fail 19 (2017) 177–191. https://doi.org/10.1002/ejhf.696
Berliner JI, Kino A, Carr JC, Bonow RO, Choudhury L. Cardiac computed tomographic imaging to evaluate myocardial scarring/fibrosis in patients with hypertrophic cardiomyopathy: a comparison with cardiac magnetic resonance imaging. Int J Cardiovasc Imaging 29 (2013) 191–197. https://doi.org/10.1007/s10554-012-0048-y
Ghosn MG, Shah DJ. Important advances in technology and unique applications related to cardiac magnetic resonance imaging. Methodist DeBakey Cardiovasc J 10 (2014) 159–162. https://doi.org/10.14797/mdcj-10-3-159
Graham-Brown MPM, Patel AS, Stensel DJ, March DS, Marsh AM, McAdam J et al (2017) Imaging of myocardial fibrosis in patients with end-stage renal disease: current limitations and future possibilities. BioMed Res Int. https://doi.org/10.1155/2017/5453606
Puntmann VO, Peker E, Chandrashekhar Y, Nagel E. T1 Mapping in characterizing myocardial disease: a comprehensive review. Circ Res 119 (2016) 277–299. https://doi.org/10.1161/circresaha.116.307974
Lapierre C, Hugues N, Dahdah N, Déry J, Raboisson MJ, Miró J. Long-term follow-up of large atrial septal occluder (Amplatzer device) with cardiac MRI in a pediatric population. Am J Roentgenol 199 (2012) 1136–1141. https://doi.org/10.2214/AJR.12.8617
Maron BJ, Maron MS (2016) The remarkable 50 years of imaging in HCM and how it has changed diagnosis and management. JACC Cardiovasc Imaging 9:858–872. https://doi.org/10.1016/j.jcmg.2016.05.003
Mahida S, Sacher F, Dubois R, Sermesant M, Bogun F, Haissaguerre M et al. Cardiac imaging in patients with ventricular tachycardia. Circulation 136 (2017) 2491–2507. https://doi.org/10.1161/circulationaha.117.029349
Kwon W, Choi J, Kim JY, Kim SY, Yoon J, Choe KH et al (2012) In-stent area stenosis on 64-slice multi-detector computed tomography coronary angiography: optimal cutoff value for minimum lumen cross-sectional area of coronary stents compared with intravascular ultrasound. Int J Cardiovasc Imaging 28:21–31. https://doi.org/10.1007/s10554-012-0057-x
Motoyama S, Ito H, Sarai M, Nagahara Y, Miyajima K, Matsumoto R et al. Ultra-high-resolution computed tomography angiography for assessment of coronary artery stenosis. Circ J 82 (2018) 1844–1851. https://doi.org/10.1253/circj.CJ-17-1281
Cochet H, Iriart X, Sridi S, Camaioni C, Corneloup O, Montaudon M et al (2018) Left atrial appendage patency and device-related thrombus after percutaneous left atrial appendage occlusion: a computed tomography study. Eur Heart J - Cardiovasc Imaging 19:1351–1361. https://doi.org/10.1093/ehjci/jey010.
Marini D, Ou P, Boudjemline Y, Kenny D, Bonnet D, Agnoletti G (2012) Midterm results of percutaneous closure of very large atrial septal defects in children: role of multislice computed tomography. EuroIntervention 7:1428–1434. https://doi.org/10.4244/EIJV7I12A223
Maresca D, Correia M, Villemain O, Bizé A, Sambin L, Tanter M et al (2018) Noninvasive imaging of the coronary vasculature using ultrafast ultrasound. JACC Cardiovasc Imaging 11:798–808. https://doi.org/10.1016/j.jcmg.2017.05.021
Strachinaru M, Bosch JG, van Dalen BM, van Gils L, van der Steen AFW, de Jong N et al (2017) Cardiac shear wave elastography using a clinical ultrasound system. Ultrasound Med Biol 43:1596–1606. https://doi.org/10.1016/j.ultrasmedbio.2017.04.012
Brekke B, Nilsen LCL, Lund J, Torp H, Bjastad T, Amundsen BH et al (2014) Ultra-high frame rate tissue Doppler imaging. Ultrasound Med Biol 40:222–231. https://doi.org/10.1016/j.ultrasmedbio.2013.09.012
Acknowledgements
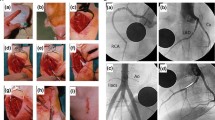
The figures were reprinted: Fig. 1: reprinted from Circulation: Cardiovascular Interventions 2009;2:90–96, by Foth et al., Immunohistochemical characterization of neotissues and tissue reactions to septal defect-occlusion devices, Figure n°1, Copyright 2009, with permission from Wolters Kluwer Health, Inc. Fig. 2: reprinted from JACC: Cardiovascular Interventions 2013;6[5]:523−32, by Farooq et al., Intracoronary optical coherence tomography and histology of overlapping everolimus-eluting bioresorbable vascular scaffolds in a porcine coronary artery model the potential implications for clinical practice, Figure n°7, Copyright 2013, with permission from Elsevier Inc. Fig. 3: reprinted from JACC: Cardiovascular Interventions 2012;5[1]:12–20, by Guagliumi et al., Examination of the in vivo mechanisms of late drug-eluting stent thrombosis-Findings from optical coherence tomography and intravascular ultrasound imaging, Figure n°1, Copyright 2012, with permission from Elsevier Inc.
Funding
This study received financial support from the French Government as part of the “Investments of the Future” program managed by the National Research Agency (ANR), Grant reference ANR-10-IAHU-04.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The manuscript does not contain clinical studies or patient data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Perdreau, E., Jalal, Z., Walton, R.D. et al. Assessment of the healing process after percutaneous implantation of a cardiovascular device: a systematic review. Int J Cardiovasc Imaging 36, 385–394 (2020). https://doi.org/10.1007/s10554-019-01734-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-019-01734-2