Abstract
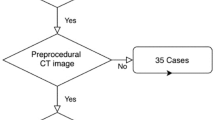
Preoperative optimal selection of the occluder size is crucial in percutaneous left atrial appendage (LAA) occlusion, and the maximal width of the LAA orifice is the main reference index, however it can not fully meet the practical operation requirements. We retrospectively analyzed three-dimensional (3D) transesophageal echocardiography (TEE) and computed tomography (CT) imaging dataset of the 41 patients who underwent LAA occlusion with LAmbre™ system. The LAA orifice parameters were overall evaluated to determine their role in device size selection. Eight LAA 3D models of the four cases who had been replaced their device during the procedure based on TEE and CT were printed out to verify the optimal parameter decision strategy. There was a significant concordance of the results between 3D TEE and CT in the LAA orifice evaluation. The correlations between the perimeter and maximal width measurements by 3D TEE and the closure disk of the device were stronger than that between the area measurements and the closure disk (r = 0.93, 0.95, 0.86, respectively and p < 0.001 all), and the result was similar to that by CT (r = 0.92, 0.93, 0.84, respectively and p < 0.001 all). The ratios of the maximal width to the minimal width of the four cases were all > 1.4, however the rest 37 cases were all ≤ 1.4. Based on the comprehensive assessment of the LAA orifice perimeter and maximal width of the 3D printed models, the experiments were all succeed just for one try. The LAA orifice perimeter of 3D printed model based on 3D TEE may help in choosing the optimal device size of LAmbre™, especially for the LAA with flater ostial shape.






Similar content being viewed by others
Abbreviations
- LAA:
-
Left atrial appendage
- 3D:
-
Three-dimensional
- TEE:
-
Transesophageal echocardiography
- DICOM:
-
Digital imaging and communications in medicine
- CT:
-
Computed tomography
References
Belgaid DR, Khan Z, Zaidi M, Hobbs A (2016) Prospective randomized evaluation of the watchman left atrial appendage closure device in patients with atrial fibrillation versus long-term warfarin therapy: the PREVAIL trial. Int J Cardiol 219:177–179. https://doi.org/10.1016/j.ijcard.2016.06.041
MJ Ramos Ramirez, Young B, Harjai K, Mascarenhas V, Vijayaraman P (2017) Left atrial appendage occlusion: in review. J Interv Cardiol 30:448–456. https://doi.org/10.1111/joic.12410
Nishimura M, Sab S, Reeves RR, Hsu JC (2018) Percutaneous left atrial appendage occlusion in atrial fibrillation patients with a contraindication to oral anticoagulation: a focused review. Europace 9:1412–1419. https://doi.org/10.1093/europace/eux313
Beigel R, Wunderlich NC, Ho SY, Arsanjani R, Siegel RJ (2014) The left atrial appendage: anatomy, function, and noninvasive evaluation. JACC Cardiovasc Imaging 7:1251–1265. https://doi.org/10.1016/j.jcmg.2014.08.009
Otton JM, Spina R, Sulas R, Subbiah RN, Jacobs N, Muller DW, Gunalingam B (2015) Left atrial appendage closure guided by personalized 3d-printed cardiac reconstruction. JACC Cardiovasc Interv 8:1004–1006. https://doi.org/10.1016/j.jcin.2015.03.015
Goitein O, Fink N, Guetta V, Beinart R, Brodov Y, Konen E, Goitein D, Di Segni E, Grupper A, Glikson M (2017) Printed MDCT 3D models for prediction of left atrial appendage (LAA) occluder device size: a feasibility study. EuroIntervention. 13(9):e1076–e1079. https://doi.org/10.4244/EIJ-D-16-00921
Goitein O, Fink N, Hay I, Di Segni E, Guetta V, Goitein D, Brodov Y, Konen E, Glikson M (2017) Cardiac CT Angiography (CCTA) predicts left atrial appendage occluder device size and procedure outcome. Int J Cardiovasc Imaging 33:739–747. https://doi.org/10.1007/s10554-016-1050-6
Vukicevic M, Mosadegh B, Min JK, Little SH (2017) Cardiac 3D Printing and its Future Directions. JACC Cardiovasc Imaging 10:171–184. https://doi.org/10.1016/j.jcmg.2016.12.001
Olejník P, Nosal M, Havran T, Furdova A, Cizmar M, Slabej M, Thurzo A, Vitovic P, Klvac M, Acel T, Masura J (2017) Utilisation of three-dimensional printed heart models for operative planning of complex congenital heart defects. Kardiol Pol 75:495–501. https://doi.org/10.5603/KP.a2017.0033
Hadeed K, Acar P, Dulac Y, Cuttone F, Alacoque X, Karsenty C (2018) Cardiac 3D printing for better understanding of congenital heart disease. Arch Cardiovasc Dis 111(1):1–4. https://doi.org/10.1016/j.acvd.2017.10.001
Iriart X, Ciobotaru V, Martin C, Cochet H, Jalal Z, Thambo JB, Quessard A (2018) Role of cardiac imaging and three-dimensional printing in percutaneous appendage closure. Arch Cardiovasc Dis 111(6–7):411–420. https://doi.org/10.1016/j.acvd.2018.04.005
Ciobotaru V, Combes N, Martin CA, Marijon E, Maupas E, Bortone A, Bruguière E, Thambo JB, Teiger E, Pujadas-Berthault P, Ternacle J, Iriart X (2018) Left atrial appendage occlusion simulation based on three-dimensional printing: new insights into outcome and technique. EuroIntervention 14(2):176–184. https://doi.org/10.4244/EIJ-D-17-00970
Obasare E, Mainigi SK, Morris DL, Slipczuk L, Goykhman I, Friend E, Ziccardi MR, Pressman GS (2018) CT based 3D printing is superior to transesophageal echocardiography for pre-procedure planning in left atrial appendage device closure. Int J Cardiovasc Imaging 34(5):821–831. https://doi.org/10.1007/s10554-017-1289-6
Hell MM, Achenbach S, Yoo IS, Franke J, Blachutzik F, Roether J, Graf V, Raaz-Schrauder D, Marwan M, Schlundt C (2017) D printing for sizing left atrial appendage closure device: head-to-head comparison with computed tomography and transesophageal echocardiography. EuroIntervention. https://doi.org/10.4244/EIJ-D-17.
Wang DD, Eng M, Kupsky D, Myers E, Forbes M, Rahman M, Zaidan M, Parikh S, Wyman J, Pantelic M, Song T, Nadig J, Karabon P, Greenbaum A, O'Neill W (2016) Application of 3-dimensional computed tomographic image guidance to WATCHMAN implantation and impact on early operator learning curve: single-center experience. JACC Cardiovasc Interv 9:4129–4140. https://doi.org/10.1016/j.jcin.2016.07.038
Liu P, Liu R, Zhang Y, Liu Y, Tang X, Cheng Y (2016) The value of 3D printing models of left atrial appendage using real-Time 3D transesophageal echocardiographic data in left atrial appendage occlusion: applications toward an era of truly personalized medicine. Cardiology 135(4):255–261. https://doi.org/10.1159/000447444
Li H, Qingyao Bingshen, Shu M, Lizhong Wang X, Song Z (2017) Application of 3D printing technology to left atrial appendage occlusion. Int J Cardiol 15(411):258–263. https://doi.org/10.1016/j.ijcard.2017.01.031
Saw J, Percutaneous Lempereur M (2014) Left atrial appendage closure: procedural techniques and outcomes. JACC Cardiovasc Interv 7:1205–1220. https://doi.org/10.1016/j.jcin.2014.05.026
Cruz-González I, Freixa X, Fernández-Díaz JA, Moreno-Samos JC, Martín-Yuste V, Goicolea J (2018) Left Atrial Appendage Occlusion With the LAmbre Device: Initial Experience. Rev Esp Cardiol (Engl Ed) 71(9):755–756. https://doi.org/10.1016/j.rec.2017.04.015
De Backer O, Arnous S, Ihlemann N, Vejlstrup N, Jørgensen E, Pehrson S, Krieger TD, Meier P, Søndergaard L, Franzen OW (2014) Percutaneous left atrial appendage occlusion for stroke prevention in atrial fibrillation: an update. Open Heart 1:e000020. https://doi.org/10.1136/openhrt-2013-000020
Wunderlich NC, Beigel R, Swaans MJ, Ho SY, Siegel RJ (2015) Percutaneous interventions for left atrial appendage exclusion: options, assessment, and imaging using 2D and 3D echocardiography. JACC Cardiovasc Imaging 8:472–488. https://doi.org/10.1016/j.jcmg.2015.02.002
Piccini JP, Sievert H, Patel MR (2017) Left atrial appendage occlusion: rationale, evidence, devices, and patient selection. Eur Heart J 38(12):869–876. https://doi.org/10.1093/eurheartj/ehw330
Yu CM, Khattab AA, Bertog SC, Lee AP, Kwong JS, Sievert H, Meier B (2013) Mechanical antithrombotic intervention by LAA occlusion in atrial fibrillation. Nat Rev Cardiol 10:707–722. https://doi.org/10.1038/nrcardio.2013.158
Goitein O, Fink N, Guetta V, Beinart R, Brodov Y, Konen E, Goitein D, Di Segni E, Grupper A, Glikson M (2017) Printed MDCT 3D models for prediction of left atrial appendage (LAA) occluder device size: a feasibility study. EuroIntervention 13:e1076–e1079. https://doi.org/10.4244/EIJ-D-16-00921
Funding
This study was supported by a grant from the National Natural Science Fundation of China (Grant No. 81771849).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflict of interest to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Institutional Review Board of the Einstein Healthcare Network and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Jia, D., Zhou, Q., Song, Hn. et al. The value of the left atrial appendage orifice perimeter of 3D model based on 3D TEE data in the choice of device size of LAmbre™ occluder. Int J Cardiovasc Imaging 35, 1841–1851 (2019). https://doi.org/10.1007/s10554-019-01627-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-019-01627-4