Abstract
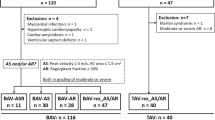
To compare reverse left ventricular (LV) remodeling after transcatheter aortic valve replacement (TAVR) between patients with bicuspid aortic valve (BAV) and tricuspid aortic valve (TAV). We retrospectively reviewed data of patients with at least two serial echocardiographic follow-ups (1, 3, 6 months and 1 year) post-TAVR. A total of 116 patients were identified. BAV morphology was documented in 67 patients. LV mass index (LVMi) at baseline was not significantly different between the TAV and BAV group (178.0 ± 6.9 vs. 166.3 ± 6.4 g/m2, P = 0.14). Reverse LV remodeling was observed in both BAV and TAV patients, but the reduction of LVMi from baseline was significantly more pronounced in TAV patients compared with BAV patients from 6 months post-TAVR (− 56.3 ± 8.1 vs. − 30.0 ± 4.7 g/m2, P < 0.01 at 6-month follow-up; − 60.6 ± 7.6 vs. − 37.9 ± 6.2 g/m2, P = 0.02 at 1-year follow-up). EDV value changes during follow-up were similar between patient with TAV and BAV. There were no significant differences in the proportions of patients with more than mild PVL or new permanent pacemaker between TAV and BAV morphology throughout the follow-up. Patients with bicuspid morphology might experience less pronounced reverse LV remodeling post-TAVR than patients with tricuspid morphology.



Similar content being viewed by others
References
Levy D, Garrison RJ, Savage DD et al (1990) Prognostic implications of echocardiographically determined left ventricular mass in the Framingham Heart Study. N Engl J Med 322:1561–1566. https://doi.org/10.1056/NEJM199005313222203
Une D, Mesana L, Chan V et al (2015) Clinical impact of changes in left ventricular function after aortic valve replacement: analysis from 3112 Patients. Circulation 132:741–747. https://doi.org/10.1161/CIRCULATIONAHA.115.015371
Lindman BR, Stewart WJ, Pibarot P et al (2014) Early regression of severe left ventricular hypertrophy after transcatheter aortic valve replacement is associated with decreased hospitalizations. JACC Cardiovasc Interv 7:662–673. https://doi.org/10.1016/j.jcin.2014.02.011
Ngo A, Hassager C, Thyregod HGH et al (2018) Differences in left ventricular remodelling in patients with aortic stenosis treated with transcatheter aortic valve replacement with corevalve prostheses compared to surgery with porcine or bovine biological prostheses. Eur Heart J Cardiovasc Imaging 19:39–46. https://doi.org/10.1093/ehjci/jew321
Roberts WC, Ko JM (2005) Frequency by decades of unicuspid, bicuspid, and tricuspid aortic valves in adults having isolated aortic valve replacement for aortic stenosis, with or without associated aortic regurgitation. Circulation 111:920–925. https://doi.org/10.1161/01.CIR.0000155623.48408.C5
Yoon S-H, Lefevre T, Ahn J-M et al (2016) Transcatheter aortic valve replacement with early- and new-generation devices in bicuspid aortic valve stenosis. J Am Coll Cardiol 68:1195–1205. https://doi.org/10.1016/j.jacc.2016.06.041
Grube E, Laborde JC, Gerckens U et al (2006) Percutaneous implantation of the corevalve self-expanding valve prosthesis in high-risk patients with aortic valve disease: the Siegburg first-in-man study. Circulation 114:1616–1624. https://doi.org/10.1161/CIRCULATIONAHA.106.639450
Petronio AS, De Carlo M, Bedogni F et al (2010) Safety and efficacy of the subclavian approach for transcatheter aortic valve implantation with the corevalve revalving system. Circ Cardiovasc Interv 3:359–366. https://doi.org/10.1161/CIRCINTERVENTIONS.109.930453
Kappetein AP, Head SJ, Genereux P et al (2012) Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document (VARC-2). Eur J Cardio-Thorac Surg Off J Eur Assoc Cardio-Thorac Surg 42:S45–S60. https://doi.org/10.1093/ejcts/ezs533
Lang RM, Badano LP, Mor-Avi V et al (2015) Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 28:1–39.e14. https://doi.org/10.1016/j.echo.2014.10.003
Magalhaes MA, Koifman E, Torguson R et al (2015) Outcome of left-sided cardiac remodeling in severe aortic stenosis patients undergoing transcatheter aortic valve implantation. Am J Cardiol 116:595–603. https://doi.org/10.1016/j.amjcard.2015.05.018
Kim S-J, Samad Z, Bloomfield GS, Douglas PS (2014) A critical review of hemodynamic changes and left ventricular remodeling after surgical aortic valve replacement and percutaneous aortic valve replacement. Am Heart J 168:150–159. https://doi.org/10.1016/j.ahj.2014.04.015.
Dweck MR, Joshi S, Murigu T et al (2012) Left ventricular remodeling and hypertrophy in patients with aortic stenosis: insights from cardiovascular magnetic resonance. J Cardiovasc Magn Reson Off J Soc Cardiovasc Magn Reson 14:50. https://doi.org/10.1186/1532-429X-14-50
Hahn RT, Roman MJ, Mogtader AH, Devereux RB (1992) Association of aortic dilation with regurgitant, stenotic and functionally normal bicuspid aortic valves. J Am Coll Cardiol 19:283–288
Lee SY, Shim CY, Hong G-R et al (2015) Association of aortic phenotypes and mechanical function with left ventricular diastolic function in subjects with normally functioning bicuspid aortic valves and comparison to subjects with tricuspid aortic valves. Am J Cardiol 116:1547–1554. https://doi.org/10.1016/j.amjcard.2015.08.017
Nistri S, Sorbo MD, Marin M et al (1999) Aortic root dilatation in young men with normally functioning bicuspid aortic valves. Heart Br Card Soc 82:19–22
von Knobelsdorff-Brenkenhoff F, Karunaharamoorthy A, Trauzeddel RF et al (2016) Evaluation of aortic blood flow and wall shear stress in aortic stenosis and its association with left ventricular remodeling. Circ Cardiovasc Imaging 9:e004038. https://doi.org/10.1161/CIRCIMAGING.115.004038
Kheradvar A, Pedrizzetti G (2012) Vortex formation in the cardiovascular system. Springer Science & Business Media, New York
Santarpia G, Scognamiglio G, Di Salvo G et al (2012) Aortic and left ventricular remodeling in patients with bicuspid aortic valve without significant valvular dysfunction: a prospective study. Int J Cardiol 158:347–352. https://doi.org/10.1016/j.ijcard.2011.01.046
Poulin F, Carasso S, Horlick EM et al (2014) Recovery of left ventricular mechanics after transcatheter aortic valve implantation: effects of baseline ventricular function and postprocedural aortic regurgitation. J Am Soc Echocardiogr Off Publ Am Soc Echocardiogr 27:1133–1142. https://doi.org/10.1016/j.echo.2014.07.001
Hoffmann R, Herpertz R, Lotfipour S et al (2012) Impact of a new conduction defect after transcatheter aortic valve implantation on left ventricular function. JACC Cardiovasc Interv 5:1257–1263. https://doi.org/10.1016/j.jcin.2012.08.011
Carrabba N, Valenti R, Migliorini A et al (2015) Impact on left ventricular function and remodeling and on 1-year outcome in patients with left bundle branch block after transcatheter aortic valve implantation. Am J Cardiol 116:125–131. https://doi.org/10.1016/j.amjcard.2015.03.054
Dobson LE, Musa TA, Uddin A et al (2017) The impact of trans-catheter aortic valve replacement induced left-bundle branch block on cardiac reverse remodeling. J Cardiovasc Magn Reson Off J Soc Cardiovasc Magn Reson 19:22. https://doi.org/10.1186/s12968-017-0335-9
Bjorck HM, Du L, Pulignani S et al (2018) Altered DNA methylation indicates an oscillatory flow mediated epithelial-to-mesenchymal transition signature in ascending aorta of patients with bicuspid aortic valve. Sci Rep 8:2777. https://doi.org/10.1038/s41598-018-20642-4
Naito S, Gross T, Disha K et al (2017) Late post-AVR progression of bicuspid aortopathy: link to hemodynamics. Gen Thorac Cardiovasc Surg 65:252–258. https://doi.org/10.1007/s11748-017-0746-4
Disha K, Dubslaff G, Rouman M et al (2017) Evidence of subannular and left ventricular morphological differences in patients with bicuspid versus tricuspid aortic valve stenosis: magnetic resonance imaging-based analysis. Interact Cardiovasc Thorac Surg 24:369–376. https://doi.org/10.1093/icvts/ivw363
Sato K, Kumar A, Jones BM et al (2017) Reversibility of cardiac function predicts outcome after transcatheter aortic valve replacement in patients with severe aortic stenosis. J Am Heart Assoc. https://doi.org/10.1161/JAHA.117.005798
Acknowledgements
This work was supported by National Natural Science Foundation of China (81370219, Beijing, China); Science and Technology Support Plan of Sichuan province (2016FZ0078); Science and Technology Innovative Research Groups Program of Sichuan province (2017TD0004); “13th Five-Year” National key Research and Development Program of China (2016YFC1102200); West China Hospital “1·3·5” Discipline of Excellence Project-Percutaneous transcatheter aortic valve implantation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Chen and Y. Feng are consultants/proctors of Venus MedTech and MicroPort. The other authors do not have disclosures.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Xiong, TY., Wang, X., Li, YJ. et al. Less pronounced reverse left ventricular remodeling in patients with bicuspid aortic stenosis treated with transcatheter aortic valve replacement compared to tricuspid aortic stenosis. Int J Cardiovasc Imaging 34, 1761–1767 (2018). https://doi.org/10.1007/s10554-018-1401-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-018-1401-6