Abstract
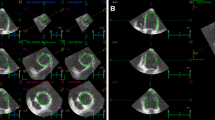
Left ventricular (LV) hypertrophy and one of its inducers, the fibroblast growth factor-23 (FGF-23) were found to be associated with unfavourable outcome in end-stage renal disease (ESRD) patients. We sought to investigate the influence of hemodialysis (HD), increased LV mass and FGF-23 on LV mechanics using three-dimensional (3D) speckle tracking echocardiography. Forty-four ESRD patients on maintenance HD were examined just before and immediately after HD, and were compared to 44 normal controls (NC). Transthoracic 3D recordings were obtained using multi-beat reconstruction from 6 consecutive cardiac cycles. LV mass index (LVMi) was evaluated and 3D speckle tracking analysis was performed to calculate global longitudinal (GLS), circumferential (GCS), area (GAS) and radial (GRS) peak systolic strain. Serum FGF-23 levels were also measured. Strain values improved in all directions after HD [pre- vs. post-HD; GLS: −20(3) vs. −21(6), GCS: −20(4) vs. −22(7), GAS: −33(5) vs. −35(10), GRS: 50(12) vs. 53.5(20) %, all p < 0.01]. LVMi was remarkably increased in our patients [ESRD vs. NC; 136(46) vs. 71(8) g/m2, p < 0.001]. Elevated FGF-23 levels were associated with increased LV mass (ρ = 0.581, p < 0.001). LVMi was inversely related to pre-HD GCS (ρ = 0.626, p < 0.001) and post-HD GCS (ρ = 0.761, p < 0.001), GAS (ρ = 0.534, p < 0.05) and GRS (ρ = −0.639, p < 0.01). Serum FGF-23 levels correlated with post-HD GAS (ρ = 0.513, p < 0.01) and GRS (ρ = −0.512, p < 0.05). HD treatment results in immediate improvement in all strain directions. Besides inducing LV hypertrophy, FGF-23 may play a role in the deterioration of LV mechanics in patients with ESRD.

Similar content being viewed by others
References
Shlipak MG, Fried LF, Cushman M, Manolio TA, Peterson D, Stehman-Breen C, Bleyer A, Newman A, Siscovick D, Psaty B (2005) Cardiovascular mortality risk in chronic kidney disease: comparison of traditional and novel risk factors. JAMA 293(14):1737–1745. doi:10.1001/jama.293.14.1737
Taddei S, Nami R, Bruno RM, Quatrini I, Nuti R (2011) Hypertension, left ventricular hypertrophy and chronic kidney disease. Heart Fail Rev 16(6):615–620. doi:10.1007/s10741-010-9197-z
Moody WE, Edwards NC, Chue CD, Ferro CJ, Townend JN (2013) Arterial disease in chronic kidney disease. Heart 99(6):365–372. doi:10.1136/heartjnl-2012-302818
Chue CD, Edwards NC, Moody WE, Steeds RP, Townend JN, Ferro CJ (2012) Serum phosphate is associated with left ventricular mass in patients with chronic kidney disease: a cardiac magnetic resonance study. Heart 98(3):219–224. doi:10.1136/heartjnl-2011-300570
Heine GH, Seiler S, Fliser D (2012) FGF-23: the rise of a novel cardiovascular risk marker in CKD. Nephrol Dial Transplant 27(8):3072–3081. doi:10.1093/ndt/gfs259
Faul C, Amaral AP, Oskouei B, Hu MC, Sloan A, Isakova T, Gutierrez OM, Aguillon-Prada R, Lincoln J, Hare JM, Mundel P, Morales A, Scialla J, Fischer M, Soliman EZ, Chen J, Go AS, Rosas SE, Nessel L, Townsend RR, Feldman HI, John Sutton M, Ojo A, Gadegbeku C, Di Marco GS, Reuter S, Kentrup D, Tiemann K, Brand M, Hill JA, Moe OW, Kuro OM, Kusek JW, Keane MG, Wolf M (2011) FGF23 induces left ventricular hypertrophy. J Clin Invest 121(11):4393–4408. doi:10.1172/JCI46122
Isakova T (2012) Fibroblast growth factor 23 and adverse clinical outcomes in chronic kidney disease. Curr Opin Nephrol Hypertens 21(3):334–340. doi:10.1097/MNH.0b013e328351a391
Bansal N, Keane M, Delafontaine P, Dries D, Foster E, Gadegbeku CA, Go AS, Hamm LL, Kusek JW, Ojo AO, Rahman M, Tao K, Wright JT, Xie D, Hsu CY, CRIC Study Investigators (2013) A longitudinal study of left ventricular function and structure from CKD to ESRD: the CRIC study. Clin J Am Soc Nephrol 8(3):355–362. doi:10.2215/CJN.06020612
Badano LP, Boccalini F, Muraru D, Bianco LD, Peluso D, Bellu R, Zoppellaro G, Iliceto S (2012) Current clinical applications of transthoracic three-dimensional echocardiography. J Cardiovasc Ultrasound 20(1):1–22. doi:10.4250/jcu.2012.20.1.1
Mosteller RD (1987) Simplified calculation of body-surface area. N Engl J Med 317(17):1098. doi:10.1056/NEJM198710223171717
Badano LP (2013) Defining normative values for 3D LV volumes: the devil is in the details. JACC Cardiovasc Imaging 6(4):530. doi:10.1016/j.jcmg.2013.01.008
Muraru D, Badano LP, Piccoli G, Gianfagna P, Del Mestre L, Ermacora D, Proclemer A (2010) Validation of a novel automated border-detection algorithm for rapid and accurate quantitation of left ventricular volumes based on three-dimensional echocardiography. Eur J Echocardiogr 11(4):359–368. doi:10.1093/ejechocard/jep217
Muraru D, Badano LP, Peluso D, Dal Bianco L, Casablanca S, Kocabay G, Zoppellaro G, Iliceto S (2013) Comprehensive analysis of left ventricular geometry and function by three-dimensional echocardiography in healthy adults. J Am Soc Echocardiogr 26(6):618–628. doi:10.1016/j.echo.2013.03.014
Alhaj E, Alhaj N, Rahman I, Niazi TO, Berkowitz R, Klapholz M (2013) Uremic cardiomyopathy: an underdiagnosed disease. Congest Heart Fail. doi:10.1111/chf.12030
Thorstensen A, Dalen H, Hala P, Kiss G, D’Hooge J, Torp H, Stoylen A, Amundsen B (2013) Three-dimensional echocardiography in the evaluation of global and regional function in patients with recent myocardial infarction: a comparison with magnetic resonance imaging. Echocardiography 30(6):682–692. doi:10.1111/echo.12115
Hayat D, Kloeckner M, Nahum J, Ecochard-Dugelay E, Dubois-Rande JL, Jean-Francois D, Gueret P, Lim P (2012) Comparison of real-time three-dimensional speckle tracking to magnetic resonance imaging in patients with coronary heart disease. Am J Cardiol 109(2):180–186. doi:10.1016/j.amjcard.2011.08.030
Kovacs A, Apor A, Nagy A, Vago H, Toth A, Nagy AI, Kovats T, Sax B, Szeplaki G, Becker D, Merkely B (2014) Left ventricular untwisting in athlete’s heart: key role in early diastolic filling? Int J Sports Med 35(3):259–264. doi:10.1055/s-0033-1349076
Bansal M, Sengupta PP (2013) Longitudinal and circumferential strain in patients with regional LV dysfunction. Curr Cardiol Rep 15(3):339. doi:10.1007/s11886-012-0339-x
Wang H, Liu J, Yao XD, Li J, Yang Y, Cao TS, Yang B (2012) Multidirectional myocardial systolic function in hemodialysis patients with preserved left ventricular ejection fraction and different left ventricular geometry. Nephrol Dial Transplant 27(12):4422–4429. doi:10.1093/ndt/gfs090
Yan P, Li H, Hao C, Shi H, Gu Y, Huang G, Chen J (2011) 2D-speckle tracking echocardiography contributes to early identification of impaired left ventricular myocardial function in patients with chronic kidney disease. Nephron Clin Pract 118(3):c232–c240. doi:10.1159/000321383
Gulel O, Soylu K, Yuksel S, Karaoglanoglu M, Cengiz K, Dilek M, Hamiseyev C, Kale A, Arik N (2008) Evidence of left ventricular systolic and diastolic dysfunction by color tissue Doppler imaging despite normal ejection fraction in patients on chronic hemodialysis program. Echocardiography 25(6):569–574
Liu YW, Su CT, Huang YY, Yang CS, Huang JW, Yang MT, Chen JH, Tsai WC (2011) Left ventricular systolic strain in chronic kidney disease and hemodialysis patients. Am J Nephrol 33(1):84–90. doi:10.1159/000322709
Chan C, Floras JS, Miller JA, Pierratos A (2002) Improvement in ejection fraction by nocturnal haemodialysis in end-stage renal failure patients with coexisting heart failure. Nephrol Dial Transplant 17(8):1518–1521
Siedlecki A, Foushee M, Curtis JJ, Gaston RS, Perry G, Iskandrian AE, de Mattos AM (2007) The impact of left ventricular systolic dysfunction on survival after renal transplantation. Transplantation 84(12):1610–1617. doi:10.1097/01.tp.0000295748.42884.97
de Mattos AM, Siedlecki A, Gaston RS, Perry GJ, Julian BA, Kew CE II, Deierhoi MH, Young C, Curtis JJ, Iskandrian AE (2008) Systolic dysfunction portends increased mortality among those waiting for renal transplant. J Am Soc Nephrol 19(6):1191–1196. doi:10.1681/ASN.2007040503
Altekin RE, Kucuk M, Yanikoglu A, Karakas MS, Er A, Ozel D, Ermis C, Demir I (2012) Evaluation of the left ventricular regional function using two-dimensional speckle tracking echocardiography in patients with end-stage renal disease with preserved left ventricular ejection fraction. Acta Cardiol 67(6):681–691
Galderisi M, Esposito R, Schiano-Lomoriello V, Santoro A, Ippolito R, Schiattarella P, Strazzullo P, de Simone G (2012) Correlates of global area strain in native hypertensive patients: a three-dimensional speckle-tracking echocardiography study. Eur Heart J Cardiovasc Imaging 13(9):730–738. doi:10.1093/ehjci/jes026
Wald R, Goldstein MB, Wald RM, Harel Z, Kirpalani A, Perl J, Yuen DA, Wolf MS, Yan AT (2014) Correlates of left ventricular mass in chronic hemodialysis recipients. Int J Cardiovasc Imaging 30(2):349–356. doi:10.1007/s10554-013-0337-0
Smith K, deFilippi C, Isakova T, Gutierrez OM, Laliberte K, Seliger S, Kelley W, Duh SH, Hise M, Christenson R, Wolf M, Januzzi J (2013) Fibroblast growth factor 23, high-sensitivity cardiac troponin, and left ventricular hypertrophy in CKD. Am J Kidney Dis 61(1):67–73. doi:10.1053/j.ajkd.2012.06.022
Touchberry CD, Green TM, Tchikrizov V, Mannix JE, Mao TF, Carney BW, Girgis M, Vincent RJ, Wetmore LA, Dawn B, Bonewald LF, Stubbs JR, Wacker MJ (2013) FGF23 is a novel regulator of intracellular calcium and cardiac contractility in addition to cardiac hypertrophy. Am J Physiol Endocrinol Metab 304(8):E863–E873. doi:10.1152/ajpendo.00596.2012
Sharma S, Joseph J, Chonchol M, Kaufman JS, Cheung AK, Rafeq Z, Smits G, Kendrick J (2013) Higher fibroblast growth factor-23 concentrations associate with left ventricular systolic dysfunction in dialysis patients. Clin Nephrol. doi:10.5414/CN107991
Ernande L, Bergerot C, Rietzschel ER, De Buyzere ML, Thibault H, Pignonblanc PG, Croisille P, Ovize M, Groisne L, Moulin P, Gillebert TC, Derumeaux G (2011) Diastolic dysfunction in patients with type 2 diabetes mellitus: is it really the first marker of diabetic cardiomyopathy? J Am Soc Echocardiogr 24(11):1268–1275. doi:10.1016/j.echo.2011.07.017
Assa S, Hummel YM, Voors AA, Kuipers J, Westerhuis R, de Jong PE, Franssen CF (2012) Hemodialysis-induced regional left ventricular systolic dysfunction: prevalence, patient and dialysis treatment-related factors, and prognostic significance. Clin J Am Soc Nephrol 7(10):1615–1623. doi:10.2215/CJN.00850112
Dou Y, Zhu F, Kotanko P (2012) Assessment of extracellular fluid volume and fluid status in hemodialysis patients: current status and technical advances. Semin Dial 25(4):377–387. doi:10.1111/j.1525-139X.2012.01095.x
Acknowledgments
Authors are grateful to GE Healthcare for equipment support and to Fresenius Medical Care for allowing our study. This work was supported by the Hungarian Scientific Research Fund (Grant Number 105555).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kovács, A., Tapolyai, M., Celeng, C. et al. Impact of hemodialysis, left ventricular mass and FGF-23 on myocardial mechanics in end-stage renal disease: a three-dimensional speckle tracking study. Int J Cardiovasc Imaging 30, 1331–1337 (2014). https://doi.org/10.1007/s10554-014-0480-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10554-014-0480-2