Abstract
Background
Gastric cancer is a major cause of morbidity and mortality in Japan and worldwide. Emerging literature has suggested unfavorable health outcomes associated with daytime napping. Herein, we aimed to investigate the association between daytime napping and the risk of gastric cancer among Japanese people.
Methods
This prospective cohort study included 49,037 participants, aged 40–79 years, from the Japan Collaborative Cohort Study (JACC Study). Participants with positive cancer history and those who reported night or rotational shift work were excluded. Cox proportional hazard models were used to calculate hazard ratios (HRs) and 95% confidence intervals (CIs) of incident gastric cancer among daytime nappers.
Results
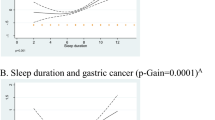
Within 650,040 person-years (median = 13.7 years) of follow-up, 1,164 participants developed gastric cancer. Daytime napping was associated with the increased risk of gastric cancer in the multivariable-adjusted model: HR (95% CI) = 1.14 (1.01, 1.29). The excess risk did not significantly differ across sexes, age groups (<65 and ≥65 years), and employment status (employed and unemployed) (p-interactions > 0.40). However, sleep duration modified this effect: HRs (95% CIs) = 1.66 (1.23, 2.23) in sleep duration ≤6 h/night versus 1.06 (0.93, 1.21) in sleep duration >6 h/night (p-interaction = 0.006).
Conclusion
Daytime napping was associated with increased gastric cancer risk, especially among those who reported short sleep duration.
Similar content being viewed by others
Data and materials availability
Not available for ethical reasons.
Abbreviations
- CI:
-
Confidence interval
- HR:
-
Hazard ratio
- JACC Study:
-
Japan Collaborative Cohort Study
- RR:
-
Relative risk
- OR:
-
Odds ratio
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A et al (2021) Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249
Cancer Statistics in Japan 2022. https://ganjoho.jp/public/qa_links/report/statistics/pdf/cancer_statistics_2022_fig_E.pdf. Accessed 8 Oct 2023
Rawla P, Barsouk A (2019) Epidemiology of gastric cancer: global trends, risk factors and prevention. Prz Gastroenterol 14(1):26–38
Liu X, Zhang Q, Shang X (2015) Meta-analysis of self-reported daytime napping and risk of cardiovascular or all-cause mortality. Med Sci Monit 21:1269–1275
Zhong G, Wang Y, Tao T, Ying J, Zhao Y (2015) Daytime napping and mortality from all causes, cardiovascular disease, and cancer: a meta-analysis of prospective cohort studies. Sleep Med 16(7):811–819
Cairns BJ, Travis RC, Wang XS, Reeves GK, Green J, Beral V, Million Women Study Collaborators (2012) A short-term increase in cancer risk associated with daytime napping is likely to reflect pre-clinical disease: prospective cohort study. Br J Cancer 107(3):527–30
Wang P, Ren FM, Lin Y, Su FX, Jia WH, Su XF et al (2015) Night-shift work, sleep duration, daytime napping, and breast cancer risk. Sleep Med 16(4):462–468
Arafa A, Eshak ES, Shirai K, Muraki I, Tamakoshi A, Iso H, JACC Study Group (2023) Daytime napping and risk of liver cancer: a large population-based prospective cohort study. Ann Hepatol 28(2):100877
Papantoniou K, Castaño-Vinyals G, Espinosa A, Turner MC, Martín-Sánchez V, Casabonne D et al (2021) Sleep duration and napping in relation to colorectal and gastric cancer in the MCC-Spain study. Sci Rep 11(1):11822
Dutheil F, Danini B, Bagheri R, Fantini ML, Pereira B, Moustafa F et al (2021) Effects of a short daytime nap on the cognitive performance: a systematic review and meta-analysis. Int J Environ Res Public Health 18(19):10212
Souabni M, Hammouda O, Romdhani M, Trabelsi K, Ammar A, Driss T (2021) Benefits of daytime napping opportunity on physical and cognitive performances in physically active participants: a systematic review. Sports Med 51(10):2115–2146
Zhao X, Cheng L, Zhu C, Cen S, Lin W, Zheng W et al (2021) A double-edged sword: the association of daytime napping duration and metabolism related diseases in a Chinese population. Eur J Clin Nutr 75(2):291–298
Bursztyn M, Stessman J (2005) The siesta and mortality: twelve years of prospective observations in 70-year-olds. Sleep 28(3):345–347
Potter GD, Skene DJ, Arendt J, Cade JE, Grant PJ, Hardie LJ (2016) Circadian rhythm and sleep disruption: causes, metabolic consequences, and countermeasures. Endocr Rev 37(6):584–608
Hu ML, Yeh KT, Lin PM, Hsu CM, Hsiao HH, Liu YC et al (2014) Deregulated expression of circadian clock genes in gastric cancer. BMC Gastroenterol 14:67
Li T, Shao W, Li S, Ma L, Zheng L, Shang W, Jia X, Sun P, Liang X, Jia J (2019) H. pylori infection induced BMAL1 expression and rhythm disorder aggravate gastric inflammation. EBioMedicine 39:301–314
Jaroenlapnopparat A, Bhatia K, Coban S (2022) Inflammation and gastric cancer. Diseases 10(3):35
Liu X, Chen S, Liu J, Xu D, Li W, Zhan Y, Sun X (2017) Impact of systemic inflammation on gastric cancer outcomes. PLoS ONE 12(3):e0174085
Fink AM, Bronas UG, Calik MW (2018) Autonomic regulation during sleep and wakefulness: a review with implications for defining the pathophysiology of neurological disorders. Clin Auton Res 28(6):509–518
Gao J, Liu SG (2021) Role of sympathetic and parasympathetic nerves in the development of gastric cancer through antagonism. Chin Med J (Engl) 134(8):908–909
Codoñer-Franch P, Gombert M (2018) Circadian rhythms in the pathogenesis of gastrointestinal diseases. World J Gastroenterol 24(38):4297–4303
Wan Q, Zhao R, Xia L, Wu Y, Zhou Y, Wang Y et al (2021) Inflammatory bowel disease and risk of gastric, small bowel and colorectal cancer: a meta-analysis of 26 observational studies. J Cancer Res Clin Oncol 147(4):1077–1087
Tse LA, Wang C, Rangarajan S, Liu Z, Teo K, Yusufali A et al (2021) Timing and length of nocturnal sleep and daytime napping and associations with obesity types in high-, middle-, and low-income countries. JAMA Netw Open 4(6):e2113775
Wang H, Chen L, Shen D, Cao Y, Zhang X, Xie K et al (2021) Association of daytime napping in relation to risk of diabetes: evidence from a prospective study in Zhejiang, China. Nutr Metab (Lond) 18(1):18
Yoo H, Kim H, Lee JH, Lee KS, Choi MJ, Song HR et al (2019) Study on the relevance of metabolic syndrome and incidence of gastric cancer in Korea. Int J Environ Res Public Health 16(7):1101
Monk TH, Buysse DJ, Welsh DK, Kennedy KS, Rose LR (2001) A sleep diary and questionnaire study of naturally short sleepers. J Sleep Res 10(3):173–179
Acknowledgments
None to declare.
Funding
This work was supported by Grants-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan (MEXT) (Monbusho); Grants-in-Aid for Scientific Research on Priority Areas of Cancer; and Grants-in-Aid for Scientific Research on Priority Areas of Cancer Epidemiology from MEXT (MonbuKagaku-sho) (Nos. 61010076, 62010074, 63010074, 1010068, 2151065, 3151064, 4151063, 5151069, 6279102, 11181101, 17015022, 18014011, 20014026, 20390156, and 26293138), Comprehensive Research on Cardiovascular and Life-Style Related Diseases (H26-Junkankitou [Seisaku]-Ippan-001and H29-Junkankitou [Seishuu]-Ippan-003), JSPS KAKENHI Grant Number JP 16H06277, and Grants-in-Aid for China Scholarship Council (CSC file No. 201608050-113).
Author information
Authors and Affiliations
Consortia
Contributions
FY and AA (conceptualization, review literature, draft writing, and data analysis), ESE, KS, and HI (supervision), ESE, KS, IM, HI, and AT (visualization, critical revision, and editing), and HI and AT (resources and funding acquisition).
Corresponding authors
Ethics declarations
Conflict of interest
None to declare.
Ethical approval and consent to participate
The research ethics committees of Nagoya University School of Medicine and Osaka University approved the protocol of the JACC study. Written informed consent was obtained from participants and community leaders.
Consent for publication
We obtained consent from participants and community leaders to publish the findings while keeping their details anonymous and all authors accepted the final version of the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yan, F., Arafa, A., Eshak, E.S. et al. Daytime napping and the risk of gastric cancer: the JACC Study. Cancer Causes Control (2024). https://doi.org/10.1007/s10552-024-01858-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10552-024-01858-4