Abstract
Purpose
Mounting evidence suggests a possible link between gut microbiome and oral cancer, pointing to some potential modifiable targets for disease prevention. In the present study, Mendelian randomization (MR) was used to explore whether there was a causal link between gut microbiome and oral cancer.
Methods
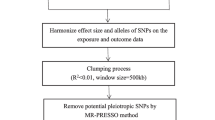
The single nucleotide polymorphisms (SNPs) significantly associated with gut microbiome were served as instrumental variables. MR analyses were performed using genetic approaches such as inverse variance weighting (IVW), MR Egger and weighted median, with IVW as the primary approach, supplemented by MR Egger and weighted median. Mendelian randomization pleiotropy residual sum and outlier (MR-PRESSO) and MR-Egger regression were used to detect the presence of horizontal pleiotropy and identify outlier SNPs.
Results
Causal effect estimates indicated that genetically predicted abundance of Prevotellaceae was associated with higher risk of oral cancer (odds ratio (OR) 1.80, 95% confidence interval (CI) 1.16–2.81, p = 0.009). There was no evidence of notable heterogeneity and horizontal pleiotropy.
Conclusion
Genetically derived estimates suggest that Prevotellaceae may be associated with the risk of oral cancer. Such robust evidence should be given priority in future studies and explore the underlying mechanisms.


Similar content being viewed by others
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on request.
References
Kaur J, Srivastava R, Borse V (2021) Recent advances in point-of-care diagnostics for oral cancer. Biosens Bioelectron 178:112995. https://doi.org/10.1016/j.bios.2021.112995
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Giraldi L, Leoncini E, Pastorino R et al (2017) Alcohol and cigarette consumption predict mortality in patients with head and neck cancer: a pooled analysis within the International Head and Neck Cancer Epidemiology (INHANCE) Consortium. Ann Oncol 28(11):2843–2851. https://doi.org/10.1093/annonc/mdx486
McCullough MJ, Prasad G, Farah CS (2010) Oral mucosal malignancy and potentially malignant lesions: an update on the epidemiology, risk factors, diagnosis and management. Aust Dent J 55(Suppl 1):61–65. https://doi.org/10.1111/j.1834-7819.2010.01200.x
Madera Anaya MV, Franco JV, Merchán-Galvis ÁM et al (2018) Quality assessment of clinical practice guidelines on treatments for oral cancer. Cancer Treat Rev 65:47–53. https://doi.org/10.1016/j.ctrv.2018.03.001
Lau A, Li KY, Yang WF et al (2016) Induction chemotherapy for squamous cell carcinomas of the oral cavity: a cumulative meta-analysis. Oral Oncol 61:104–114. https://doi.org/10.1016/j.oraloncology.2016.08.022
Korpela K, Helve O, Kolho KL et al (2020) Maternal fecal microbiota transplantation in cesarean-born infants rapidly restores normal gut microbial development: a proof-of-concept study. Cell 183(2):324–334. https://doi.org/10.1016/j.cell.2020.08.047
de Vos WM, Tilg H, Van Hul M et al (2022) Gut microbiome and health: mechanistic insights. Gut 71(5):1020–1032. https://doi.org/10.1136/gutjnl-2021-326789
Gopalakrishnan V, Helmink BA, Spencer CN et al (2018) The influence of the gut microbiome on cancer, immunity, and cancer immunotherapy. Cancer Cell 33(4):570–580. https://doi.org/10.1016/j.ccell.2018.03.015
Chen F, Dai X, Zhou CC et al (2022) Integrated analysis of the faecal metagenome and serum metabolome reveals the role of gut microbiome-associated metabolites in the detection of colorectal cancer and adenoma. Gut 71(7):1315–1325. https://doi.org/10.1136/gutjnl-2020-323476
Yang Y, Misra BB, Liang L et al (2019) Integrated microbiome and metabolome analysis reveals a novel interplay between commensal bacteria and metabolites in colorectal cancer. Theranostics 9(14):4101–4114. https://doi.org/10.7150/thno.35186
Temraz S, Nassar F, Nasr R et al (2019) Gut microbiome: a promising biomarker for immunotherapy in colorectal cancer. Int J Mol Sci 20(17):4155. https://doi.org/10.3390/ijms20174155
Heshiki Y, Vazquez-Uribe R, Li J et al (2020) Predictable modulation of cancer treatment outcomes by the gut microbiota. Microbiome 8(1):28. https://doi.org/10.1186/s40168-020-00811-2
Choi KW, Chen CY, Stein MB et al (2019) Assessment of bidirectional relationships between physical activity and depression among adults: a 2-sample Mendelian randomization study. JAMA Psychiat 76(4):399–408. https://doi.org/10.1001/jamapsychiatry.2018.4175
Kurilshikov A, Medina-Gomez C, Bacigalupe R et al (2021) Large-scale association analyses identify host factors influencing human gut microbiome composition. Nat Genet 53(2):156–165. https://doi.org/10.1038/s41588-020-00763-1
Lesseur C, Diergaarde B, Olshan AF et al (2016) Genome-wide association analyses identify new susceptibility loci for oral cavity and pharyngeal cancer. Nat Genet 48(12):1544–1550. https://doi.org/10.1038/ng.3685
Zheng J, Baird D, Borges MC et al (2017) Recent developments in mendelian randomization studies. Curr Epidemiol Rep 4(4):330–345. https://doi.org/10.1007/s40471-017-0128-6
Burgess S, Scott RA, Timpson NJ et al (2015) Using published data in Mendelian randomization: a blueprint for efficient identification of causal risk factors. Eur J Epidemiol 30(7):543–552. https://doi.org/10.1007/s10654-015-0011-z
Bowden J, Davey Smith G, Burgess S (2015) Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol 44(2):512–525. https://doi.org/10.1093/ije/dyv080
Bowden J, Davey Smith G, Haycock PC et al (2016) Consistent estimation in mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol 40(4):304–314. https://doi.org/10.1002/gepi.21965
D’souza S, Addepalli V (2018) Preventive measures in oral cancer: an overview. Biomed Pharmacother 107:72–80. https://doi.org/10.1016/j.biopha.2018.07.114
Matson V, Chervin CS, Gajewski TF (2021) Cancer and the microbiome-influence of the commensal microbiota on cancer, immune responses, and immunotherapy. Gastroenterology 160(2):600–163. https://doi.org/10.1053/j.gastro.2020.11.041
Loftus M, Hassouneh SA, Yooseph S (2021) Bacterial community structure alterations within the colorectal cancer gut microbiome. BMC Microbiol 21(1):98. https://doi.org/10.1186/s12866-021-02153-x
Liao H, Li C, Ai Y et al (2021) Gut microbiome is more stable in males than in females during the development of colorectal cancer. J Appl Microbiol 131(1):435–448. https://doi.org/10.1111/jam.14943
Kadosh E, Snir-Alkalay I, Venkatachalam A et al (2020) The gut microbiome switches mutant p53 from tumour-suppressive to oncogenic. Nature 586(7827):133–138. https://doi.org/10.1038/s41586-020-2541-0
Zhang Y, Shen J, Shi X et al (2021) Gut microbiome analysis as a predictive marker for the gastric cancer patients. Appl Microbiol Biotechnol 105(2):803–814. https://doi.org/10.1007/s00253-020-11043-7
Sethi V, Kurtom S, Tarique M et al (2018) Gut microbiota promotes tumor growth in mice by modulating immune response. Gastroenterology 155(1):33-37.e6. https://doi.org/10.1053/j.gastro.2018.04.001
Tikka C, Manthari RK, Ommati MM et al (2020) Immune disruption occurs through altered gut microbiome and NOD2 in arsenic induced mice: correlation with colon cancer markers. Chemosphere 246:125791. https://doi.org/10.1016/j.chemosphere.2019.125791
Baruch EN, Youngster I, Ben-Betzalel G et al (2021) Fecal microbiota transplant promotes response in immunotherapy-refractory melanoma patients. Science 371(6529):602–609. https://doi.org/10.1126/science.abb5920
Zhao Y, Feng Y, Ye Q et al (2022) The oral microbiome in young women at different stages of periodontitis: Prevotella dominant in stage III periodontitis. Front Cell Infect Microbiol 12:1047607. https://doi.org/10.3389/fcimb.2022.1047607
Zhang L, Liu Y, Zheng HJ et al (2020) The oral microbiota may have influence on oral cancer. Front Cell Infect Microbiol 9:476. https://doi.org/10.3389/fcimb.2019.00476
Li Z, Chen G, Wang P et al (2021) Alterations of the oral microbiota profiles in Chinese patient with oral cancer. Front Cell Infect Microbiol 11:780067. https://doi.org/10.3389/fcimb.2021.780067
Zhang Y, D’Souza G, Fakhry C et al (2022) Oral human papillomavirus associated with differences in oral microbiota beta diversity and microbiota abundance. J Infect Dis 226(6):1098–1108. https://doi.org/10.1093/infdis/jiac010
Zhang X, Li C, Cao W et al (2021) Alterations of gastric microbiota in gastric cancer and precancerous stages. Front Cell Infect Microbiol 11:559148. https://doi.org/10.3389/fcimb.2021.559148
Zhao Q, Yang T, Yan Y et al (2020) Alterations of oral microbiota in Chinese patients with esophageal cancer. Front Cell Infect Microbiol 10:541144. https://doi.org/10.3389/fcimb.2020.541144
Chen W, Liu F, Ling Z et al (2012) Human intestinal lumen and mucosa-associated microbiota in patients with colorectal cancer. PLoS ONE 7(6):e39743. https://doi.org/10.1371/journal.pone.0039743
Zackular JP, Baxter NT, Iverson KD et al (2013) The gut microbiome modulates colon tumorigenesis. mBio 4(6):e00692-13. https://doi.org/10.1128/mBio.00692-13
Bascones-Martínez A, Figuero-Ruiz E (2004) Periodontal diseases as bacterial infection. Med Oral Patol Oral Cir Bucal 9(Suppl):101–100. https://doi.org/10.4321/s1699-65852005000300002
Alnuaimi AD, Ramdzan AN, Wiesenfeld D et al (2016) Candida virulence and ethanol-derived acetaldehyde production in oral cancer and non-cancer subjects. Oral Dis 22(8):805–814. https://doi.org/10.1111/odi.12565
Karpiński TM (2019) Role of oral microbiota in cancer development. Microorganisms 7(1):20. https://doi.org/10.3390/microorganisms7010020
Díaz P, Valenzuela Valderrama M, Bravo J et al (2018) Helicobacter pylori and gastric cancer: adaptive cellular mechanisms involved in disease progression. Front Microbiol 9:5. https://doi.org/10.3389/fmicb.2018.00005
Gur C, Ibrahim Y, Isaacson B et al (2015) Binding of the Fap2 protein of Fusobacterium nucleatum to human inhibitory receptor TIGIT protects tumors from immune cell attack. Immunity 42(2):344–355. https://doi.org/10.1016/j.immuni.2015.01.010
Flanagan L, Schmid J, Ebert M et al (2014) Fusobacterium nucleatum associates with stages of colorectal neoplasia development, colorectal cancer and disease outcome. Eur J Clin Microbiol Infect Dis 33(8):1381–1390. https://doi.org/10.1007/s10096-014-2081-3
Huang J, Liu D, Wang Y et al (2022) Ginseng polysaccharides alter the gut microbiota and kynurenine/tryptophan ratio, potentiating the antitumour effect of antiprogrammed cell death 1/programmed cell death ligand 1 (anti-PD-1/PD-L1) immunotherapy. Gut 71(4):734–745. https://doi.org/10.1136/gutjnl-2020-321031
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. The first draft of the manuscript was written by KX. Analyses were performed by KX and CXL. RC and CHZ assisted in substantive revisions to the drafted manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
The article does not contain any studies with human participants or animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10552_2023_1800_MOESM1_ESM.tif
Supplementary file1 Fig. S1 Sensitivity analyses of the associations between Prevotellaceae and oral cancer (TIF 1621 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Xiang, K., Li, CX., Chen, R. et al. Genetically predicted gut microbiome and risk of oral cancer. Cancer Causes Control 35, 429–435 (2024). https://doi.org/10.1007/s10552-023-01800-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-023-01800-0