Abstract
Purpose
The U.S. military health system (MHS) provides beneficiaries with universal health care while health care access varies in the U.S. general population by insurance status/type. We divided the patients from the U.S. general population by insurance status/type and compared them to the MHS patients in survival.
Methods
The MHS patients were identified from the Department of Defense’s Automated Central Tumor Registry (ACTUR). Patients from the U.S. general population were identified from the Surveillance, Epidemiology, and End Results (SEER) program. Multivariable Cox regression analysis was conducted to compare different insurance status/type in SEER to ACTUR in overall survival.
Results
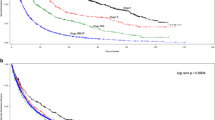
Compared to ACTUR patients with non-small cell lung cancer (NSCLC), SEER patients showed significant worse survival. The adjusted hazard ratios (HRs) were 1.08 [95% Confidence Interval (CI) = 1.03–1.13], 1.22 (95% CI = 1.16–1.28), 1.40 (95% CI = 1.33–1.47), 1.50 (95% CI = 1.41–1.59), for insured, insured/no specifics, Medicaid, and uninsured patients, respectively. The pattern was consistently observed in subgroup analysis by race, gender, age, or tumor stage. Results were similar for small cell lung cancer (SCLC), although they were only borderline significant in some subgroups.
Conclusion
The survival advantage of patients receiving care from a universal health care system over the patients from the general population was not restricted to uninsured or Medicaid as expected, but was present cross all insurance types, including patients with private insurance. Our findings highlight the survival benefits of universal health care system to lung cancer patients.


Similar content being viewed by others
Data availability
ACTUR data are not available for public use according to DoD regulations.
References
Niu X, Roche LM, Pawlish KS, Henry KA (2013) Cancer survival disparities by health insurance status. Cancer Med 2:403–411
Walker GV, Grant SR, Guadagnolo BA et al (2014) Disparities in stage at diagnosis, treatment, and survival in nonelderly adult patients with cancer according to insurance status. J Clin Oncol 32:3118–3125
Bradley CJ, Dahman B, Given CW (2008) Treatment and survival differences in older Medicare patients with lung cancer as compared with those who are dually eligible for Medicare and Medicaid. J Clin Oncol 26:5067–5073
Slatore CG, Au DH, Gould MK (2010) An official American Thoracic Society systematic review: insurance status and disparities in lung cancer practices and outcomes. Am J Respir Crit Care Med 182:1195–1205
Keating NL, Landrum MB, Lamont EB et al (2011) Quality of care for older patients with cancer in the Veterans Health Administration versus the private sector: a cohort study. Ann Intern Med 154:727–736
Pezzi TA, Schwartz DL, Mohamed ASR et al (2018) Barriers to combined-modality therapy for limited-stage small cell lung cancer. JAMA Oncol 4:e174504
Evaluation of the TRICARE Program: Fiscal Year 2020 Report to Congress: https://health.mil/Military-Health-Topics/Access-Cost-Quality-and-Safety/Health-Care-Program-Evaluation/Annual-Evaluation-of-the-TRICARE-Program. Accessed Apr 13 2021
TRICARE Health Plans. https://www.tricare.mil/Plans/HealthPlans. Accessed on Dec 20 2022
Evaluation of the TRICARE Program: Fiscal Year 2021 Report to Congress. https://www.health.mil/Military-Health-Topics/Access-Cost-Quality-and-Safety/Health-Care-Program-Evaluation/Annual-Evaluation-of-the-TRICARE-Program. Accessed Dec 21 2022
TRICARE Rates and Reimbursement. https://www.health.mil/Military-Health-Topics/Access-Cost-Quality-and-Safety/TRICARE-Health-Plan/Rates-and-Reimbursement. Accessed Dec 20 2022
Lin J, Kamamia C, Brown D et al (2018) Survival among lung cancer patients in the U.S. military health system: a comparison with the SEER population. Cancer Epidemiol Biomarkers Prev 27:673–679
Lin J, Kamamia C, Brown DW et al (2021) Comparative study of survival among small cell lung cancer patients in the U.S. military health system and those in the surveillance, epidemiology, and end results (SEER) program. Ann Epidemiol 64:132–139
Tryon J. (2007) User’s Guide For ACTUR Cancer Registry Software System Abstracting Module
SEER*Stat Databases: November 2014 Submission. Case Listing and Frequency Sessions: https://seer.cancer.gov/data-software/documentation/seerstat/nov2014/ Surveilance, Epidemiology, and End Results Program. Accessed Apr 13 2021
International Classification of Diseases for Oncology, 3rd Edition (ICD-O-3). World Health Organization. https://apps.who.int/iris/bitstream/handle/10665/96612/9789241548496_eng.pdf. Accessed Apr 13 2021
Flowchart Format—Multiple Primary and histology coding rules, lung multiple primary rules—Flowchart: https://seer.cancer.gov/tools/mphrules/mphrules_flowchart.pdf. Surveillance, Epidemiology and End Results Program, National Cancer Institute; Accessed Apr 12 2021
Altan M, Chiang AC (2015) Management of small cell lung cancer: progress and updates. Cancer J 21:425–433
National Comprehensive Cancer Network (NCCN) Clinical Practice Guidelines in Oncology. Small Cell Lung Cancer: https://www2.tri-kobe.org/nccn/guideline/lung/english/small.pdf. Accessed Apr 13 2021
SEER Program Coding and Staging Manual 2018. Surgery Codes. Lung C340-C349: https://seer.cancer.gov/manuals/2018/AppendixC/Surgery_Codes_Lung_2018.pdf. Accessed Mar 18 2020
SEER Ackowledgement of Treatment Data Limitations: https://seer.cancer.gov/data/sample-treatment-limitations.html. Surveillance, Epidemiology, and End Results Program, National Cancer Institute.
American Joint Committee on Cancer (2002) AJCC Cancer Staging Manual, sixth Edition. In: Greene FL, Page DL, Flemming ID et al (eds) Chicago. Springer, IL
Lee E, Wang JW (2003) Statistical Methods for Survival Data Analysis, 3rd edn. Wiley, Hoboken, New Jersey
Lin JQ, Li SQ, Pezzi TA et al (2020) Veterans affairs insurance disparities for metastatic lung cancer in the Hawaiian islands. JTO Clin Res Rep 1:100003
Parikh AA, Robinson J, Zaydfudim VM, Penson D, Whiteside MA (2014) The effect of health insurance status on the treatment and outcomes of patients with colorectal cancer. J Surg Oncol 110:227–232
Coburn N, Fulton J, Pearlman DN, Law C, DiPaolo B, Cady B (2008) Treatment variation by insurance status for breast cancer patients. Breast J 14:128–134
Virgo KS, Little AG, Fedewa SA, Chen AY, Flanders WD, Ward EM (2011) Safety-net burden hospitals and likelihood of curative-intent surgery for non-small cell lung cancer. J Am Coll Surg 213:633–643
Zafar SY, Peppercorn JM, Schrag D et al (2013) The financial toxicity of cancer treatment: a pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist 18:381–390
Ramsey SD, Bansal A, Fedorenko CR et al (2016) Financial insolvency as a risk factor for early mortality among patients with cancer. J Clin Oncol 34:980–986
Ning MS, Gomez DR, Shah AK et al (2019) The insurance approval process for proton radiation therapy: a significant barrier to patient care. Int J Radiat Oncol Biol Phys 104:724–733
Gupta A, Khan AJ, Goyal S et al (2019) Insurance approval for proton beam therapy and its impact on delays in treatment. Int J Radiat Oncol Biol Phys 104:714–723
Stokes SM, Wakeam E, Swords DS, Stringham JR, Varghese TK Jr (2018) Impact of insurance status on receipt of definitive surgical therapy and posttreatment outcomes in early stage lung cancer. Surgery 164:1287–1293
Groth SS, Al-Refaie WB, Zhong W et al (2013) Effect of insurance status on the surgical treatment of early-stage non-small cell lung cancer. Ann Thorac Surg 95:1221–1226
Acknowledgements
The authors thank Joint Pathology Center (formerly Armed Forces Institute of Pathology) for providing ACTUR data and the National Cancer Institute for the use of the SEER data.
Funding
This project was supported by Murtha Cancer Center Research Program via Uniformed Services University of the Health Sciences under the auspices of the Henry. M. Jackson Foundation for the Advancement of Military medicine.
Author information
Authors and Affiliations
Contributions
Conceptualization: JL, CDS, KZ, Methodology: JL, KZ, Formal analysis and investigation: JL, KZ, Writing—original draft: JL, Writing-review and editing: JL, CDS, KZ, Funding acquisition: CDS, Resources: CDS, KZ.
Corresponding author
Ethics declarations
Competing interests
The authors have no competing interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Disclaimers: The contents of this publication are the sole responsibility of the author(s) and do not necessarily reflect the views, opinions or policies of Uniformed Services University of the Health Sciences (USUHS), The Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc., the Department of Defense (DoD) or the Departments of the Army, Navy, or Air Force. Mention of trade names, commercial products, or organizations does not imply endorsement by the U.S. Government.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lin, J., Shriver, C.D. & Zhu, K. Survival among lung cancer patients: comparison of the U.S. military health system and the surveillance, epidemiology, and end results (SEER) program by health insurance status. Cancer Causes Control 35, 21–31 (2024). https://doi.org/10.1007/s10552-023-01765-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-023-01765-0