Abstract
Purpose
Racial disparities in acute myeloid leukemia (AML) have been reported but the relative contribution of disease versus patient-specific factors including comorbidities and access to care is unclear.
Methods
We conducted a retrospective analysis of patient characteristics, treatment patterns and outcomes in a racially diverse patient cohort controlling for cytogenetic risk group. Patients were classified into four groups: non-Hispanic White (NHW), non-Hispanic Black (NHB), Hispanic and Other.
Results
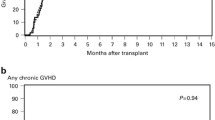
We evaluated 106 patients from 84 zipcodes incorporating demographics, clinicopathologic features, treatment patterns and outcomes. We identified significant differences in BMI and geographic poverty based on ethnoracial group, while prognostic mutations in NPM1 and FLT3 did not differ significantly. Utilization of intensive chemotherapy and transplant rate did not differ by ethnoracial group. However, there was a significantly higher use of alternate donor transplants in minority populations. There was a notably increased rate of clinical trial enrollment in NHW patients compared to other groups. In log-rank analysis, NHW patients had increased overall survival (OS) compared to NHB, Hispanic and Other patients (31.6 months vs. 16.7 months vs. 14.3 months, vs 18.1 months, p = 0.021). In bivariate analysis, overall survival was negatively influenced by advanced age and race. Obesity and zip code poverty levels approached statistical significance in predicting OS. In multivariate analysis, the only factors independently influencing OS were race and allogeneic stem cell transplant.
Conclusion
These results suggest that race impacts survival in intermediate-risk AML, highlighting the need to dissect biologic and nonbiologic factors that contribute to this disparity.


Similar content being viewed by others
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
De Santis CE, Miller KD, Goding Sauer A, Jemal A, Siegel RL (2019) Cancer statistics for African American. CA 69(3):211–233
Bang S-M, Ahn JY, Park J et al (2008) Low frequency and variability of FLT3 mutations in Korean patients with acute myeloid leukemia. J Korean Med Sci 23(5):833–837
Sekeres MA, Peterson B, Dodge RK et al (2004) Differences in prognostic factors and outcomes in African Americans and whites with acute myeloid leukemia. Blood 103(11):4036–4042
Darbinyan K, Shastri A, Budhathoki A et al (2017) Hispanic ethnicity is associated with younger age at presentation but worse survival in acute myeloid leukemia. Blood Adv 1(24):2120–2123
Wei H, Wang Y, Zhou C et al (2018) Distinct genetic alteration profiles of acute myeloid leukemia between Caucasian and Eastern Asian population. J Hematol Oncol 11(1):18
Polite BN, Adams-Campbell LL, Brawley OW et al (2017) Charting the future of cancer health disparities research: a position statement from the American Association for Cancer Research, the American Cancer Society, the American Society of Clinical Oncology, and the National Cancer Institute. J Clin Oncol 35(26):3075–3082
Patel MI, Ma Y, Mitchell BS, Rhoads KF (2012) Understanding disparities in leukemia: a national study. Cancer Causes Control 23(11):1831–1837
Papaemmanuil E, Gerstung M, Bullinger L et al (2016) Genomic classification and prognosis in acute myeloid leukemia. N Engl J Med 374(23):2209–2221
Byrd JC, Mrózek K, Dodge RK, Carroll AJ, Edwards CG, Arthur DC, Pettenati MJ, Patil SR, Rao KW, Watson MS, Koduru PR, Moore JO, Stone RM, Mayer RJ, Feldman EJ, Davey FR, Schiffer CA, Larson RA, Bloomfield CD, Cancer and Leukemia Group B (CALGB 8461) (2002) Pretreatment cytogenetic abnormalities are predictive of induction success, cumulative incidence of relapse, and overall survival in adult patients with de novo acute myeloid leukemia: results from Cancer and Leukemia Group B (CALGB 8461). Blood 100(13):4325–4336
Patel JP, Gönen M, Figueroa ME et al (2012) Prognostic relevance of integrated genetic profiling in acute myeloid leukemia. N Engl J Med 366(12):1079–1089
Cheson BD, Bennett JM, Kopecky KJ et al (2003) Revised recommendations of the international working group for diagnosis, standardization of response criteria, treatment outcomes, and reporting standards for therapeutic trials in acute myeloid leukemia. J Clin Oncol 21(24):4642–4649
Master S, Mansour R, Devarakonda SS, Shi Z, Mills G, Shi R (2016) Predictors of survival in acute myeloid leukemia by treatment modality. Anticancer Res 36(4):1719–1727
Do DP, Zheng C (2017) A marginal structural modeling strategy investigating short and long-term exposure to neighborhood poverty on BMI among U.S. black and white adults. Health Place 46:201–209
Elfassy T, Glymour MM, Kershaw KN et al (2017) Association between sustained poverty and changes in body mass index, 1990–2015: the Coronary Artery Risk Development in Young Adults Study. Am J Epidemiol 187(6):1240–1249
Master S, Munker R, Shi Z, Mills G, Shi R (2016) Insurance status and other non-biological factors predict outcomes in acute myelogenous leukemia: analysis of Data from the National Cancer Database. Anticancer Res 36(9):4915–4921
Döhner K, Schlenk RF, Habdank M et al (2005) Mutant nucleophosmin (NPM1) predicts favorable prognosis in younger adults with acute myeloid leukemia and normal cytogenetics: interaction with other gene mutations. Blood 106(12):3740–3746
Thiede C, Koch S, Creutzig E et al (2006) Prevalence and prognostic impact of NPM1 mutations in 1485 adult patients with acute myeloid leukemia (AML). Blood 107(10):4011–4020
Venditti A, Piciocchi A, Candoni A et al (2019) GIMEMA AML1310 trial of risk-adapted, MRD-directed therapy for young adults with newly diagnosed acute myeloid leukemia. Blood 134(12):935
Ciurea SO, Zhang MJ, Bacigalupo AA et al (2015) Haploidentical transplant with posttransplant cyclophosphamide vs matched unrelated donor transplant for acute myeloid leukemia. Blood 126(8):1033–1040
McCurdy SR, Kasamon YL, Kanakry CG et al (2017) Comparable composite endpoints after HLA-matched and HLA-haploidentical transplantation with post-transplantation cyclophosphamide. Haematologica 102(2):391–400
Byrne MM, Halman LJ, Koniaris LG, Cassileth PA, Rosenblatt JD, Cheung MC (2011) Effects of poverty and race on outcomes in acute myeloid leukemia. Am J Clin Oncol 34(3):297–304
Bhatt VR, Shostrom V, Gundabolu K, Armitage JO (2018) Utilization of initial chemotherapy for newly diagnosed acute myeloid leukemia in the United States. Blood Adv 2(11):1277–1282
Winestone LE, Getz KD, Rao P et al (2019) Disparities in pediatric acute myeloid leukemia (AML) clinical trial enrollment. Leuk Lymphoma 60(9):2190–2198
Ford JG, Howerton MW, Lai GY et al (2008) Barriers to recruiting underrepresented populations to cancer clinical trials: a systematic review. Cancer 112(2):228–242
Statler A, Hobbs B, Radivoyevitch T et al (2019) The impact of comorbidities and organ dysfunction commonly used for clinical trial eligibility criteria on outcome in acute myeloid leukemia (AML) patients receiving induction chemotherapy. Blood 134:16
Bhatnagar B et al (2021) Poor survival and differential impact of genetic features of black patients with acute myeloid leukemia. Cancer Discov 11:626–637
Pulte D, Redaniel MT, Jansen L, Brenner H, Jeffreys M (2013) Recent trends in survival of adult patients with acute leukemia: overall improvements, but persistent and partly increasing disparity in survival of patients from minority groups. Haematologica 98(2):222–229
Utuama O, Mukhtar F, Pham YT-H et al (2019) Racial/ethnic, age and sex disparities in leukemia survival among adults in the United States during 1973–2014 period. PLoS ONE 14(8):e0220864–e0220864
Funding
University of Illinois at Chicago Cancer Center Pilot Grant awarded to Dr. Irum Kha.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflicts of interest to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Abraham, I.E., Patel, A.A., Wang, H. et al. Impact of race on outcomes in intermediate-risk acute myeloid leukemia. Cancer Causes Control 32, 705–712 (2021). https://doi.org/10.1007/s10552-021-01422-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-021-01422-4