Abstract
Purpose
Given the associations between poverty and poorer outcomes among older adults with cancer, we sought to understand the effects of dual enrollment in Medicare and Medicaid—as a marker of poverty—on self-reported care experiences among seniors diagnosed with cancer.
Methods
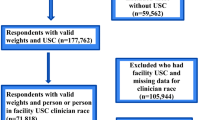
Retrospective, observational study using cancer registry, Medicare claims, and care experience survey data (Surveillance, Epidemiology, and End Results [SEER]—Consumer Assessment of Healthcare Providers and Systems [CAHPS®]) for a national sample of fee-for-service (FFS) and Medicare Advantage (MA) enrollees aged 65 or older. We included people with one incident primary, malignant cancer diagnosed between 2005 and 2011, surveyed within 2 years after diagnosis (n = 9,800; 995 dual enrollees). Medicare CAHPS measures included 5 global ratings and 3 composite scores.
Results
After adjustment for potential confounders, people with cancer histories who were dually enrolled were significantly more likely to report better experiences than non-duals on 2 measures (Medicare/their health plan: adjusted odds ratio [aOR]: 0.68, 95% confidence interval [CI] 0.53–0.87; prescription drug plan [PDP]: aOR: 0.54, 95% CI 0.40–0.73).
Conclusions
Dual enrollees with cancer reported better experiences than Medicare-only enrollees in terms of their health plan (Medicare FFS or Medicare Advantage) and their PDP. Better ratings among dually enrolled beneficiaries suggest possible divergence between health outcomes and care experiences, warranting additional investigation.
Similar content being viewed by others
References
Marmot MG, Bell R (2009) Action on health disparities in the United States: commission on social determinants of health. JAMA 301:1169–1171
Andrulis DP (1998) Access to care is the center piece in the elimination of socioeconomic disparities in health. Ann Internal Med 129:412–416
Siminoff LA, Ross L (2005) Access and equity to cancer care in the USA: a review and assessment. Postgrad Med J 81:674–679
Koroukian SM, Xu F, Dor A, Cooper GS (2006) Colorectal cancer screening in the elderly population: disparities by dual Medicare-Medicaid enrollment status. Health Serv Res 41:2136–2154
Boscoe FP, Henry KA, Sherman RL, Johnson CJ (2016) The relationship between cancer incidence, stage and poverty in the United States. Int J Cancer 139:607–612
Bradley CJ, Dahman B, Given CW (2008) Treatment and survival differences in older Medicare patients with lung cancer as compared with those who are dually eligible for Medicare and Medicaid. J Clin Oncol 26:5067–5073
Carcaise-Edinboro P, Bradley CJ, Dahman B (2010) Surveillance mammography for Medicaid/Medicare breast cancer patients. J Cancer Surviv 4:59–66
Doll KM, Meng K, Basch EM, Gehrig PA, Brewster WR, Meyer AM (2015) Gynecologic cancer outcomes in the elderly poor: a population-based study. Cancer 121:3591–3599
Kirby J, Berdahl T (2012) Indicators of health care quality by income and insurance status among individuals with a usual source of care, 2009. https://meps.ahrq.gov/mepsweb/data_files/publications/st367/stat367.shtml. Accessed 24 Mar 2014.
Ahmed S, Shahid RK (2012) Disparity in cancer care: a Canadian perspective. Curr Oncol 19:e376–e382
National Cancer Institute (2017) Health disparities. https://cancercontrol.cancer.gov/research-emphasis/health-disparities.html. Accessed 7 Feb 2018.
Kaiser Family Foundation (2015) State health facts: Medicare dual eligibles. Kaiser Family Foundation, San Franciso, CA
MedPAC. Dual eligible beneficiaries: an overview. Report to the congress: New approaches in Medicare, Chapter 3, pp 71–94
Stefanacci RG (2011) Improving the care of “dual eligibles”— what’s ahead. Ann Long Term Care Clinic Care Aging 19(9):26–30
MedPAC. (2016) Data book: beneficiaries dually eligible for Medicare and Medicaid. https://medpac.gov/docs/default-source/publications/january-2016-medpac-and-macpac-data-book-beneficiaries-dually-eligible-for-Medicare-and-Medicaid.pdf?sfvrsn=0. Accessed 20 Jun 2019.
Berwick DM, Nolan TW, Whittington J (2008) The triple aim: care, health, and cost. Health Aff 27:759–769
Mollica MA, Lines LM, Halpern MT et al (2017) Patient experiences of cancer care: scoping review, future directions, and introduction of a new data resource: surveillance epidemiology and end results-consumer assessment of healthcare providers and systems (SEER-CAHPS). Patient Exp J 4:103–121
Chawla N, Urato M, Ambs A et al (2015) Unveiling Seer-Cahps®: a new data resource for quality of care research. J Gen Intern Med 30:641–650
Halpern MT, Urato MP, Kent EE (2017) The health care experience of patients with cancer during the last year of life: analysis of the SEER-CAHPS data set. Cancer 123:336–344
National Cancer Institute (2016) SEER-Medicare publications by journal & year. National Cancer Institute, Bethesda, MA
Elliott MN, Haviland AM, Orr N, Hambarsoomian K, Cleary PD (2011) How do the experiences of Medicare beneficiary subgroups differ between managed care and original Medicare? Health Serv Res 46:1039–1058
National Cancer Institute (2017) Medicare CAHPS response rates. National Cancer Institute, Bethesda, MA
Martino SC, Elliott MN, Cleary PD et al (2009) Psychometric properties of an instrument to assess Medicare beneficiaries' prescription drug plan experiences. Health Care Financ Rev 30:41–53
National Cancer Institute (2017) SEER-CAHPS data documentation. National Cancer Institute, Bethesda, MA
Damiano PC, Elliott M, Tyler MC, Hays RD (2004) Differential use of the CAHPS® 0–10 global rating scale by Medicaid and commercial populations. Health Serv Outcomes Res Methodol 5:193–205
Halpern MT, Urato MP, Kent EE (2016) The health care experience of patients with cancer during the last year of life: analysis of the SEER-CAHPS data set. Cancer 123:336–344
Hargraves JL, Hays RD, Cleary PD (2003) Psychometric properties of the consumer assessment of health plans study (CAHPS) 2.0 adult core survey. Health Serv Res 38:1509–1527
Macias C, Gold PB, Öngür D, Cohen BM, Panch T (2015) Are single-item global ratings useful for assessing health status? J Clin Psychol Med Settings 22:251–264
Ware J, Kosinski M, Gandek B (2003) SF-36 health survey: manual & interpretation guide. Quality Metric Inc, Lincoln, RI
Zaborski LB, Zaslavsky AM (2012) MCAHPS Technical Report, appendix 2.04: individual-level weight construction. RAND, Santa Monica, CA
Warren JL, Butler EN, Stevens J et al (2015) Receipt of chemotherapy among Medicare patients with cancer by type of supplemental insurance. J Clin Oncol 33:312–318
Elliott MN, Haviland AM, Kanouse DE, Hambarsoomian K, Hays RD (2009) Adjusting for subgroup differences in extreme response tendency in ratings of health care: impact on disparity estimates. Health Serv Res 44:542–561
Allen SM, Piette ER, Mor V (2014) The adverse consequences of unmet need among older persons living in the community: dual-eligible versus Medicare-only beneficiaries. J Gerontol B 69(Suppl 1):S51–S58
Priest J, Buikema A, Engel-Nitz NM, Cook CL, Cantrell CR (2012) Quality of care, health care costs, and utilization among Medicare part D enrollees with and without low-income subsidy. Popul Health Manag 15:101–112
Rahman M, Grabowski DC, Gozalo PL, Thomas KS, Mor V (2014) Are dual eligibles admitted to poorer quality skilled nursing facilities? Health Serv Res 49:798–817
Koroukian SM, Bakaki PM, Owusu C, Earle CC, Cooper GS (2012) Cancer outcomes in low-income elders: is there an advantage to being on Medicaid? Medicare Medicaid Res Rev 2:2
Elliott M, Swartz R, Adams J, Spritzer K, Hays R (2001) Consumer evaluations of health plans and health care providers. Case-mix adjustment of the national CAHPS benchmarking data 10: a violation of model assumptions? Health Serv Res 36:555–574
O'Malley AJ, Zaslavsky AM, Elliott MN, Zaborski L, Cleary PD (2005) Case-mix adjustment of the CAHPS® hospital survey. Health Serv Res 40:2162–2181
Potetz L, DeWilde LF (2009) Cancer and Medicare: a chartbook. American Cancer Society Cancer Action Network, Washington, DC
Elliott MN, Beckett MK, Chong K, Hambarsoomians K, Hays RD (2008) How do proxy responses and proxy-assisted responses differ from what Medicare beneficiaries might have reported about their health care? Health Serv Res 43:833–848
Funding
Funding for this research was provided to LML, JC, and MTH under National Cancer Institute Contract #HHSN-261–2015-00132U.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Dr. Halpern was employed by RTI International and Temple University at the time of this study’s initial submission. He is now employed by the National Cancer Institute. At the time of initial submission, Dr. Kent was affiliated with the National Cancer Institute.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lines, L.M., Cohen, J., Halpern, M.T. et al. Care experiences among dually enrolled older adults with cancer: SEER-CAHPS, 2005–2013. Cancer Causes Control 30, 1137–1144 (2019). https://doi.org/10.1007/s10552-019-01218-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-019-01218-7