Abstract
Purpose
This study compared the demographic and clinicopathologic characteristics and risk of mortality between the triple positive (TP) and ER+/PR+/HER2− breast cancer subtypes.
Methods
Cases of first primary female invasive TP and ER+/PR+/HER2− breast cancer were obtained from the California Cancer Registry. Logistic regression analysis was used to compare differences in factors associated with the TP versus the ER+/PR+/HER2− subtype. Cox regression was used to compute the adjusted risk of breast cancer-specific mortality of the TP versus ER+/PR+/HER2−.
Results
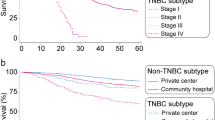
The odds of TP versus ER+/PR+/HER2− were higher with advanced stage, high grade, low SES, ≤ 45 years of age (OR 1.48; CI 1.40–1.55), black (OR 1.11; CI 1.02–1.21), Asian/Pacific Islander (OR 1.15; CI 1.09–1.22), and uninsured (OR 1.42; CI 1.15–1.73). Unadjusted survival analysis indicated worse survival for the TP when compared with the ER+/PR+/HER2− subtype. However, adjusted risk of mortality for the TP subtype was not statistically significantly worse than the ER+/PR+/HER2− subtype.
Conclusions
Young age, advanced stage and grade, low SES, black and API race, and lack of health insurance are more common in the TP subtype than in the ER+/PR+/HER2− subtype. However the risk of mortality between these two subtypes is similar.

Similar content being viewed by others
References
Parise CA, Bauer KR, Brown MM, Caggiano V (2009) Breast cancer subtypes as defined by the estrogen receptor (ER), progesterone receptor (PR), and the human epidermal growth factor receptor 2 (HER2) among women with invasive breast cancer in California, 1999–2004. Breast J 15:593–602
Parise CA, Caggiano V (2014) Breast cancer survival defined by the ER/PR/HER2 subtypes and a surrogate classification according to tumor grade and immunohistochemical biomarkers. J. Cancer Epidemiol 2014:469251
Bauer KR, Brown M, Cress RD, Parise CA, Caggiano V (2007) Descriptive analysis of estrogen receptor (ER)-negative, progesterone receptor (PR)-negative, and HER2-negative invasive breast cancer, the so-called triple-negative phenotype: a population-based study from the California cancer Registry. Cancer 109:1721–1728
Boyle P (2012) Triple-negative breast cancer: epidemiological considerations and recommendations. Ann Oncol 23(Suppl 6):vi7–12
Liao HY, Zhang WW, Sun JY, Li FY, He ZY, Wu SG (2018) The clinicopathological features and survival outcomes of different histological subtypes in triple-negative breast cancer. J Cancer 9:296–303
Carey LA, Perou CM, Livasy CA et al (2006) Race, breast cancer subtypes, and survival in the Carolina Breast Cancer Study. JAMA 295:2492–2502
Parise CA, Caggiano V (2017) Risk factors associated with the triple-negative breast cancer subtype within four race/ethnicities. Breast Cancer Res Treat 163:151–158
Cheang MC, Chia SK, Voduc D et al (2009) Ki67 index, HER2 status, and prognosis of patients with luminal B breast cancer. J Natl Cancer Inst 101:736–750
Urru SAM, Gallus S, Bosetti C et al (2018) Clinical and pathological factors influencing survival in a large cohort of triple-negative breast cancer patients. BMC Cancer 18:56
Zhao S, Ma D, Xiao Y, Jiang YZ, Shao ZM (2018) Clinicopathologic features and prognoses of different histologic types of triple-negative breast cancer: a large population-based analysis. Eur J Surg Oncol 44(4):420–428
Fritz AG (2000) International classification of diseases for oncology: ICD-O, 3rd edn. World Health Organization, Geneva, pp. vi, 239
California Department of Public, Cancer Surveillance and Research Branch (2008) Cancer reporting in California: abstracting and coding procedures for hospitals. California cancer reporting system standards, vol. I. California Department of Public, Cancer Surveillance and Research Branch, Sacramento
ICD10Data.com. http://www.icd10.com. Accessed Jan 2016
DAKO HERCEPTest® 2019 [March, 2019]; 11th: Available from: https://www.agilent.com/cs/library/packageinsert/public/PD04086US_01.pdf.
PathVision HER-2 DNA Probe Kit Package Insert. 2016 [March, 2019]; Available from: https://www.molecular.abbott/us/en/products/oncology/pathvysion-her-2-dna-probe-kit
American Community Survey. U.S. Department of Commerce, United States Census Bureau. https://www.census.gov/programs-surveys/acs/. Accessed Jan 2016
Yost K, Perkins C, Cohen R, Morris C, Wright W (2001) Socioeconomic status and breast cancer incidence in California for different race/ethnic groups. Cancer Causes Control 12:703–711
Clarke CA, Glaser SL, Keegan TH, Stroup A (2005) Neighborhood socioeconomic status and Hodgkin’s lymphoma incidence in California. Cancer Epidemiol Biomark Prev 14:1441–1447
Parikh-Patel A, Bates JH, Campleman S (2006) Colorectal cancer stage at diagnosis by socioeconomic and urban/rural status in California, 1988–2000. Cancer 107:1189–1195
Zell JA, Rhee JM, Ziogas A, Lipkin SM, Anton-Culver H (2007) Race, socioeconomic status, treatment, and survival time among pancreatic cancer cases in California. Cancer Epidemiol Biomark Prev 16:546–552
Brown M, Tsodikov A, Bauer KR, Parise CA, Caggiano V (2008) The role of human epidermal growth factor receptor 2 in the survival of women with estrogen and progesterone receptor-negative, invasive breast cancer: The California Cancer Registry, 1999–2004. Cancer 112:737–747
Ou SH, Zell JA, Ziogas A, Anton-Culver H (2008) Low socioeconomic status is a poor prognostic factor for survival in stage I nonsmall cell lung cancer and is independent of surgical treatment, race, and marital status. Cancer 112:2011–2020
Yin D, Morris C, Allen M, Cress R, Bates J, Liu L (2010) Does socioeconomic disparity in cancer incidence vary across racial/ethnic groups? Cancer Causes Control 21:1721–1730
Telli ML, Chang ET, Kurian AW et al (2011) Asian ethnicity and breast cancer subtypes: a study from the California Cancer Registry. Breast Cancer Res Treat 127:471–478
Parise CA, Bauer KR, Caggiano V (2012) Disparities in receipt of adjuvant radiation therapy after breast-conserving surgery among the cancer-reporting regions of California. Cancer 118:2516–2524
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Hosmer D, Lemeshow S (1989) Applied logistic regression. Wiley, New York
IBM Corp (2012) IBM SPSS statistics for Windows, vol 21.0. IBM Corp., Armonk
Alqaisi A, Chen L, Romond E et al (2014) Impact of estrogen receptor (ER) and human epidermal growth factor receptor-2 (HER2) co-expression on breast cancer disease characteristics: implications for tumor biology and research. Breast Cancer Res Treat 148:437–444
Alwan NAS, Mualla FH, Al Naqash M, Kathum S, Tawfiq FN, Nadhir S (2017) Clinical and pathological characteristics of triple positive breast cancer among Iraqi patients. Gulf J Oncol 1:51–60
Parise CA, Caggiano V (2017) Risk of mortality of node-negative, ER/PR/HER2 breast cancer subtypes in T1, T2, and T3 tumors. Breast Cancer Res Treat 165:743–750
Tamimi RM, Baer HJ, Marotti J et al (2008) Comparison of molecular phenotypes of ductal carcinoma in situ and invasive breast cancer. Breast Cancer Res 10:R67
Ades F, Zardavas D, Bozovic-Spasojevic I et al (2014) Luminal B breast cancer: molecular characterization, clinical management, and future perspectives. J Clin Oncol 32:2794–2803
Bediaga NG, Beristain E, Calvo B et al (2016) Luminal B breast cancer subtype displays a dicotomic epigenetic pattern. SpringerPlus 5:623
Bhargava R, Dabbs DJ (2008) Luminal B breast tumors are not HER2 positive. Breast Cancer Res 10:404; author reply 5
Goldhirsch A, Wood WC, Coates AS et al (2011) Strategies for subtypes-dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol 22:1736–1747
Sorlie T, Perou CM, Tibshirani R et al (2001) Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc Natl Acad Sci USA 98:10869–10874
Sorlie T, Tibshirani R, Parker J et al (2003) Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci USA 100:8418–8423
Sotiriou C, Neo SY, McShane LM et al (2003) Breast cancer classification and prognosis based on gene expression profiles from a population-based study. Proc Natl Acad Sci USA 100:10393–10398
Creighton CJ (2012) The molecular profile of luminal B breast cancer. Biologics 6:289–297
Acknowledgments
We wish to thank Melissa Taylor and the staff at the Sutter Resource Library for their valuable assistance.
Disclaimer
The collection of cancer incidence data used in this study was supported by the California Department of Public Health as part of the statewide cancer reporting program mandated by California Health and Safety Code Section 103885; the National Cancer Institute’s Surveillance, Epidemiology and End Results Program under contract N01-PC-35136 awarded to the Northern California Cancer Center, contract N01-PC-35139 awarded to the University of Southern California, and contract N01-PC-54404 awarded to the Public Health Institute; and the Centers for Disease Control and Prevention’s National Program of Cancer Registries, under agreement 1U58DP00807-01 awarded to the Public Health Institute. The ideas and opinions expressed herein are those of the authors and endorsement by the State of California, Department of Public Health the National Cancer Institute, and the Centers for Disease Control and Prevention or their contractors and subcontractors is not intended nor should be inferred.
Funding
This study was funded by Grant 947110-1107555 from the Sutter Medical Center Sacramento Foundation.
Author information
Authors and Affiliations
Contributions
CAP and VC equally contributed to the conceptualization, analysis, and writing of this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
This research study involved analysis of existing data from the CCR without subject identifiers or intervention. Therefore, the study was categorized as Exempt from institutional review board oversight.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Parise, C.A., Caggiano, V. Differences in clinicopatholgic characteristics and risk of mortality between the triple positive and ER+/PR+/HER2− breast cancer subtypes. Cancer Causes Control 30, 417–424 (2019). https://doi.org/10.1007/s10552-019-01152-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10552-019-01152-8