Abstract
Purpose
Axillary lymph nodes (LNs) with cortical thickness > 3 mm have a higher likelihood of malignancy. To examine the positive predictive value (PPV) of axillary LN cortical thickness in newly diagnosed breast cancer patients, and nodal, clinical, and tumor characteristics associated with axillary LN metastasis.
Methods
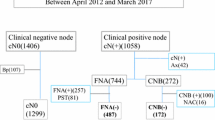
Retrospective review of axillary LN fine needle aspirations (FNAs) performed 1/1/2018–12/31/2019 included 135 axillary FNAs in 134 patients who underwent axillary surgery. Patient demographics, clinical characteristics, histopathology, and imaging features were obtained from medical records. Hypothesis testing was performed to identify predictors of axillary LN metastasis.
Results
Cytology was positive in 72/135 (53.3%), negative in 61/135 (45.2%), and non-diagnostic in 2/135 (1.5%). At surgery, histopathology was positive in 84 (62.2%) and negative in 51 (37.8%). LN cortices were thicker in metastatic compared to negative nodes (p < 0.0001). PPV of axillary LNs with cortical thickness ≥ 3 mm, ≥ 3.5 mm, ≥ 4 mm and, ≥ 4.25 mm was 0.62 [95% CI 0.53, 0.70], 0.63 [0.54, 0.72], 0.67 [0.57, 0.76] , and 0.74 [0.64, 0.83], respectively. At multivariable analysis, abnormal hilum (OR = 3.44, p = 0.016) and diffuse cortical thickening (OR = 2.86, p = 0.038) were associated with nodal metastasis.
Conclusion
In newly diagnosed breast cancer patients, increasing axillary LN cortical thickness, abnormal fatty hilum, and diffuse cortical thickening are associated with nodal metastasis. PPV of axillary LN cortical thickness ≥ 3 mm and ≥ 3.5 mm is similar but increases for cortical thickness ≥ 4 mm. FNA of axillary LNs with cortex < 4 mm may be unnecessary for some patients undergoing sentinel LN biopsy.



Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publically available due to HIPPA and IRB but are available from the corresponding author on reasonable request.
Abbreviations
- LN :
-
Lymph node
- PPV :
-
Positive predictive value
- CI :
-
Confidence interval
- FNA :
-
Fine needle aspiration
- IDC :
-
Invasive ductal carcinoma
- ILC :
-
Invasive lobular carcinoma
- IDLC :
-
Invasive carcinoma with ductal and lobular features
- DCIS :
-
Ductal carcinoma in situ
- SLNB :
-
Sentinel lymph node biopsy
- ALND :
-
Axillary lymph node dissection
- US :
-
Ultrasound
References
Carter CL, Allen C, Henson DE (1989) Relation of tumor size, lymph node status, and survival in 24,740 breast cancer cases. Cancer 63:181–187
Collan YU, Eskelinen MJ, Nordling SA, Lipponen P, Pesonen E, Kumpusalo LM, Pajarinen P, Kettunen KO (1994) Prognostic studies in breast cancer. Multivariate combination of nodal status, proliferation index, tumor size, and DNA ploidy. Acta Oncol 33:873–878. https://doi.org/10.3109/02841869409098449
Rivadeneira DE, Simmons RM, Christos PJ, Hanna K, Daly JM, Osborne MP (2000) Predictive factors associated with axillary lymph node metastases in T1a and T1b breast carcinomas: analysis in more than 900 patients. J Am Coll Surg 191:1–6. https://doi.org/10.1016/s1072-7515(00)00310-0
Pilewskie ML, Morrow M (2014) Management of the clinically node-negative axilla: what have we learned from the clinical trials? Oncology 28:371–378
Krag DN, Anderson SJ, Julian TB, Brown AM, Harlow SP, Costantino JP, Ashikaga T, Weaver DL, Mamounas EP, Jalovec LM, Frazier TG, Noyes RD, Robidoux A, Scarth HM, Wolmark N (2010) Sentinel-lymph-node resection compared with conventional axillary-lymph-node dissection in clinically node-negative patients with breast cancer: overall survival findings from the NSABP B-32 randomised phase 3 trial. Lancet Oncol 11:927–933. https://doi.org/10.1016/S1470-2045(10)70207-2
Bromham N, Schmidt-Hansen M, Astin M, Hasler E, Reed MW (2017) Axillary treatment for operable primary breast cancer. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD004561.pub3
Garcia-Etienne CA, Ferrari A, Della Valle A, Lucioni M, Ferraris E, Di Giulio G, Squillace L, Bonzano E, Lasagna A, Rizzo G, Tancredi R, Scotti Foglieni A, Dionigi F, Grasso M, Arbustini E, Cavenaghi G, Pedrazzoli P, Filippi AR, Dionigi P, Sgarella A (2020) Management of the axilla in patients with breast cancer and positive sentinel lymph node biopsy: An evidence-based update in a European breast center. Eur J Surg Oncol 46:15–23. https://doi.org/10.1016/j.ejso.2019.08.013
Giuliano AE, Ballman KV, McCall L, Beitsch PD, Brennan MB, Kelemen PR, Ollila DW, Hansen NM, Whitworth PW, Blumencranz PW, Leitch AM, Saha S, Hunt KK, Morrow M (2017) Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: The ACOSOG Z0011 (Alliance) randomized clinical trial. JAMA 318:918–926. https://doi.org/10.1001/jama.2017.11470
Giuliano AE, Hunt KK, Ballman KV, Beitsch PD, Whitworth PW, Blumencranz PW, Leitch AM, Saha S, McCall LM, Morrow M (2011) Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA 305:569–575. https://doi.org/10.1001/jama.2011.90
Magnoni F, Galimberti V, Corso G, Intra M, Sacchini V, Veronesi P (2020) Axillary surgery in breast cancer: An updated historical perspective. Semin Oncol 47:341–352. https://doi.org/10.1053/j.seminoncol.2020.09.001
Boughey JC, Suman VJ, Mittendorf EA, Ahrendt GM, Wilke LG, Taback B, Leitch AM, Kuerer HM, Bowling M, Flippo-Morton TS, Byrd DR, Ollila DW, Julian TB, McLaughlin SA, McCall L, Symmans WF, Le-Petross HT, Haffty BG, Buchholz TA, Nelson H, Hunt KK, Alliance for Clinical Trials in O, (2013) Sentinel lymph node surgery after neoadjuvant chemotherapy in patients with node-positive breast cancer: the ACOSOG Z1071 (Alliance) clinical trial. JAMA 310:1455–1461. https://doi.org/10.1001/jama.2013.278932
Sacre RA (1986) Clinical evaluation of axillary lymph nodes compared to surgical and pathological findings. Eur J Surg Oncol 12:169–173
Marino MA, Avendano D, Zapata P, Riedl CC, Pinker K (2020) Lymph node imaging in patients with primary breast cancer: concurrent diagnostic tools. Oncologist 25:e231–e242. https://doi.org/10.1634/theoncologist.2019-0427
Weiss A, King C, Vincuilla J, Parker T, Portnow L, Nakhlis F, Dominici L, Mittendorf EA, King TA (2022) Rates of pathologic nodal disease among cN0 and cN1 patients undergoing routine axillary ultrasound and neoadjuvant chemotherapy. Breast Cancer Res Treat 195:181–189. https://doi.org/10.1007/s10549-022-06677-2
Mainiero MB, Cinelli CM, Koelliker SL, Graves TA, Chung MA (2010) Axillary ultrasound and fine-needle aspiration in the preoperative evaluation of the breast cancer patient: an algorithm based on tumor size and lymph node appearance. AJR Am J Roentgenol 195:1261–1267. https://doi.org/10.2214/AJR.10.4414
Leenders MW, Broeders M, Croese C, Richir MC, Go HL, Langenhorst BL, Meijer S, Schreurs WH (2012) Ultrasound and fine needle aspiration cytology of axillary lymph nodes in breast cancer. To do or not to do? Breast 21:578–583. https://doi.org/10.1016/j.breast.2012.05.008
Preda T, McGrath R, Bingham J, Fawcett A, O’Dea C, Bochner M, Gill PG, Kollias J (2020) How much does axillary ultrasound contribute in women undergoing breast-conserving surgery with no palpable axillary nodes? ANZ J Surg 90:1146–1150. https://doi.org/10.1111/ans.15680
Hieken TJ, Trull BC, Boughey JC, Jones KN, Reynolds CA, Shah SS, Glazebrook KN (2013) Preoperative axillary imaging with percutaneous lymph node biopsy is valuable in the contemporary management of patients with breast cancer. Surgery 154:831–838. https://doi.org/10.1016/j.surg.2013.07.017
Liu M, Yang Y, Xie F, Guo J, Wang S, Yang H, Wang S (2019) Could axillary clearance be avoided in clinically node-negative breast cancer patients with positive nodes diagnosed by ultrasound guided biopsy in the post-ACOSOG Z0011 era? PLoS ONE. https://doi.org/10.1371/journal.pone.0210437
Pilewskie M, Mautner SK, Stempel M, Eaton A, Morrow M (2016) Does a positive axillary lymph node needle biopsy result predict the need for an axillary lymph node dissection in clinically node-negative breast cancer patients in the ACOSOG Z0011 era? Ann Surg Oncol 23:1123–1128. https://doi.org/10.1245/s10434-015-4944-y
National Comprehensive Cancer Network: Breast Cancer (Version 4.2022). In:
Mittendorf EA, Kantor O, Weiss A, Richardson E, Garrido-Castro A, Portnow LH, Krop IE, Lin NU, Winer EP, Tolaney SM, King TA (2023) Nodal positivity in early-stage triple-negative breast cancer: implications for preoperative immunotherapy. Ann Surg Oncol 30:100–106. https://doi.org/10.1245/s10434-022-12357-8
Weiss A, Martinez-Saez O, Waks AG, Laws A, McGrath M, Tarantino P, Portnow L, Winer E, Rey M, Tapia M, Prat A, Partridge AH, Tolaney SM, Cejalvo JM, Mittendorf EA, King TA (2023) Nodal positivity and systemic therapy among patients with clinical T1–T2N0 human epidermal growth factor receptor-positive breast cancer: Results from two international cohorts. Cancer 129:1836–1845. https://doi.org/10.1002/cncr.34750
Alvarez S, Anorbe E, Alcorta P, Lopez F, Alonso I, Cortes J (2006) Role of sonography in the diagnosis of axillary lymph node metastases in breast cancer: a systematic review. AJR Am J Roentgenol 186:1342–1348. https://doi.org/10.2214/AJR.05.0936
Krishnamurthy S, Sneige N, Bedi DG, Edieken BS, Fornage BD, Kuerer HM, Singletary SE, Hunt KK (2002) Role of ultrasound-guided fine-needle aspiration of indeterminate and suspicious axillary lymph nodes in the initial staging of breast carcinoma. Cancer 95:982–988. https://doi.org/10.1002/cncr.10786
Tahir M, Osman KA, Shabbir J, Rogers C, Suarez R, Reynolds T, Bucknall T (2008) Preoperative axillary staging in breast cancer-saving time and resources. Breast J 14:369–371. https://doi.org/10.1111/j.1524-4741.2008.00600.x
Liu XS (2017) Common language effect size for multiple treatment comparisons. Meas Eval Couns Dev 48:238–243. https://doi.org/10.1177/0748175615578739
Boughey JC, Ballman KV, Le-Petross HT, McCall LM, Mittendorf EA, Ahrendt GM, Wilke LG, Taback B, Feliberti EC, Hunt KK (2016) Identification and resection of clipped node decreases the false-negative rate of sentinel lymph node surgery in patients presenting with node-positive breast cancer (T0–T4, N1–N2) who receive neoadjuvant chemotherapy: results from ACOSOG Z1071 (Alliance). Ann Surg 263:802–807. https://doi.org/10.1097/SLA.0000000000001375
Simons JM, van Pelt M, Marinelli A, Straver ME, Zeillemaker AM, Pereira Arias-Bouda LM, van Nijnatten TJA, Koppert LB, Hunt KK, Smidt ML, Luiten EJT, van der Pol CC (2019) Excision of both pretreatment marked positive nodes and sentinel nodes improves axillary staging after neoadjuvant systemic therapy in breast cancer. Br J Surg 106:1632–1639. https://doi.org/10.1002/bjs.11320
Cho N, Moon WK, Han W, Park IA, Cho J, Noh DY (2009) Preoperative sonographic classification of axillary lymph nodes in patients with breast cancer: node-to-node correlation with surgical histology and sentinel node biopsy results. AJR Am J Roentgenol 193:1731–1737. https://doi.org/10.2214/AJR.09.3122
Zhu Y, Zhou W, Zhou JQ, Fei XC, Ye TJ, Huang O, Chen XS, Zhan WW (2016) Axillary staging of early-stage invasive breast cancer by ultrasound-guided fine-needle aspiration cytology: which ultrasound criteria for classifying abnormal lymph nodes should be adopted in the post-ACOSOG Z0011 trial era? J Ultrasound Med 35:885–893. https://doi.org/10.7863/ultra.15.06019
Ewing DE, Layfield LJ, Joshi CL, Travis MD (2015) Determinants of false-negative fine-needle aspirates of axillary lymph nodes in women with breast cancer: lymph node size, cortical thickness and hilar fat retention. Acta Cytol 59:311–314. https://doi.org/10.1159/000440797
Schmid P, Cortes J, Pusztai L, McArthur H, Kummel S, Bergh J, Denkert C, Park YH, Hui R, Harbeck N, Takahashi M, Foukakis T, Fasching PA, Cardoso F, Untch M, Jia L, Karantza V, Zhao J, Aktan G, Dent R, O’Shaughnessy J, Investigators K (2020) Pembrolizumab for early triple-negative breast cancer. N Engl J Med 382:810–821. https://doi.org/10.1056/NEJMoa1910549
Nanda R, Liu MC, Yau C, Shatsky R, Pusztai L, Wallace A, Chien AJ, Forero-Torres A, Ellis E, Han H, Clark A, Albain K, Boughey JC, Jaskowiak NT, Elias A, Isaacs C, Kemmer K, Helsten T, Majure M, Stringer-Reasor E, Parker C, Lee MC, Haddad T, Cohen RN, Asare S, Wilson A, Hirst GL, Singhrao R, Steeg K, Asare A, Matthews JB, Berry S, Sanil A, Schwab R, Symmans WF, van ’t Veer L, Yee D, DeMichele A, Hylton NM, Melisko M, Perlmutter J, Rugo HS, Berry DA, Esserman LJ, (2020) Effect of pembrolizumab plus neoadjuvant chemotherapy on pathologic complete response in women with early-stage breast cancer: an analysis of the ongoing phase 2 adaptively randomized I-SPY2 trial. JAMA Oncol 6:676–684. https://doi.org/10.1001/jamaoncol.2019.6650
Abe H, Schmidt RA, Kulkarni K, Sennett CA, Mueller JS, Newstead GM (2009) Axillary lymph nodes suspicious for breast cancer metastasis: sampling with US-guided 14-gauge core-needle biopsy–clinical experience in 100 patients. Radiology 250:41–49. https://doi.org/10.1148/radiol.2493071483
Bedi DG, Krishnamurthy R, Krishnamurthy S, Edeiken BS, Le-Petross H, Fornage BD, Bassett RL Jr, Hunt KK (2008) Cortical morphologic features of axillary lymph nodes as a predictor of metastasis in breast cancer: in vitro sonographic study. AJR Am J Roentgenol 191:646–652. https://doi.org/10.2214/AJR.07.2460
Chung HL, Tso HH, Middleton LP, Sun J, Leung JWT (2022) Axillary nodal metastases in invasive lobular carcinoma versus invasive ductal carcinoma: comparison of node detection and morphology by ultrasound. AJR Am J Roentgenol 218:33–41. https://doi.org/10.2214/AJR.21.26135
Balasubramanian I, Fleming CA, Corrigan MA, Redmond HP, Kerin MJ, Lowery AJ (2018) Meta-analysis of the diagnostic accuracy of ultrasound-guided fine-needle aspiration and core needle biopsy in diagnosing axillary lymph node metastasis. Br J Surg 105:1244–1253. https://doi.org/10.1002/bjs.10920
Bhandari A, Xia E, Wang Y, Sindan N, Kc R, Guan Y, Lin Y-L, Wang X, Zhang X, Wang O (2018) Impact of sentinel lymph node biopsy in newly diagnosed invasive breast cancer patients with suspicious node: a comparative accuracy survey of fine-needle aspiration biopsy versus core-needle biopsy. Am J of Transl Res 10:1860–1873
Rautiainen S, Masarwah A, Sudah M, Sutela A, Pelkonen O, Joukainen S, Sironen R, Karja V, Vanninen R (2013) Axillary lymph node biopsy in newly diagnosed invasive breast cancer: comparative accuracy of fine-needle aspiration biopsy versus core-needle biopsy. Radiology 269:54–60. https://doi.org/10.1148/radiol.13122637
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to the study conception and design. Material preparation, data collection, and analysis were performed by Allyson L. Chesebro MD, Anne-Sophie T. Loonis MD, and Camden P. Bay PhD. The first draft of the manuscript was written by Anne-Sophie T. Loonis MD and Allyson L. Chesebro MD and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have not disclosed any competing interests.
Ethics approval
This study was approved by the appropriate institutional review board with waiver of informed consent (IRB protocol number 17-109).
Competing Interests
The authors have no relevant financial or non-financial interests to disclose.
Consent to participate
This study was approved by the appropriate institutional review board with waiver of informed consent (IRB protocol number 17-109).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Loonis, AS.T., Chesebro, A.L., Bay, C.P. et al. Positive predictive value of axillary lymph node cortical thickness and nodal, clinical, and tumor characteristics in newly diagnosed breast cancer patients. Breast Cancer Res Treat 203, 511–521 (2024). https://doi.org/10.1007/s10549-023-07155-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-07155-z