Abstract
Purpose
We studied women enrolled in the Boston Mammography Cohort Study to investigate whether subgroups defined by age, race, or family history of breast cancer experienced differences in the incidence of screening or diagnostic imaging rates during the COVID-19 lockdown and had slower rebound in the incidence of these rates during reopening.
Methods
We compared the incidence of monthly breast cancer screening and diagnostic imaging rates over during the pre-COVID-19 (January 2019–February 2020), lockdown (March–May 2020), and reopening periods (June–December 2020), and tested for differences in the monthly incidence within the same period by age (< 50 vs ≥ 50), race (White vs non-White), and first-degree family history of breast cancer (yes vs no).
Results
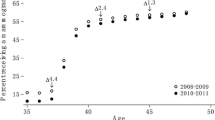
Overall, we observed a decline in breast cancer screening and diagnostic imaging rates over the three time periods (pre-COVID-19, lockdown, and reopening). The monthly incidence of breast cancer screening rates for women age ≥ 50 was 5% higher (p = 0.005) in the pre-COVID-19 period (January 2019–February 2020) but was 19% lower in the reopening phase (June–December 2020) than that of women aged < 50 (p < 0.001). White participants had 36% higher monthly incidence of breast cancer diagnostic imaging rates than non-White participants (p = 0.018).
Conclusion
The rebound in screening was lower in women age ≥ 50 and lower in non-White women for diagnostic imaging. Careful attention must be paid as the COVID-19 recovery continues to ensure equitable resumption of care.


Similar content being viewed by others
Data availability
Data used here may be requested through the Boston Mammography Cohort Study research team upon request and approval of the institutional IRB. The data are not publicly available to protect the privacy of research participants.
References
A Timeline of COVID-19 Developments in 2020. AJMC. Accessed April 25, 2022. https://www.ajmc.com/view/a-timeline-of-covid19-developments-in-2020
Moreland A, Herlihy C, Tynan MA et al (2020) Timing of state and territorial COVID-19 stay-at-home orders and changes in population movement—United States, March 1–May 31, 2020. Morb Mortal Wkly Rep 69(35):1198–1203. https://doi.org/10.15585/mmwr.mm6935a2
Vanni G, Pellicciaro M, Materazzo M et al (2020) Lockdown of breast cancer screening for COVID-19: possible scenario. In Vivo 34(5):3047–3053. https://doi.org/10.21873/invivo.12139
Freer PE (2021) The impact of the COVID-19 pandemic on breast imaging. Radiol Clin North Am 59(1):1–11. https://doi.org/10.1016/j.rcl.2020.09.008
Naidich JJ, Boltyenkov A, Wang JJ, Chusid J, Hughes D, Sanelli PC (2020) Impact of the coronavirus disease 2019 (COVID-19) pandemic on imaging case volumes. J Am Coll Radiol 17(7):865–872. https://doi.org/10.1016/j.jacr.2020.05.004
Papautsky EL, Hamlish T (2020) Patient-reported treatment delays in breast cancer care during the COVID-19 pandemic. Breast Cancer Res Treat 184(1):249–254. https://doi.org/10.1007/s10549-020-05828-7
London JW, Fazio-Eynullayeva E, Palchuk MB, Sankey P, McNair C (2020) Effects of the COVID-19 pandemic on cancer-related patient encounters. JCO Clin Cancer Inform 4:657–665. https://doi.org/10.1200/CCI.20.00068
Maringe C, Spicer J, Morris M et al (2020) The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol 21(8):1023–1034. https://doi.org/10.1016/S1470-2045(20)30388-0
Kaufman HW, Chen Z, Niles J, Fesko Y (2020) Changes in the number of us patients with newly identified cancer before and during the coronavirus disease 2019 (COVID-19) pandemic. JAMA Netw Open 3(8):e2017267. https://doi.org/10.1001/jamanetworkopen.2020.17267
Patt D, Gordan L, Diaz M et al (2020) Impact of COVID-19 on cancer care: how the pandemic is delaying cancer diagnosis and treatment for american seniors. JCO Clin Cancer Inform 4:1059–1071. https://doi.org/10.1200/CCI.20.00134
Nyante SJ, Benefield TS, Kuzmiak CM, Earnhardt K, Pritchard M, Henderson LM (2021) Population-level impact of coronavirus disease 2019 on breast cancer screening and diagnostic procedures. Cancer 127(12):2111–2121. https://doi.org/10.1002/cncr.33460
Epstein MM, Sundaresan D, Fair M et al (2022) Trends in breast and prostate cancer screening and diagnostic procedures during the COVID-19 pandemic in central Massachusetts. Cancer Causes Control 33(10):1313–1323. https://doi.org/10.1007/s10552-022-01616-4
Moraliyage H, De Silva D, Ranasinghe W et al (2021) Cancer in lockdown: impact of the COVID-19 pandemic on patients with cancer. Oncologist 26(2):e342–e344. https://doi.org/10.1002/onco.13604
Vanni G, Materazzo M, Pellicciaro M et al (2020) Breast cancer and COVID-19: the effect of fear on patients’ decision-making process. In Vivo 34:1651–1659. https://doi.org/10.21873/invivo.11957
Lo CH, Nguyen LH, Drew DA et al (2021) Race, ethnicity, community-level socioeconomic factors, and risk of COVID-19 in the United States and the United Kingdom. eClinicalMedicine. https://doi.org/10.1016/j.eclinm.2021.101029
Smith AC, Woerner J, Perera R, Haeny AM, Cox JM (2022) An investigation of associations between race, ethnicity, and past experiences of discrimination with medical mistrust and COVID-19 protective strategies. J Racial Ethn Health Disparities 9(4):1430–1442. https://doi.org/10.1007/s40615-021-01080-x
Louis-Jean J, Cenat K, Njoku CV, Angelo J, Sanon D (2020) Coronavirus (COVID-19) and racial disparities: a perspective analysis. J Racial Ethn Health Disparities 7(6):1039–1045. https://doi.org/10.1007/s40615-020-00879-4
Ojikutu BO, Bogart LM, Dong L (2022) Mistrust, empowerment, and structural change: lessons we should be learning from COVID-19. Am J Public Health 112(3):401–404. https://doi.org/10.2105/AJPH.2021.306604
Du S, Carfang L, Restrepo E et al (2022) Patient-reported experiences of breast cancer screening, diagnosis, and treatment delay, and telemedicine adoption during COVID-19. Curr Oncol Tor Ont 29(8):5919–5932. https://doi.org/10.3390/curroncol29080467
Fedewa SA, Cotter MM, Wehling KA, Wysocki K, Killewald R, Makaroff L (2021) Changes in breast cancer screening rates among 32 community health centers during the COVID-19 pandemic. Cancer 127(23):4512–4515. https://doi.org/10.1002/cncr.33859
Marcondes FO, Cheng D, Warner ET, Kamran SC, Haas JS (2021) The trajectory of racial/ethnic disparities in the use of cancer screening before and during the COVID-19 pandemic: a large US academic center analysis. Prev Med 151:106640. https://doi.org/10.1016/j.ypmed.2021.106640
Velazquez AI, Hayward JH, Gregory B, Dixit N (2021) trends in breast cancer screening in a safety-net hospital during the COVID-19 pandemic. JAMA Netw Open 4(8):e2119929. https://doi.org/10.1001/jamanetworkopen.2021.19929
Blair L, Warner ET, James P et al (2022) Exposure to natural vegetation in relation to mammographic density in a Massachusetts-based clinical cohort. Environ Epidemiol 6(4):e216. https://doi.org/10.1097/EE9.0000000000000216
Siu AL (2016) Screening for breast cancer: U.S. preventive services task force recommendation statement. Ann Intern Med. https://doi.org/10.7326/M15-2886
CDCBreastCancer. What are the risk factors for breast cancer? Centers for disease control and prevention. Published March 9, 2022. Accessed July 19, 2022. https://www.cdc.gov/cancer/breast/basic_info/risk_factors.htm
Smigal C, Jemal A, Ward E et al (2006) Trends in breast cancer by race and ethnicity: update 2006. CA Cancer J Clin 56(3):168–183. https://doi.org/10.3322/canjclin.56.3.168
Ulm K (1990) Simple method to calculate the confidence interval of a standardized mortality ratio (SMR). Am J Epidemiol 131(2):373–375. https://doi.org/10.1093/oxfordjournals.aje.a115507
Bernal JL, Cummins S, Gasparrini A (2017) Interrupted time series regression for the evaluation of public health interventions: a tutorial. Int J Epidemiol 46(1):348–355. https://doi.org/10.1093/ije/dyw098
Xiao H, Augusto O, Wagenaar BH (2021) Reflection on modern methods: a common error in the segmented regression parameterization of interrupted time-series analyses. Int J Epidemiol 50(3):1011–1015. https://doi.org/10.1093/ije/dyaa148
Linden A (2015) Conducting interrupted time-series analysis for single- and multiple-group comparisons. Stata J 15(2):480–500. https://doi.org/10.1177/1536867X1501500208
Andrews DWK (1991) Heteroskedasticity and autocorrelation consistent covariance matrix estimation. Econometrica 59(3):817–858. https://doi.org/10.2307/2938229
Zeileis A (2006) Object-oriented computation of sandwich estimators. J Stat Softw 16:1–16. https://doi.org/10.18637/jss.v016.i09
Surviellance, Epidemiology, and end results (SEER) program. Cancer of the breast (Female)—cancer stat facts. SEER. Accessed June 9, 2022. https://seer.cancer.gov/statfacts/html/breast.html
Li CI, Malone KE, Daling JR (2003) Differences in breast cancer stage, treatment, and survival by race and ethnicity. Arch Intern Med 163(1):49–56. https://doi.org/10.1001/archinte.163.1.49
Ooi SL, Martinez ME, Li CI (2011) Disparities in breast cancer characteristics and outcomes by race/ethnicity. Breast Cancer Res Treat 127(3):729–738. https://doi.org/10.1007/s10549-010-1191-6
Daly B, Olopade OI (2015) A perfect storm: how tumor biology, genomics, and health care delivery patterns collide to create a racial survival disparity in breast cancer and proposed interventions for change. CA Cancer J Clin 65(3):221–238. https://doi.org/10.3322/caac.21271
Sprague BL, Lowry KP, Miglioretti DL et al (2021) changes in mammography use by women’s characteristics during the first 5 months of the COVID-19 pandemic. JNCI J Natl Cancer Inst 113(9):1161–1167. https://doi.org/10.1093/jnci/djab045
Labaki C, Bakouny Z, Schmidt A et al (2021) Recovery of cancer screening tests and possible associated disparities after the first peak of the COVID-19 pandemic. Cancer Cell 39(8):1042–1044. https://doi.org/10.1016/j.ccell.2021.06.019
Miller-Kleinhenz JM, Collin LJ, Seidel R et al (2021) racial disparities in diagnostic delay among women with breast cancer. J Am Coll Radiol 18(10):1384–1393. https://doi.org/10.1016/j.jacr.2021.06.019
Funding
The project was supported by the Breast Cancer Research Foundation (RT). Researchers were supported by the University of Louisville CIEHS P30 ES030283 (NCD), K01CA188075 (ETW), T32CA09001 (NCD, MOS, MEB) P30 ES000002 (JH, FL), and NIH/NCI K00 CA212222 (MEB). This manuscript is the responsibility of the authors and does not represent the official views of the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Mollie E. Barnard reports personal fees from Epi Excellence LLC outside of the submitted work. All other authors have no relevant financial interests to disclose.
Ethical approval
The study was approved by the Mass General Brigham Human Research Committee, the Institutional Review Board (IRB) of Mass General Brigham. Participants provided written informed consent prior to joining the Boston Mammography Cohort Study.
Consent to participate
Written informed consent was obtained from all individual participants included in the study.
Consent to publication
The authors affirm that human research participants provided written informed consent for publication of their data published in a journal article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, N., Cheng, D., Sodipo, M.O. et al. Impact of age, race, and family history on COVID-19–related changes in breast cancer screening among the Boston mammography cohort study. Breast Cancer Res Treat 202, 335–343 (2023). https://doi.org/10.1007/s10549-023-07083-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-07083-y