Abstract
Purpose
High-risk breast pathology is a breast cancer risk factor for which timely treatment is crucial. Nurse navigation programs have been implemented to minimize delays in patient care. This study evaluated nurse navigation in terms of timeliness to surgery for patients with high-risk breast pathology.
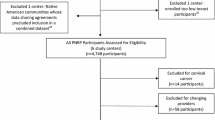
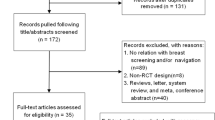
Methods
This was a single-institution, retrospective review of patients with identified high-risk breast pathology undergoing lumpectomy between January 2017 and June 2019. Patients were stratified into cohorts based on periods with and without nurse navigation. Preoperative and postoperative time to care as well as demographic and tumor characteristics were compared using univariate and multivariate analysis.
Results
100 patients had assigned nurse navigators and 29 patients did not. Nurse navigation was associated with reduced time from referral to date of surgery (DOS) by 16.9 days (p = 0.003). Patients > 75 years had a shorter time to first appointment (p = 0.03), and patients with Medicare insurance had a reduced time from referral to DOS (p = 0.005). 20% of all patients were upstaged to cancer on final surgical pathology.
Conclusion
Nurse navigation was significantly associated with decreased time to care for patients with high-risk breast pathology undergoing lumpectomy. We recommend nurse navigation programs as part of a comprehensive approach for patients with high-risk breast pathology.
Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Cancer Stat Facts: Female Breast Cancer (2019) http://seer.cancer.gov/statfacts/html/breast.html. Accessed July 26, 2022
Lopez-Garcia MA, Geyer FC, Lacroix-Triki M, Marchió C, Reis-Filho JS (2010) Breast cancer precursors revisited: molecular features and progression pathways. Histopathology 57(2):171–192. https://doi.org/10.1111/j.1365-2559.2010.03568.x
American Cancer Society. Breast Cancer Facts & Figs. 2019–2020 Atlanta: American Cancer Society, Inc.
Bleicher RJ, Ruth K, Sigurdson ER et al (2016) Time to surgery and breast Cancer survival in the United States. JAMA Oncol 2(3):330–339. https://doi.org/10.1001/jamaoncol.2015.4508
Molina Y, Kim SJ, Berrios N et al (2018) Patient Navigation improves subsequent breast Cancer Screening after a noncancerous result: evidence from the patient Navigation in Medically Underserved Areas Study. J Womens Health (Larchmt) 27(3):317–323. https://doi.org/10.1089/jwh.2016.6120
McKevitt EC, Dingee CK, Leung SP et al (2017) Reduced time to breast Cancer diagnosis with coordination of Radiological and Clinical Care. Cureus 9(12):e1919. https://doi.org/10.7759/cureus.1919
Garcia D, Siegel JB, Mahvi DA et al (2020) What is elective oncologic surgery in the time of COVID-19? A literature review of the Impact of Surgical Delays on Outcomes in patients with Cancer. Clin Oncol Res 3(6):1–11. https://doi.org/10.31487/j.COR.2020.06.05
Basu M, Linebarger J, Gabram SG, Patterson SG, Amin M, Ward KC (2013) The effect of nurse navigation on timeliness of breast cancer care at an academic comprehensive cancer center. Cancer 119(14):2524–2531. https://doi.org/10.1002/cncr.28024
Role of the Oncology Nurse Navigator throughout the Cancer Trajectory. Oncol Nurs Forum. 45(3):283. https://doi.org/10.1188/18.Onf.283
Case MA (2011) Oncology nurse navigator. Clin J Oncol Nurs 15(1):33–40. https://doi.org/10.1188/11.Cjon.33-40
Rosenberg K (2011) Patient navigators improve colorectal cancer screening rates. Am J Nurs 111(10):15. https://doi.org/10.1097/01.NAJ.0000406404.80894.5a
Enomoto LM, Fenstermaker J, Desnoyers RJ et al (2019) Oncology Navigation decreases time to treatment in patients with pancreatic malignancy. Ann Surg Oncol 26(5):1512–1518. https://doi.org/10.1245/s10434-019-07157-6
Luckett R, Pena N, Vitonis A, Bernstein MR, Feldman S (2015) Effect of patient navigator program on no-show rates at an academic referral colposcopy clinic. J Womens Health (Larchmt) 24(7):608–615. https://doi.org/10.1089/jwh.2014.5111
Bush ML, Kaufman MR, Shackleford T (2018) Adherence in the Cancer Care setting: a systematic review of Patient Navigation to Traverse Barriers. J Cancer Educ 33(6):1222–1229. https://doi.org/10.1007/s13187-017-1235-2
Baik SH, Gallo LC, Wells KJ (2016) Patient Navigation in breast Cancer Treatment and Survivorship: a systematic review. J Clin Oncol 34(30):3686–3696. https://doi.org/10.1200/jco.2016.67.5454
McKevitt E, Dingee C, Warburton R et al (2018) Patient navigation reduces time to care for patients with breast symptoms and abnormal screening mammograms. Am J Surg 215(5):805–811. https://doi.org/10.1016/j.amjsurg.2017.12.016
Cantril C, Moore E, Yan X (2019) Diagnosis Disclosure: patient preferences and the role of the breast nurse Navigator. Clin J Oncol Nurs 23(6):619–626. https://doi.org/10.1188/19.Cjon.619-626
Motulsky H Intuitive Biostatistics: A Nonmathematical Guide to Statistical Thinking 4th ed. Published 4th
Cen C, Chun J, Schnabel F (2020) Management of women at increased risk for breast cancer secondary to high-risk proliferative lesions and family history of the disease. Breast J 26(8):1543–1548. https://doi.org/10.1111/tbj.13964
Chen F, Mercado C, Yermilov I et al (2010) Improving breast cancer quality of care with the use of patient navigators. Am Surg 76(10):1043–1046 Published 2010/11/26
Ali-Faisal SF, Colella TJ, Medina-Jaudes N, Benz Scott L (2017) The effectiveness of patient navigation to improve healthcare utilization outcomes: a meta-analysis of randomized controlled trials. Patient Educ Couns 100(3):436–448. https://doi.org/10.1016/j.pec.2016.10.014
Chiarelli AM, Muradali D, Blackmore KM et al (2017) Evaluating wait times from screening to breast cancer diagnosis among women undergoing organised assessment vs usual care. Br J Cancer 116(10):1254–1263. https://doi.org/10.1038/bjc.2017.87
Ward WH, DeMora L, Handorf E et al (2020) Preoperative delays in the treatment of DCIS and the Associated incidence of invasive breast Cancer. Ann Surg Oncol 27(2):386–396. https://doi.org/10.1245/s10434-019-07844-4
Lewis JT, Hartmann LC, Vierkant RA et al (2006) An analysis of breast cancer risk in women with single, multiple, and atypical papilloma. Am J Surg Pathol 30(6):665–672. https://doi.org/10.1097/00000478-200606000-00001
Jacobs TW, Byrne C, Colditz G, Connolly JL, Schnitt SJ (1999) Radial scars in benign breast-biopsy specimens and the risk of breast cancer. N Engl J Med 340(6):430–436. https://doi.org/10.1056/nejm199902113400604
Said SM, Visscher DW, Nassar A et al (2015) Flat epithelial atypia and risk of breast cancer: a Mayo cohort study. Cancer 121(10):1548–1555. https://doi.org/10.1002/cncr.29243
Kraft E, Limberg JN, Dodelzon K et al (2021) Radial scars and complex sclerosing lesions of the breast: prevalence of malignancy and natural history under active surveillance. Ann Surg Oncol 28(9):5149–5155. https://doi.org/10.1245/s10434-021-09713-5
Limberg J, Kucher W, Fasano G, Hoda S, Michaels A, Marti JL (2021) Intraductal papilloma of the breast: prevalence of malignancy and natural history under active surveillance. Ann Surg Oncol 28(11):6032–6040. https://doi.org/10.1245/s10434-021-09870-7
Degnim AC, King TA (2013) Surgical management of high-risk breast lesions. Surg Clin North Am 93(2):329–340. https://doi.org/10.1016/j.suc.2012.12.005
Dudley DJ, Drake J, Quinlan J et al (2012) Beneficial effects of a combined navigator/promotora approach for hispanic women diagnosed with breast abnormalities. Cancer Epidemiol Biomarkers Prev 21(10):1639–1644. https://doi.org/10.1158/1055-9965.Epi-12-0538
Stahl KA, Dodge D, Olecki EJ et al (2022) Insurance Status and Travel Distance to single treatment facility Predictive of Mastectomy. J Surg Res 270:22–30. https://doi.org/10.1016/j.jss.2021.08.035
Sprague BL, Ahern TP, Herschorn SD, Sowden M, Weaver DL, Wood ME (2021) Identifying key barriers to effective breast cancer control in rural settings. Prev Med 152(Pt 2):106741. https://doi.org/10.1016/j.ypmed.2021.106741
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Catherine Chung MD, Catherine Barker, Rupak Mukherjee PhD, Julie Siegel MD, and Andrea Abbott MD. The first draft of the manuscript was written by Catherine Chung and Catherine Barker and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no relevant conflicts of interest to disclose.
Ethical approval
This is an observational study. The IRB of the Medical University of South Carolina has confirmed that no ethical approval is required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Barker, C.S., Chung, C.W., Mukherjee, R. et al. The impact of nurse navigation on timeliness to treatment for benign high-risk breast pathology. Breast Cancer Res Treat 202, 129–137 (2023). https://doi.org/10.1007/s10549-023-07049-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-07049-0