Abstract
Purpose
Studies comparing the effect of aromatase inhibitor (AI) and tamoxifen use on cardiovascular disease (CVD) risk factors in hormone receptor-positive breast cancer (BC) survivors report conflicting results. We examined associations of endocrine therapy use with incident diabetes, dyslipidemia, and hypertension.
Methods
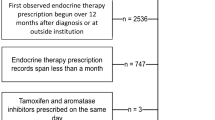
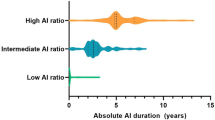
The Pathways Heart Study examines cancer treatment exposures with CVD-related outcomes in Kaiser Permanente Northern California members with BC. Electronic health records provided sociodemographic and health characteristics, BC treatment, and CVD risk factor data. Hazard ratios (HR) and 95% confidence intervals (CI) of incident diabetes, dyslipidemia, and hypertension in hormone receptor-positive BC survivors using AIs or tamoxifen compared with survivors not using endocrine therapy were estimated using Cox proportional hazards regression models adjusted for known confounders.
Results
In 8985 BC survivors, mean baseline age and follow-up time was 63.3 and 7.8 years, respectively; 83.6% were postmenopausal. By treatment, 77.0% used AIs, 19.6% used tamoxifen, and 16.0% used neither. Postmenopausal women who used tamoxifen had an increased rate (HR 1.43, 95% CI 1.06–1.92) of developing hypertension relative to those who did not use endocrine therapy. Tamoxifen use was not associated with incident diabetes, dyslipidemia, or hypertension in premenopausal BC survivors. Postmenopausal AI users had higher hazard rates of developing diabetes (HR 1.37, 95% CI 1.05–1.80), dyslipidemia (HR 1.58, 95% CI 1.29–1.92), and hypertension (HR 1.50, 95% CI 1.24–1.82) compared with non-endocrine therapy users.
Conclusion
Hormone receptor-positive BC survivors treated with AIs may have higher rates of developing diabetes, dyslipidemia, and hypertension over an average 7.8 years post-diagnosis.
Similar content being viewed by others
Data availability
These data are not publicly available because they contain potentially identifiable information but may be available from Kaiser Permanente Northern California contingent on appropriate human subjects’ approval and necessary data use agreements.
Abbreviations
- AJCC:
-
American Joint Committee on Cancer
- AI:
-
Aromatase inhibitor
- BC:
-
Breast cancer
- BMI:
-
Body mass index
- CVD:
-
Cardiovascular disease
- CI:
-
Confidence interval
- EHR:
-
Electronic health record
- GED:
-
General education degree
- HR:
-
Hazard rate ratio
- ICD:
-
International Classification of Disease
- KPNC:
-
Kaiser Permanente Northern California
- SD:
-
Standard deviation
References
American Cancer Society (2019) Breast cancer facts & figures 2019–2020. In: American Cancer Society. American Cancer Society, Inc, Atlanta
Cheung YM, Ramchand SK, Yeo B, Grossmann M (2019) Cardiometabolic effects of endocrine treatment of estrogen receptor-positive early breast cancer. J Endocr Soc 3(7):1283–1301
Matthews A, Stanway S, Farmer RE, Strongman H, Thomas S, Lyon AR, Smeeth L, Bhaskaran K (2018) Long term adjuvant endocrine therapy and risk of cardiovascular disease in female breast cancer survivors: systematic review. BMJ 363:k3845
Okwuosa TM, Morgans A, Rhee JW, Reding KW, Maliski S, Plana JC, Volgman AS, Moseley KF, Porter CB, Ismail-Khan R et al (2021) Impact of hormonal therapies for treatment of hormone-dependent cancers (breast and prostate) on the cardiovascular system: effects and modifications: a scientific statement from the American Heart Association. Circ Genom Precis Med 14(3):e000082
Early Breast Cancer Trialists' Collaborative G (2015) Aromatase inhibitors versus tamoxifen in early breast cancer: patient-level meta-analysis of the randomised trials. The Lancet 386(10001):1341–1352
Sund M, Garcia-Argibay M, Garmo H, Ahlgren J, Wennstig AK, Fredriksson I, Lindman H, Valachis A (2021) Aromatase inhibitors use and risk for cardiovascular disease in breast cancer patients: a population-based cohort study. Breast 59:157–164
Mehta LS, Watson KE, Barac A, Beckie TM, Bittner V, Cruz-Flores S, Dent S, Kondapalli L, Ky B, Okwuosa T et al (2018) Cardiovascular disease and breast cancer: where these entities intersect: a Scientific Statement From the American Heart Association. Circulation 137(8):e30–e66
Abdel-Qadir H, Amir E, Fischer HD, Fu L, Austin PC, Harvey PJ, Rochon PA, Lee DS, Anderson GM (2016) The risk of myocardial infarction with aromatase inhibitors relative to tamoxifen in post-menopausal women with early stage breast cancer. Eur J Cancer 68:11–21
Choi SH, Kim KE, Park Y, Ju YW, Jung JG, Lee ES, Lee HB, Han W, Noh DY, Yoon HJ et al (2020) Effects of tamoxifen and aromatase inhibitors on the risk of acute coronary syndrome in elderly breast cancer patients: an analysis of nationwide data. Breast 54:25–30
Haque R, Shi J, Schottinger JE, Chung J, Avila C, Amundsen B, Xu X, Barac A, Chlebowski RT (2016) Cardiovascular disease after aromatase inhibitor use. JAMA Oncol 2(12):1590–1597
Kamaraju S, Shi Y, Smith E, Nattinger AB, Laud P, Neuner J (2019) Are aromatase inhibitors associated with higher myocardial infarction risk in breast cancer patients? A Medicare population-based study. Clin Cardiol 42(1):93–100
Khosrow-Khavar F, Filion KB, Bouganim N, Suissa S, Azoulay L (2020) Aromatase inhibitors and the risk of cardiovascular outcomes in women with breast cancer: a population-based cohort study. Circulation 141(7):549–559
Matthews AA, Peacock Hinton S, Stanway S, Lyon AR, Smeeth L, Lund JL, Bhaskaran K (2021) Endocrine therapy use and cardiovascular risk in postmenopausal breast cancer survivors. Heart 107(16):1327–1335
Pineda-Moncusi M, Garcia-Giralt N, Diez-Perez A, Tusquets I, Servitja S, Albanell J, Prieto-Alhambra D, Nogues X (2020) Thromboembolic, cardiovascular and overall mortality risks of aromatase inhibitors, compared with tamoxifen treatment: an outpatient-register-based retrospective cohort study. Ther Adv Med Oncol 12:1758835920909660
Xu X, Chlebowski RT, Shi J, Barac A, Haque R (2019) Aromatase inhibitor and tamoxifen use and the risk of venous thromboembolism in breast cancer survivors. Breast Cancer Res Treat 174(3):785–794
He Y, Zhang J, Shen G, Liu L, Zhao Q, Lu X, Yang H, Hong D (2019) Aromatase inhibitors and risk of cardiovascular events in breast cancer patients: a systematic review and meta-analysis. BMC Pharmacol Toxicol 20(1):62
Khosrow-Khavar F, Filion KB, Al-Qurashi S, Torabi N, Bouganim N, Suissa S, Azoulay L (2017) Cardiotoxicity of aromatase inhibitors and tamoxifen in postmenopausal women with breast cancer: a systematic review and meta-analysis of randomized controlled trials. Ann Oncol 28(3):487–496
Rosano GM, Chierchia SL, Leonardo F, Beale CM, Collins P (1996) Cardioprotective effects of ovarian hormones. Eur Heart J 17:15–19
Lewis S (2007) Do endocrine treatments for breast cancer have a negative impact on lipid profiles and cardiovascular risk in postmenopausal women? Am Heart J 153(2):182–188
Kato I, Toniolo P, Akhmedkhanov A, Koenig KL, Shore R, Zeleniuch-Jacquotte A (1998) Prospective study of factors influencing the onset of natural menopause. J Clin Epidemiol 51(12):1271–1276
Weir CB, Jan A (2022) BMI classification percentile and cut off points. In: StatPearls. Treasure Island
Kwan ML, Cheng RK, Iribarren C, Neugebauer R, Rana JS, Nguyen-Huynh M, Shi Z, Laurent CA, Lee VS, Roh JM et al (2022) Risk of cardiometabolic risk factors in women with and without a history of breast cancer: the pathways heart study. J Clin Oncol 40(15):1635–1646
Karter AJ, Schillinger D, Adams AS, Moffet HH, Liu J, Adler NE, Kanaya AM (2013) Elevated rates of diabetes in Pacific Islanders and Asian subgroups: the Diabetes Study of Northern California (DISTANCE). Diabetes Care 36(3):574–579
Jaffe MG, Lee GA, Young JD, Sidney S, Go AS (2013) Improved blood pressure control associated with a large-scale hypertension program. JAMA 310(7):699–705
Kim JE, Choi J, Park J, Han W, Kang D, Choi JY (2022) Effects of endocrine therapy on cardiovascular diseases and type 2 diabetes among breast cancer survivors: the National Health Insurance Service Database of Korea. J Am Heart Assoc 11(20):e026743
Sun LM, Chen HJ, Liang JA, Li TC, Kao CH (2014) Association of tamoxifen use and increased diabetes among Asian women diagnosed with breast cancer. Br J Cancer 111(9):1836–1842
Ye F, Wen J, Yang A, Wang Y, Li N, Yu P, Wei W, Tang J (2022) The influence of hormone therapy on secondary diabetes mellitus in breast cancer: a meta-analysis. Clin Breast Cancer 22(1):e48–e58
Choi YJ, Bak K, Yeo Y, Choi Y, Shin S (2021) Incident type 2 diabetes risk of selective estrogen receptor modulators in female patients with breast cancer. Pharmaceuticals 14(9):925
Gupta T, Purington N, Liu M, Han S, Sledge G, Schapira L, Kurian AW (2022) Incident comorbidities after tamoxifen or aromatase inhibitor therapy in a racially and ethnically diverse cohort of women with breast cancer. Breast Cancer Res Treat 196(1):175–183
Santorelli ML, Hirshfield KM, Steinberg MB, Rhoads GG, Lin Y, Demissie K (2016) Hormonal therapy for breast cancer and diabetes incidence among postmenopausal women. Ann Epidemiol 26(6):436–440
Dewar JA, Horobin JM, Preece PE, Tavendale R, Tunstall-Pedoe H, Wood RA (1992) Long term effects of tamoxifen on blood lipid values in breast cancer. BMJ 305(6847):225–226
Grey AB, Stapleton JP, Evans MC, Reid IR (1995) The effect of the anti-estrogen tamoxifen on cardiovascular risk factors in normal postmenopausal women. J Clin Endocrinol Metab 80(11):3191–3195
Gupta S, Tandon VR, Kapoor B, Gupta A, Gupta GD, Khajuria V (2006) Effects of tamoxifen therapy on plasma lipid profile in patients of breast cancer. J Assoc Physicians India 54:183–186
He T, Li X, Li J, Wang Z, Fan Y, Li X, Fu Z, Wu Y, Lv Q, Luo T et al (2021) Lipid changes during endocrine therapy in breast cancer patients: the results of a 5-year real-world retrospective analysis. Front Oncol 11:670897
Hozumi Y, Suemasu K, Takei H, Aihara T, Takehara M, Saito T, Ohsumi S, Masuda N, Ohashi Y (2011) The effect of exemestane, anastrozole, and tamoxifen on lipid profiles in Japanese postmenopausal early breast cancer patients: final results of National Surgical Adjuvant Study BC 04, the TEAM Japan sub-study. Ann Oncol 22(8):1777–1782
Ilanchezhian S, Thangaraju M, Sachdanandam P (1995) Plasma lipids and lipoprotein alterations in tamoxifen-treated breast cancer women in relation to the menopausal status. Cancer Biochem Biophys 15(2):83–90
Love RR, Wiebe DA, Feyzi JM, Newcomb PA, Chappell RJ (1994) Effects of tamoxifen on cardiovascular risk factors in postmenopausal women after 5 years of treatment. J Natl Cancer Inst 86(20):1534–1539
Love RR, Wiebe DA, Newcomb PA, Cameron L, Leventhal H, Jordan VC, Feyzi J, DeMets DL (1991) Effects of tamoxifen on cardiovascular risk factors in postmenopausal women. Ann Intern Med 115(11):860–864
Tominaga T, Kimijima I, Kimura M, Takatsuka Y, Takashima S, Nomura Y, Kasumi F, Yamaguchi A, Masuda N, Noguchi S et al (2010) Effects of toremifene and tamoxifen on lipid profiles in post-menopausal patients with early breast cancer: interim results from a Japanese phase III trial. Jpn J Clin Oncol 40(7):627–633
Wang J, Yin J, Qiu J, Jiang J, Hu Y, Zhu K, Zheng H, Luo T, Zhong X (2022) Comparison of dyslipidemia incidence in Chinese early-stage breast cancer patients following different endocrine therapies: a population-based cohort study. Front Endocrinol 13:815960
Wang K, Shen L, Tian W, Zhang S (2022) Comparison of changes in lipid profiles of premenopausal women with early-stage breast cancer treated with different endocrine therapies. Sci Rep 12(1):22650
Wasan KM, Ramaswamy M, Haley J, Dunn BP (1997) Administration of long-term tamoxifen therapy modifies the plasma lipoprotein-lipid concentration and lipid transfer protein I activity in postmenopausal women with breast cancer. J Pharm Sci 86(7):876–879
Boszkiewicz K, Piwowar A, Petryszyn P (2022) Aromatase inhibitors and risk of metabolic and cardiovascular adverse effects in breast cancer patients-a systematic review and meta-analysis. J Clin Med 11(11):3133
Monnier A (2006) Effects of adjuvant aromatase inhibitor therapy on lipid profiles. Expert Rev Anticancer Ther 6(11):1653–1662
Blaes A, Beckwith H, Florea N, Hebbel R, Solovey A, Potter D, Yee D, Vogel R, Luepker R, Duprez D (2017) Vascular function in breast cancer survivors on aromatase inhibitors: a pilot study. Breast Cancer Res Treat 166(2):541–547
Stergiou GS, Zourbaki AS, Efstathiou SP, Stathopoulos GP, Keramopoulos AD, Mountokalakis TD (2002) Effect of estrogen receptor modulator tamoxifen on blood pressure, plasma renin activity, and renal sodium excretion. Am J Hypertens 15(8):739–742
Acknowledgements
We thank all the women who provided data for these analyses. We thank the National Institutes of Health National Cancer Institute for providing funding (R01CA214057).
Funding
The Pathways Heart Study is supported by the National Cancer Institute, Bethesda, MD 20814 (R01 CA214057, U01 CA195565).
Author information
Authors and Affiliations
Contributions
ER-S, MLK, and HG conceived and designed this study. Data collection and assembly was completed by MLK, ZS, CAL, VSL, JMR, YH, HS, and HG. Data analysis was completed by ER-S, CAL, YH, and HS. The findings were interpreted by ER-S, MLK, CI, RC, RN, JSR, MN-H, DLH, LHK, and HG. The first draft of the manuscript was written by ER-S and all authors commented on previous versions. All authors read and approved the final, submitted manuscript.
Corresponding author
Ethics declarations
Competing interests
All authors have no financial or non-financial interests to declare.
Ethical approval
The Human Subjects Institutional Review Board of Kaiser Permanente Northern California has approved this study.
Consent to participate
This was a data-only study that used existing protected health information from the electronic health records of Kaiser Permanente Northern California and is therefore, regulated by the HIPAA Privacy Rule.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Previous presentations: 2021 San Antonio Breast Cancer Symposium, Virtual Poster Presentation (Heather Greenlee).
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rillamas-Sun, E., Kwan, M.L., Iribarren, C. et al. Development of cardiometabolic risk factors following endocrine therapy in women with breast cancer. Breast Cancer Res Treat 201, 117–126 (2023). https://doi.org/10.1007/s10549-023-06997-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-06997-x