Abstract
Purpose
Immediate lymphatic reconstruction (ILR) is a procedure known to reduce the risk of lymphedema in patients undergoing axillary lymph node dissection (ALND). However, patients who receive adjuvant radiotherapy are at increased risk of lymphedema. The aim of this study was to quantify the extent of radiation at the site of surgical prevention.
Methods
We recently began deploying clips at the site of ILR to identify the site during radiation planning. A retrospective review was performed to identify breast cancer patients who underwent ILR with clip deployment and adjuvant radiation therapy from October 2020 to April 2022. Patients were excluded if they had not completed radiotherapy. The exposure and dose of radiation received by the site was determined and recorded.
Results
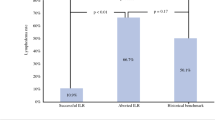
In a cohort of 11 patients, the site fell within the radiation field in 7 patients (64%) and received a median dose of 4280 cGy. Among these 7 patients, 3 had sites located within tissue considered at risk of oncologic recurrence and the remaining 4 sites received radiation from a tangential field treating the breast or chest wall. The median dose to the ILR site for the 4 patients whose sites were outside the radiation fields was 233 cGy.
Conclusion
Our findings suggest that even when the site of surgical prevention was not within the targeted radiation field during treatment planning, it remains susceptible to radiation. Strategies for limiting radiation at this site are needed.



Similar content being viewed by others
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available due containment of protected health information but are available from the corresponding author on reasonable request.
References
Johnson AR, Fleishman A, Granoff MD et al Evaluating the impact of Immediate Lymphatic Reconstruction for the Surgical Prevention of Lymphedema. Plast Reconstr Surg Published online 2021:373E-381E. doi:https://doi.org/10.1097/PRS.0000000000007636
Johnson AR, Kimball S, Epstein S et al (2019) Lymphedema Incidence after Axillary Lymph Node Dissection: quantifying the impact of Radiation and the lymphatic Microsurgical Preventive Healing Approach. Ann Plast Surg 82(4S Suppl 3):S234–S241. https://doi.org/10.1097/SAP.0000000000001864
Warren LEG, Miller CL, Horick N et al (2014) The impact of radiation therapy on the risk of lymphedema after treatment for breast cancer: a prospective cohort study. Int J Radiat Oncol Biol Phys 88(3):565–571. https://doi.org/10.1016/j.ijrobp.2013.11.232
Miller CL, Specht MC, Skolny MN et al (2014) Risk of lymphedema after mastectomy: potential benefit of applying ACOSOG Z0011 protocol to mastectomy patients. Breast Cancer Res Treat 144(1):71–77. https://doi.org/10.1007/s10549-014-2856-3
Coen JJ, Taghian AG, Kachnic LA, Assaad SI, Powell SN (2003) Risk of lymphedema after regional nodal irradiation with breast conservation therapy. Int J Radiat Oncol Biol Phys 55(5):1209–1215. https://doi.org/10.1016/s0360-3016(02)04273-6
Wernicke AG, Goodman RL, Turner BC et al (2011) A 10-year follow-up of treatment outcomes in patients with early stage breast cancer and clinically negative axillary nodes treated with tangential breast irradiation following sentinel lymph node dissection or axillary clearance. Breast Cancer Res Treat 125(3):893–902. https://doi.org/10.1007/s10549-010-1167-6
Ahmed RL, Schmitz KH, Prizment AE, Folsom AR (2011) Risk factors for lymphedema in breast cancer survivors, the Iowa Women’s Health Study. Breast Cancer Res Treat 130(3):981–991. https://doi.org/10.1007/s10549-011-1667-z
Shaitelman SF, Chiang YJ, Griffin KD et al (2017) Radiation therapy targets and the risk of breast cancer-related lymphedema: a systematic review and network meta-analysis. Breast Cancer Res Treat 162(2):201–215. https://doi.org/10.1007/s10549-016-4089-0
Allam O, Park KE, Chandler L et al (2020) The impact of radiation on lymphedema: a review of the literature. Gland Surg 9(2):596–602. https://doi.org/10.21037/gs.2020.03.20
Gross JP, Sachdev S, Helenowski IB et al (2018) Radiation Therapy Field Design and Lymphedema Risk after Regional nodal irradiation for breast Cancer. Int J Radiat Oncol Biol Phys 102(1):71–78. https://doi.org/10.1016/j.ijrobp.2018.03.046
The American Society of Breast Surgeons (2022) Consensus Guideline on Axillary Management for Patients With In-Situ and Invasive Breast Cancer: A Concise Overview Purpose.;
Spiguel L, Shaw C, Katz A et al (2017) Fluorescein isothiocyanate: a novel application for lymphatic surgery. Annals of plastic surgery, vol 78. Lippincott Williams and Wilkins, pp S296–S298. doi:https://doi.org/10.1097/SAP.0000000000001034
Friedman R, Bustos VP, Postian T et al (2022) Utilizing a lower extremity vein graft for immediate lymphatic reconstruction. J Plast Reconstr Aesthetic Surg 75(8):2851–2854. https://doi.org/10.1097/GOX.0000000000003296
Granoff MD, Pardo J, Shillue K et al Variable Anatomy of the Lateral Upper Arm Lymphatic Channel: A Potential Anatomic Risk Factor for the Development of Breast Cancer Related Lymphedema. Plast Reconstr Surg. 2023 Jan 24. doi: https://doi.org/10.1097/PRS.0000000000010245. Epub ahead of print. PMID: 36727729
Granoff M, Pardo J, Johnson AR et al (2022) The superficial and functional lymphatic anatomy of the Upper Extremity. Plast Reconstr Surg Published online August 4. https://doi.org/10.1097/PRS.0000000000009555
Acknowledgements and Funding Information
Research reported in this publication was supported in part by the National Heart, Lung, and Blood Institute of the National Institutes of Health under award number R01HL157991 (D.S.), the National Institutes of Health Common Fund under award number U54HL165440 (D.S.), and the 2022 JOBST Lymphatic Research Grant awarded by the Boston Lymphatic Symposium, Inc. (received by author R.F.).
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Rosie Friedman, JacqueLyn Kinney, Daphna Spiegel, Julia Willcox, Abraham Recht, and Dhruv Singhal. The first draft of the manuscript was written by Rosie Friedman and Daphna Spiegel, and all authors commented on previous versions of the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing Interests
The authors have no relevant financial or other non-financial interests to disclose.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Beth Israel Deaconess Medical Center Institutional Review Board, Protocol #2022P000234.
Consent to participate
Secondary data were utilized for this study and therefore participant consent was not required.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Friedman, R., Spiegel, D.Y., Kinney, J. et al. Quantifying radiation in the axillary bed at the site of lymphedema surgical prevention. Breast Cancer Res Treat 201, 299–305 (2023). https://doi.org/10.1007/s10549-023-06988-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-023-06988-y