Abstract
Background
Breast cancer is the most common cancer among women, but most cancer registries do not capture recurrences. We estimated the incidence of local, regional, and distant recurrences using administrative data.
Methods
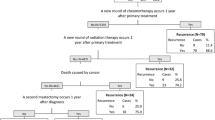
Patients diagnosed with stage I-III primary breast cancer in Ontario, Canada from 2013 to 2017 were included. Patients were followed until 31/Dec/2021, death, or a new primary cancer diagnosis. We used hospital administrative data (diagnostic and intervention codes) to identify local recurrence, regional recurrence, and distant metastasis after primary diagnosis. We used logistic regression to explore factors associated with developing a distant metastasis.
Results
With a median follow-up 67 months, 5,431/45,857 (11.8%) of patients developed a distant metastasis a median 23 (9, 42) months after diagnosis of the primary tumor. 1086 (2.4%) and 1069 (2.3%) patients developed an isolated regional or a local recurrence, respectively. Patients with distant metastatic disease had a median overall survival of 15.4 months (95% CI 14.4–16.4 months) from the time recurrence/metastasis was identified. In contrast, the median survival for all other patients was not reached. Patients were more likely to develop a distant metastasis if they had more advanced stage, greater comorbidity, and presented with symptoms (p < 0.0001). Trastuzumab halved the risk of recurrence [OR 0.53 (0.45–0.63), p < 0.0001].
Conclusion
Distant metastasis is not a rare outcome for patients diagnosed with breast cancer, translating to an annual incidence of 2132 new cases (17.8% of all breast cancer diagnoses). Overall survival remains high for patients with locoregional recurrences, but was poor following a diagnosis of a distant metastasis.






Similar content being viewed by others
Data availability
Ontario Health is prohibited from making the data used in this research publicly accessible if it includes potentially identifiable personal health information and/or personal information as defined in Ontario law, specifically the Personal Health Information Protection Act (PHIPA) and the Freedom of Information and Protection of Privacy Act (FIPPA). Upon request, data de-identified to a level suitable for public release may be provided.
References
Warren J, Yabroff K (2015) Challenges and opportunities in measuring cancer recurrence in the United States: PubMed: NCBI. J Natl Cancer Inst 107:8
Vuksanovic D, Sanmugarajah J, Lunn D, Sawhney R, Eu K, Liang R (2021) Unmet needs in breast cancer survivors are common, and multidisciplinary care is underutilised: the Survivorship Needs Assessment Project. Breast Cancer 28(2):289–297
Koch L, Bertram H, Eberle A et al (2014) Fear of recurrence in long-term breast cancer survivors: still an issue. Results on prevalence, determinants, and the association with quality of life and depression from the cancer survivorship: a multi-regional population-based study. Psychooncology 23(5):547–554
Mariotto AB, Etzioni R, Hurlbert M, Penberthy L, Mayer M (2017) Estimation of the number of women living with metastatic breast cancer in the United States. Cancer Epidemiol Biomarkers Prev 26(6):809–815
Muradali D, Kennedy EB, Eisen A, Holloway CMB, Smith CR, Chiarelli AM (2017) Breast screening for survivors of breast cancer: a systematic review. Prev Med (Baltim) 103:70–75
Darby S, McGale P, Correa C et al (2011) Effect of radiotherapy after breast-conserving surgery on 10-year recurrence and 15-year breast cancer death: meta-analysis of individual patient data for 10 801 women in 17 randomised trials. Lancet 378(9804):1707–1716
Dong Y, Zhang WW, Wang J, Sun JY, He ZY, Wu SG (2019) The 21-gene recurrence score and effects of adjuvant radiotherapy after breast conserving surgery in early-stage breast cancer. Futur Oncol 15(14):1629–1639
Bradley R, Burrett J, Clarke M et al (2015) Aromatase inhibitors versus tamoxifen in early breast cancer: patient-level meta-analysis of the randomised trials. Lancet 386(10001):1341–1352
Dent R, Trudeau M, Pritchard KI et al (2007) Triple-negative breast cancer: clinical features and patterns of recurrence. Clin Cancer Res 13(15):4429–4434
Siotos C, Naska A, Bello RJ et al (2019) Survival and disease recurrence rates among breast cancer patients following mastectomy with or without breast reconstruction. Plast Reconstr Surg 144(2):169e–177e
Voogd AC, Nielsen M, Peterse JL et al (2001) Differences in risk factors for local and distant recurrence after breast-conserving therapy or mastectomy for stage I and II breast cancer: pooled results of two large European randomized trials. J Clin Oncol 19(6):1688–1697
Chubak J, Yu O, Pocobelli G et al (2012) Administrative data algorithms to identify second breast cancer events following early-stage invasive breast cancer. J Natl Cancer Inst 104(12):931–940
Xu Y, Kong S, Cheung WY et al (2019) Development and validation of case-finding algorithms for recurrence of breast cancer using routinely collected administrative data. BMC Cancer 19:1
Ritzwoller DP, Hassett MJ, Uno H et al (2018) Development, validation, and dissemination of a breast cancer recurrence detection and timing informatics algorithm. J Natl Cancer Inst 110(3):273–281
Mariotto AB, Zou Z, Zhang F, Howlader N, Kurian AW, Etzioni R (2018) Can we use survival data from cancer registries to learn about disease recurrence? The case of breast cancer. Cancer Epidemiol Biomarkers Prev 27(11):1332–1341
Haque R, Shi J, Schottinger JE et al (2015) A hybrid approach to identify subsequent breast cancer using pathology and automated health information data. Med Care 53(4):380–385
Habbous S, Homenauth E, Barisic A et al (2022) Differences in breast cancer diagnosis by patient presentation in Ontario: a retrospective cohort study. C Open 10(2):E313–E330
Padmanabhan N, Subramanyan A, Radhakrishna S (2015) Synchronous bilateral breast cancers. J Clin Diagnostic Res 9(9):10–13
Botteri E, Bagnardi V, Rotmensz N et al (2009) Analysis of local regional recurrences in breast cancer after conservative surgery. Ann Oncol 21(4):723–728
Luo C, Zhong X, Deng L, Xie Y, Hu K, Zheng H (2019) Nomogram predicting locoregional recurrence to assist decision-making of postmastectomy radiation therapy in patients with T1–2N1 breast cancer. Int J Radiat Oncol Biol Phys 103(4):905–912
Tovar JR, Zandonade E, Amorim MHC (2014) Factors associated with the incidence of local recurrences of breast cancer in women who underwent conservative surgery. Int J Breast Cancer 2014:639534
Spronk I, Schellevis FG, Burgers JS, de Bock GH, Korevaar JC (2018) Incidence of isolated local breast cancer recurrence and contralateral breast cancer: a systematic review. Breast 39:70–79
Geurts YM, Witteveen A, Bretveld R et al (2017) Patterns and predictors of first and subsequent recurrence in women with early breast cancer. Breast Cancer Res Treat 165(3):709–720
Hassett MJ, Ritzwoller DP, Taback N et al (2014) Validating billing/encounter codes as indicators of lung, colorectal, breast, and prostate cancer recurrence using two large contemporary cohorts. Med Care 52(10):e65–e73
Warren JL, Mariotto A, Melbert D et al (2016) Sensitivity of Medicare claims to identify cancer recurrence in elderly colorectal and breast cancer patients. Med Care 54(8):e47–e54
Wapnir IL, Khan A (2019) Current strategies for the management of locoregional breast cancer recurrence. Oncol (United States) 33(1):19–25
Rasmussen LA, Jensen H, Virgilsen LF, Thorsen LBJ, Offersen BV, Vedsted P (2019) A validated algorithm for register-based identification of patients with recurrence of breast cancer—based on danish breast cancer group (DBCG) data. Cancer Epidemiol 59:129–134
Holloway CMB, Shabestari O, Eberg M et al (2022) Identifying breast cancer recurrence in administrative data: algorithm development and validation. Curr Oncol 29(8):5338–5367
Kroenke CH, Chubak J, Johnson L, Castillo A, Weltzien E, Caan BJ (2016) Enhancing breast cancer recurrence algorithms through selective use of medical record data. JNCI J Natl Cancer Inst 108(3):336
Habbous S, Forster K, Darling G et al (2020) Incidence and real-world burden of brain metastases from solid tumors and hematologic malignancies in Ontario: a population-based study. Neuro-oncology Adv 3:1
Ontario Cancer Statistics 2020. 2020. https://www.cancercareontario.ca/en/statistical-reports/ontario-cancer-statistics-2020/ch-1-estimated-current-cancer-incidence. Accessed November 11, 2020
Pagani O, Senkus E, Wood W et al (2010) International guidelines for management of metastatic breast cancer: can metastatic breast cancer be cured? JNCI J Natl Cancer Inst 102(7):456
Coleman M, Forman D, Bryant H et al (2011) Cancer survival in Australia, Canada, Denmark, Norway, Sweden, and the UK, 1995–2007 (the International Cancer Benchmarking Partnership): an analysis of population-based cancer registry data. Lancet 377(9760):127–138
Miksad RA, Zietemann V, Gothe R et al (2008) Progression-free survival as a surrogate endpoint in advanced breast cancer. Int J Technol Assess Health Care 24(4):371–383
Kemp R, Prasad V (2017) Surrogate endpoints in oncology: When are they acceptable for regulatory and clinical decisions, and are they currently overused? BMC Med 15:1
Hernandez-Villafuerte K, Fischer A, Latimer N (2018) Challenges and methodologies in using progression free survival as a surrogate for overall survival in oncology. Int J Technol Assess Health Care 34(3):300–316
Seely JM, Alhassan T (2018) Screening for breast cancer in 2018—what should we be doing today? Curr Oncol 25(Suppl 1):S115–S124
Jones T, Duquette D, Underhill M et al (2018) Surveillance for cancer recurrence in long-term young breast cancer survivors randomly selected from a statewide cancer registry. Breast Cancer Res Treat 169(1):141–152
Zeng Z, Espino S, Roy A et al (2018) Using natural language processing and machine learning to identify breast cancer local recurrence. BMC Bioinformatics 19(Suppl 17):498
Acknowledgements
Parts of this material are based on data and information compiled and provided by the Canadian Institute of Health Information (CIHI). However, the analyses, conclusions, opinions and statements expressed herein are those of the author, and not necessarily those of CIHI. We acknowledge support of the Ministry of Health and Long-Term Care in this report. All views expressed are those of the authors of this report and do not necessarily reflect those of Ontario or the Ministry.
Funding
No specific funding sources were used.
Author information
Authors and Affiliations
Contributions
All authors contributed substantially to this work, including conception and study design (SH, KF, AE, CH, SK), analysis (SH, EH, AB), and manuscript preparation (all).
Corresponding author
Ethics declarations
Conflict of interests
All co-authors have no conflicts of interest to disclose.
Ethics approval
Research ethics was not required as per the Ontario Health privacy office.
Consent to participate
Patient consent was not required for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Habbous, S., Barisic, A., Homenauth, E. et al. Estimating the incidence of breast cancer recurrence using administrative data. Breast Cancer Res Treat 198, 509–522 (2023). https://doi.org/10.1007/s10549-022-06812-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-022-06812-z