Abstract
Purpose
Breast cancer (BC) is the most common type of cancer among women in Brazil. Evidence shows that delayed treatment onset is associated with increased mortality. This study aimed to evaluate median days between diagnosis and treatment and factors associated with delayed start of treatment (> 60 days after diagnosis): stage, treatment received, subtype, epidemiological characteristics, and type of healthcare coverage.
Methods
This analysis included 1709 stage I–III BC patients from AMAZONA III, a prospective, observational study, diagnosed from January 2016 to March 2018 in 22 centers in Brazil.
Results
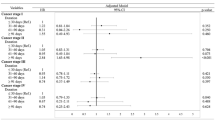
The median number of days from diagnosis to beginning of first oncologic treatment was 46 days (IQR 28–75) overall, 43 days (IQR 25–75) for stage I disease, 49 days (IQR 28–81) for stage II, and 44 days (IQR 30–68) for stage III, (p = 0.1180). According to first treatment received, diagnosis-to-treatment interval was 43 days (IQR 29–65) for neoadjuvant chemotherapy and 48 days (IQR 26–81) for surgery. Diagnosis-to-treatment interval was higher in women treated in the public system versus the private system (56 vs. 34 days, p < 0.0001). Patients in the public system had an increased odds of delayed treatment initiation (OR 4.74 95% CI 3.09–7.26, p < .0001). The longer interval from diagnosis to treatment in the public system was independent of clinical stage, type of treatment (systemic vs surgery first), subtype and region of the country.
Conclusion
By characterizing the delays in care delivery, our study will aid stakeholders to better design interventions and allocate resource to improve timely treatment for breast cancer in Brazil.
ClinicalTrials.gov Identifier: NCT02663973, registered on January, 26th, 2016.
Similar content being viewed by others
Data availability
Data can be made available upon request and according to LACOG policies.
References
Lee BL, Liedke PE, Barrios CH, Simon SD, Finkelstein DM, Goss PE (2012) Breast cancer in Brazil: present status and future goals. Lancet Oncol 13(3):e95–e102. https://doi.org/10.1016/S1470-2045(11)70323-0
Khorana AA, Tullio K, Elson P, Pennell NA, Grobmyer SR, Kalady MF, Raymond D, Abraham J, Klein EA, Walsh RM, Monteleone EE, Wei W, Hobbs B, Bolwell BJ (2019) Time to initial cancer treatment in the United States and association with survival over time: an observational study. PLoS ONE 14(3):e0213209. https://doi.org/10.1371/journal.pone.0213209.Erratum.In:PLoSOne.2019;14(4):e0215108
McLaughlin JM, Anderson RT, Ferketich AK, Seiber EE, Balkrishnan R, Paskett ED (2012) Effect on survival of longer intervals between confirmed diagnosis and treatment initiation among low-income women with breast cancer. J Clin Oncol 30(36):4493–4500. https://doi.org/10.1200/JCO.2012.39.7695
Shin DW, Cho J, Kim SY, Guallar E, Hwang SS, Cho B, Oh JH, Jung KW, Seo HG, Park JH (2013) Delay to curative surgery greater than 12 weeks is associated with increased mortality in patients with colorectal and breast cancer but not lung or thyroid cancer. Ann Surg Oncol 20(8):2468–2476. https://doi.org/10.1245/s10434-013-2957-y
Downing A, Twelves C, Forman D, Lawrence G, Gilthorpe MS (2014) Time to begin adjuvant chemotherapy and survival in breast cancer patients: a retrospective observational study using latent class analysis. Breast J 20(1):29–36. https://doi.org/10.1111/tbj.12209
Gagliato Dde M, Gonzalez-Angulo AM, Lei X, Theriault RL, Giordano SH, Valero V, Hortobagyi GN, Chavez-Macgregor M (2014) Clinical impact of delaying initiation of adjuvant chemotherapy in patients with breast cancer. J Clin Oncol 32(8):735–744. https://doi.org/10.1200/JCO.2013.49.7693
Hershman DL, Wang X, McBride R, Jacobson JS, Grann VR, Neugut AI (2006) Delay in initiating adjuvant radiotherapy following breast conservation surgery and its impact on survival. Int J Radiat Oncol Biol Phys 65(5):1353–1360. https://doi.org/10.1016/j.ijrobp.2006.03.048
Goss PE, Lee BL, Badovinac-Crnjevic T, Strasser-Weippl K, Chavarri-Guerra Y, St Louis J, Villarreal-Garza C, Unger-Saldaña K, Ferreyra M, Debiasi M, Liedke PE, Touya D, Werutsky G, Higgins M, Fan L, Vasconcelos C, Cazap E, Vallejos C, Mohar A, Knaul F, Arreola H, Batura R, Luciani S, Sullivan R, Finkelstein D, Simon S, Barrios C, Kightlinger R, Gelrud A, Bychkovsky V, Lopes G, Stefani S, Blaya M, Souza FH, Santos FS, Kaemmerer A, de Azambuja E, Zorilla AF, Murillo R, Jeronimo J, Tsu V, Carvalho A, Gil CF, Sternberg C, Dueñas-Gonzalez A, Sgroi D, Cuello M, Fresco R, Reis RM, Masera G, Gabús R, Ribeiro R, Knust R, Ismael G, Rosenblatt E, Roth B, Villa L, Solares AL, Leon MX, Torres-Vigil I, Covarrubias-Gomez A, Hernández A, Bertolino M, Schwartsmann G, Santillana S, Esteva F, Fein L, Mano M, Gomez H, Hurlbert M, Durstine A, Azenha G (2013) Planning cancer control in Latin America and the Caribbean. Lancet Oncol 14(5):391–436. https://doi.org/10.1016/S1470-2045(13)70048-2
Desai S, Hurley J, Takita C, Reis IM, Zhao W, Rodgers SE, Wright JL (2013) Impact of surgery-radiation interval on locoregional outcome in patients receiving neo-adjuvant therapy and mastectomy. Breast J 19(4):427–430. https://doi.org/10.1111/tbj.12140
Cordeiro E, Dixon M, Coburn N, Holloway CM (2015) A patient-centered approach to wait times in the surgical management of breast cancer in the province of Ontario. Ann Surg Oncol 22(8):2509–2516. https://doi.org/10.1245/s10434-014-4320-3
Bleicher RJ, Ruth K, Sigurdson ER, Beck JR, Ross E, Wong YN, Patel SA, Boraas M, Chang EI, Topham NS, Egleston BL (2016) Time to surgery and breast cancer survival in the United States. JAMA Oncol 2(3):330–339. https://doi.org/10.1001/jamaoncol.2015.4508.Erratum.In:JAMAOncol.2016;2(9):1244
Miles A, McClements PL, Steele RJ, Redeker C, Sevdalis N, Wardle J (2017) Perceived diagnostic delay and cancer-related distress: a cross-sectional study of patients with colorectal cancer. Psychooncology 26(1):29–36. https://doi.org/10.1002/pon.4093
Holland JC, Andersen B, Breitbart WS, Buchmann LO, Compas B, Deshields TL, Dudley MM, Fleishman S, Fulcher CD, Greenberg DB, Greiner CB, Handzo GF, Hoofring L, Hoover C, Jacobsen PB, Kvale E, Levy MH, Loscalzo MJ, McAllister-Black R, Mechanic KY, Palesh O, Pazar JP, Riba MB, Roper K, Valentine AD, Wagner LI, Zevon MA, McMillian NR, Freedman-Cass DA (2013) Distress management. J Natl Compr Canc Netw 11(2):190–209. https://doi.org/10.6004/jnccn.2013.0027
Posluszny DM, Dougall AL, Johnson JT, Argiris A, Ferris RL, Baum A, Bovbjerg DH, Dew MA (2015) Posttraumatic stress disorder symptoms in newly diagnosed patients with head and neck cancer and their partners. Head Neck 37(9):1282–1289. https://doi.org/10.1002/hed.23760
Robinson KM, Christensen KB, Ottesen B, Krasnik A (2012) Diagnostic delay, quality of life and patient satisfaction among women diagnosed with endometrial or ovarian cancer: a nationwide Danish study. Qual Life Res 21(9):1519–1525. https://doi.org/10.1007/s11136-011-0077-3
Debiasi M, Reinert T, Kaliks R, Amorim G, Caleffi M, Sampaio C, Fernandes GDS, Barrios CH (2016) Estimation of premature deaths from lack of access to anti-HER2 therapy for advanced breast cancer in the Brazilian public health system. J Glob Oncol 3(3):201–207. https://doi.org/10.1200/JGO.2016.005678
Silva GAE, Souza-Júnior PRB, Damacena GN, Szwarcwald CL (2017) Early detection of breast cancer in Brazil: data from the National Health Survey, 2013. Rev Saude Publica 51(suppl 1):14s. https://doi.org/10.1590/S1518-8787.2017051000191
Liedke PE, Finkelstein DM, Szymonifka J, Barrios CH, Chavarri-Guerra Y, Bines J, Vasconcelos C, Simon SD, Goss PE (2014) Outcomes of breast cancer in Brazil related to health care coverage: a retrospective cohort study. Cancer Epidemiol Biomarkers Prev 23(1):126–133. https://doi.org/10.1158/1055-9965.EPI-13-0693
Werutsky G, Nunes P, Barrios C (2019) Locally advanced breast cancer in Brazil: current status and future perspectives. Ecancermedicalscience 13:895. https://doi.org/10.3332/ecancer.2019.895
Law 12,732 (Nov, 22, 2012) Dispõe sobre o primeiro tratamento de paciente com neoplasia maligna comprovada e estabelece prazo para seu início. Diário Oficial da União on Nov, 23, 2012. http://www.planalto.gov.br/ccivil_03/_ato2011-2014/2012/lei/l12732.htm
Agência Nacional de Saúde Suplementar: General data. Brazil (2020). http://www.ans.gov.br/perfil-do-setor/dados-gerais. Accessed 28 May 2020
U.S. National Library of Medicine. ClinicaTrials.gov. https://clinicaltrials.gov/ct2/show/NCT02663973?term=NCT02663973. Accessed 05 Nov 2020
Souza CB, Fustinoni SM, Amorim MH, Zandonade E, Matos JC, Schirmer J (2015) Breast cancer: diagnosis-to-treatment waiting times for elderly women at a reference hospital of São Paulo, Brazil. Cien Saude Colet 20(12):3805–3816. https://doi.org/10.1590/1413-812320152012.00422015
INCA Instituto Nacional de Câncer (2020) Breast cancer in Brazil: synthesis of information. Brazil. https://www.inca.gov.br/sites/ufu.sti.inca.local/files/media/document/a_situacao_ca_mama_brasil_2019.pdf. Accessed 14 Jul 2020
Yoo TK, Han W, Moon HG, Kim J, Lee JW, Kim MK, Lee E, Kim J, Noh DY (2016) Delay of treatment initiation does not adversely affect survival outcome in breast cancer. Cancer Res Treat 48(3):962–969. https://doi.org/10.4143/crt.2015.173
Medeiros GC, Bergmann A, Aguiar SS, Thuler LC (2015) Análise dos determinantes que influenciam o tempo para o início do tratamento de mulheres com câncer de mama no Brasil [Determinants of the time between breast cancer diagnosis and initiation of treatment in Brazilian women]. Cad Saude Publica 31(6):1269–1282. https://doi.org/10.1590/0102-311X00048514
Dedey F, Wu L, Ayettey H, Sanuade OA, Akingbola TS, Hewlett SA, Tayo BO, Cole HV, de-Graft-Aikins A, Ogedegbe G, Adanu R, (2016) Factors associated with waiting time for breast cancer treatment in a teaching hospital in Ghana. Health Educ Behav 43(4):420–427. https://doi.org/10.1177/1090198115620417
Piñeros M, Sánchez R, Perry F, García OA, Ocampo R, Cendales R (2011) Demoras en el diagnóstico y tratamiento de mujeres con cáncer de mama en Bogotá, Colombia [Delay for diagnosis and treatment of breast cancer in Bogotá, Colombia]. Salud Publica Mex 53(6):478–485
Bleicher RJ (2018) Timing and delays in breast cancer evaluation and treatment. Ann Surg Oncol 25(10):2829–2838. https://doi.org/10.1245/s10434-018-6615-2
Acknowledgements
We would like to thank the patients, the research teams, and investigators for the dedication to this study. We acknowledge Instituto Avon, Itaú Seguros, and Grupo Bamaq for the financial support under the PRONON (Ministry of Health, Brazil) program and SAS Institute Inc. for providing license-free access to SAS®.
Funding
This study was funded by a Grant from Programa Nacional de Apoio à Atenção Oncológica (PRONON) of the Brazilian Health Ministry (No. 25000.173.901/2013-73).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interest
RMM, RGJ, GW, TFR, GQ, SDS, JB, DDR have nothing to disclose. CHB declares no relevant conflicts of interest under consideration for publication. CHB reports grants/research support: (to the institution) Pfizer, Novartis, Amgen, AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Roche/Genentech, Lilly, Sanofi, Taiho Pharmaceutical, Mylan, Merrimack, Merck, AbbVie, Astellas Pharma, BioMarin, Bristol-Myers Squibb, Daiichi Sankyo, Abraxis Biosciences, AB Science, Asana Biosciences, Medivation, Exelixis, ImClone Systems, LEO Pharma, Millennium, Merck KGaA, Shanghai Henlius Biotech, Polyphor, PharmaMar. Advisory Boards and Consulting: Boehringer-Ingelheim, GSK, Novartis, Pfizer, Roche/Genentech, Eisai, Bayer, MSD, Astra Zeneca, Zodiac, Lilly, Sanofi.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Hospital Moinhos de Vento (Date September, 18th, 2015 /No 1.234.499).”
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maschmann, R.M., De Jesus, R.G., Werutsky, G. et al. Time interval between diagnosis to treatment of breast cancer and the impact of health insurance coverage: a sub analysis of the AMAZONA III Study (GBECAM 0115). Breast Cancer Res Treat 198, 123–130 (2023). https://doi.org/10.1007/s10549-022-06809-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-022-06809-8