Abstract
Purpose
To characterize the distress trajectory in patients with newly diagnosed, non-metastatic breast cancer from pre-neoadjuvant chemotherapy until 12 months after onset of treatment and to identify demographic and clinical predictors of distress in these patients.
Methods
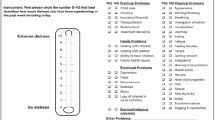
In a retrospective, longitudinal study, chart review data were abstracted for 252 eligible patients treated at a comprehensive cancer care center. The center screens for distress at least monthly with the distress thermometer; the highest distress score per month was included in the analyses. The growth trajectory was established using mixed modeling and predictors were added to the initial growth model in subsequent models.
Results
Distress showed a cubic growth trajectory with highest distress prior to treatment onset followed by a steep decline in the first three months of treatment. A slight increase in distress was apparent over months 6–10. Being Hispanic was associated with a stronger increase in distress in the second half of the year (p = 0.012). NACT was associated with lower distress and surgery with higher distress (both: p < 0.001).
Conclusion
Distress is at its peak prior to treatment onset and rapidly decreases once treatment has started. Oncologist should be aware that both completion of NACT and undergoing surgery are associated with increases in distress and Hispanic patients may be more at risk for an increase in distress at these times; this suggests that careful monitoring of distress during the treatment trajectory and in Hispanic patients in particular in order to provide timely support.

Similar content being viewed by others
Data availability
The data that support the findings of this study are available on reasonable request form the corresponding author.
References
National Comprehensive Cancer Network I. 2022. Distress Management. NCCN Clinical Practice Guidelines in Oncology 2022.
Mehnert A, Hartung TJ, Friedrich M, Vehling S et al (2017) One in two cancer patients is significantly distressed: prevalence and indicators of distress. Psychooncology. https://doi.org/10.1002/pon.4464
Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C et al (2001) The prevalence of psychological distress by cancer site. Psychooncology 10(1):19–28. https://doi.org/10.1002/1099-1611(200101/02)10:1%3c19::AID-PON501%3e3.0.CO;2-6
Härtl K, Engel J, Herschbach P, Reinecker H et al (2010) Personality traits and psychosocial stress: quality of life over 2 years following breast cancer diagnosis and psychological impact factors. Psychooncology 19(2):160–169. https://doi.org/10.1002/pon.1536
Hegel MT, Moore CP, Collins ED, Kearing S et al (2006) Distress, psychiatric syndromes, and impairment of function in women with newly diagnosed breast cancer. Cancer 107(12):2924–2931. https://doi.org/10.1002/cncr.22335
Lutgendorf SK, Sood AK, Antoni MH (2010) Host factors and cancer progression: biobehavioral signaling pathways and interventions. J clin oncol 28(26):4094–4099. https://doi.org/10.1200/JCO.2009.26.9357
Oh H-M, Son C-G (2021) The risk of psychological stress on cancer recurrence: a systematic review. Cancers 13(22):5816. https://doi.org/10.3390/cancers13225816
Groenvold M, Petersen MA, Idler E, Bjorner JB et al (2007) Psychological distress and fatigue predicted recurrence and survival in primary breast cancer patients. Breast Cancer Res Treat 105(2):209–219. https://doi.org/10.1007/s10549-006-9447-x
Adeyemi OJ, Gill TL, Paul R, Huber LB (2021) Evaluating the association of self-reported psychological distress and self-rated health on survival times among women with breast cancer in the U.S. PLoS ONE 16(12):e0260481. https://doi.org/10.1371/journal.pone.0260481
Antoni MH, Lechner SC, Kazi A, Wimberly SR et al (2006) How stress management improves quality of life after treatment for breast cancer. J Consult Clin Psychol 74(6):1143–1152. https://doi.org/10.1037/0022-006x.74.6.1152
Andersen BL, Yang H-C, Farrar WB, Golden-Kreutz DM et al (2008) Psychologic intervention improves survival for breast cancer patients: a randomized clinical trial. Cancer 113(12):3450–3458. https://doi.org/10.1002/cncr.23969
Yang H-C, Thornton LM, Shapiro CL, Andersen BL (2008) Surviving recurrence: psychological and quality-of-life recovery. Cancer 112(5):1178–1187. https://doi.org/10.1002/cncr.23272
Kant J, Czisch A, Schott S, Siewerdt-Werner D et al (2018) Identifying and predicting distinct distress trajectories following a breast cancer diagnosis—from treatment into early survival. J Psychosom Res 115:6–13. https://doi.org/10.1016/j.jpsychores.2018.09.012
Renna ME, Shrout MR, Madison AA, Alfano CM et al (2020) Within-person changes in cancer-related distress predict breast cancer survivors’ inflammation across treatment. Psychoneuroendocrinology 121:104866. https://doi.org/10.1016/j.psyneuen.2020.104866
Culver JL, Arena PL, Antoni MH, Carver CS (2002) Coping and distress among women under treatment for early stage breast cancer: comparing african americans, hispanics and non-hispanic whites. Psychooncology 11(6):495–504. https://doi.org/10.1002/pon.615
Fayanju OM, Yenokyan K, Ren Y, Goldstein BA et al (2019) The effect of treatment on patient-reported distress after breast cancer diagnosis. Cancer 125(17):3040–3049. https://doi.org/10.1002/cncr.32174
Fayanju OM, Ren Y, Stashko I, Power S et al (2021) Patient-reported causes of distress predict disparities in time to evaluation and time to treatment after breast cancer diagnosis. Cancer 127(5):757–768. https://doi.org/10.1002/cncr.33310
Wittenberg L, Yutsis M, Taylor S, Giese-Davis J et al (2010) Marital status predicts change in distress and well-being in women newly diagnosed with breast cancer and their peer counselors. Breast J 16(5):481–489. https://doi.org/10.1111/j.1524-4741.2010.00964.x
Mertz BG, Bistrup PE, Johansen C, Dalton SO et al (2012) Psychological distress among women with newly diagnosed breast cancer. Eur J Oncol Nurs 16(4):439–443. https://doi.org/10.1016/j.ejon.2011.10.001
Politi MC, Enright TM, Weihs KL (2007) The effects of age and emotional acceptance on distress among breast cancer patients. Support Care Cancer 15(1):73–79. https://doi.org/10.1007/s00520-006-0098-6
Pirl WF, Fann JR, Greer JA, Braun I et al (2014) Recommendations for the implementation of distress screening programs in cancer centers: report from the American psychosocial oncology society (APOS), association of oncology social work (AOSW), and oncology nursing society (ons) joint task force. Cancer 120(19):2946–2954. https://doi.org/10.1002/cncr.28750
Ma X, Zhang J, Zhong W, Shu C et al (2014) The diagnostic role of a short screening tool–the distress thermometer: a meta-analysis. Support Care Cancer 22(7):1741–1755. https://doi.org/10.1007/s00520-014-2143-1
Ploos van Amstel FK, Tol J, Sessink KH, van der Graaf WTA et al (2017) A specific distress cutoff score shortly after breast cancer diagnosis. Cancer Nurs 40(3):E35-e40. https://doi.org/10.1097/ncc.0000000000000380
Corporation I. IBM SPSS Statistics for Windows 1989. 2016 Armon, N.Y
Kuznetsova A, Brockhoff PB, Christensen RHB (2017) lmerTest package: tests in linear mixed effects models. J Stat Softw 82(13):1–26. https://doi.org/10.18637/jss.v082.i13
Bates D, Mächler M, Bolker B, Walker S (2015) Fitting linear mixed-effects models using lme4. J Stat Softw 67(1):1–48. https://doi.org/10.18637/jss.v067.i01
Wang J, Haiyi X, Fisher JH (2012) Application of multilevel modelling to longitudinal data, in Multilevel Models. Applications using SAS. Higher Eduction Press and Walter de Gruyter GmbH & Co., Berlin
Helgeson VS, Snyder P, Seltman H (2004) Psychological and physical adjustment to breast cancer over 4 years: identifying distinct trajectories of change. Health Psychol 23(1):3
Assari S, Khoshpouri P, Chalian H (2019) Combined effects of race and socioeconomic status on cancer beliefs, cognitions, and emotions. Healthcare (Basel, Switzerland) 7(1):17. https://doi.org/10.3390/healthcare7010017
Ashing-Giwa KT, Padilla G, Tejero J, Kraemer J et al (2004) Understanding the breast cancer experience of women: a qualitative study of African American, Asian American. Lat Cauc Cancer Surviv Psychooncology 13(6):408–428. https://doi.org/10.1002/pon.750
Thomas EJ, Elliott R (2009) Brain imaging correlates of cognitive impairment in depression. Front Hum Neurosci. https://doi.org/10.3389/neuro.09.030.2009
Spencer SM, Lehman JM, Wynings C, Arena P et al (1999) Concerns about breast cancer and relations to psychosocial well-being in a multiethnic sample of early-stage patients. Health Psychol 18(2):159–168. https://doi.org/10.1037/0278-6133.18.2.159
Funding
This work was supported by the National Institutes of Health/National Cancer Institute under award number (Grant No. P30CA016672).
Author information
Authors and Affiliations
Contributions
TL and DT contributed to the study conception and design. Material preparation and data collection were performed by TL and ET. Analyses were performed by TL. The first draft of the manuscript was written by TL and ZK. All authors commented on previous versions of the manuscript and read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This observational study and a corresponding waiver for consent was approved by the institution’s Internal Review Board.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lacourt, T.E., Koncz, Z., Tullos, E.A. et al. A detailed description of the distress trajectory from pre- to post-treatment in breast cancer patients receiving neoadjuvant chemotherapy. Breast Cancer Res Treat 197, 299–305 (2023). https://doi.org/10.1007/s10549-022-06805-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-022-06805-y