Abstract
Purpose
Metformin has demonstrated a chemoprotective effect in breast cancer but there is limited evidence on the effect of cumulative exposure to metformin and the risk of hormone receptor-positive and human epidermal growth factor receptor 2-negative (HR + /HER2-) breast cancer. This study assessed this risk with dose and intensity of metformin in postmenopausal women with type-2 diabetes mellitus (T2DM).
Methods
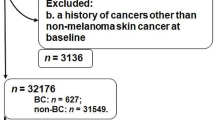
This nested case–control study used the Surveillance, Epidemiology, and End Results-Medicare data (2008–2015). Cohort entry was the date of incident T2DM diagnosis. Cases were those diagnosed with HR + /HER2- breast cancer (event date) as their first/only cancer. Non-cancer T2DM controls were matched using variable-ratio-matching. Cumulative dose and average intensity of metformin were measured during the 1-year lookback period. Dose(mg) was categorized as: (1)0, (2)0–30,000, (3)30,001–136,000, (4)136,001–293,000, and (5) > 293,000, and intensity(mg/day) as: 0, 1–500, and > 500. Covariates were conceptualized using the Andersen Behavioral Model. Conditional logistic regression was used to assess the risk of HR + /HER2- breast cancer with metformin-use.
Results
There were 690 cases and 2747 controls. The median duration of T2DM was 1178 days in controls and 1180 days in cases. Higher cumulative dose categories: 4 (adjusted odds ratio(aOR) = 0.72, 95% CI 0.55–0.95,p = 0.02), and 5 (OR = 0.60, 95% CI 0.42–0.85,p < 0.01) had significantly lower odds of HR + /HER2- breast cancer compared to category 0. The highest intensity category of metformin had 39% lower odds of HR + /HER2- breast cancer (OR = 0.61, 95% CI 0.46–0.82,p < 0.01) compared to the 0 mg/day group.
Conclusions
Higher metformin exposure was associated with reduced risk of HR + /HER2- breast cancer, adding to the evidence supporting metformin’s chemoprotective effect.


Similar content being viewed by others
Data availability
This study used the linked SEER-Medicare database. The interpretation and reporting of these data are the sole responsibility of the authors. The authors acknowledge the efforts of the National Cancer Institute; the Office of Research, Development and Information, CMS; Information Management Services (IMS), Inc.; and the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries in the creation of the SEER-Medicare database. The data that support the findings of this study are available from IMS, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available.
References
Fowler MJ (2008) Microvascular and macrovascular complications of diabetes. Clin Diabetes 26:77–82
Kang C, LeRoith D, Gallagher EJ (2018) Diabetes, obesity, and breast cancer. Endocrinology 159:3801–3812
Vigneri P, Frasca F, Sciacca L, Pandini G, Vigneri R (2009) Diabetes and cancer. Endocr Relat Cancer 16:1103–1123
Boyle P, Boniol M, Koechlin A, Robertson C, Valentini F, Coppens K et al (2012) Diabetes and breast cancer risk: a meta-analysis. Br J Cancer 107:1608–1617
Michels KB, Solomon CG, Hu FB, Rosner BA, Hankinson SE, Colditz GA et al (2003) Type 2 diabetes and subsequent incidence of breast cancer in the nurses’ health study. Diabetes Care 26:1752–1758
Shlomai G, Neel B, LeRoith D, Gallagher EJ (2016) Type 2 diabetes mellitus and cancer: the role of pharmacotherapy. J Clin Oncol. https://doi.org/10.1200/JCO.2016.67.4044
Panno ML, Salerno M, Pezzi V, Sisci D, Maggiolini M, Mauro L et al (1996) Effect of oestradiol and insulin on the proliferative pattern and on oestrogen and progesterone receptor contents in MCF-7 cells. J Cancer Res Clin Oncol 122:745–749
Rose DP, Vona-Davis L (2012) The cellular and molecular mechanisms by which insulin influences breast cancer risk and progression. Endocr Relat Cancer 19:R225–R241
Zhang K, Bai P, Dai H, Deng Z. Metformin and risk of cancer among patients with type 2 diabetes mellitus: A systematic review and meta-analysis. Primary Care Diabetes [Internet]. 2020; Available from: https://linkinghub.elsevier.com/retrieve/pii/S1751991820302138
Tang GH, Satkunam M, Pond GR, Steinberg GR, Blandino G, Schunemann HJ et al (2018) Association of metformin with breast cancer incidence and mortality in patients with type II diabetes: a GRADE-Assessed systematic review and meta-analysis. Cancer Epidemiol Biomark Prev. https://doi.org/10.1158/1055-9965.EPI-17-0936
Col NF, Ochs L, Springmann V, Aragaki AK, Chlebowski RT (2012) Metformin and breast cancer risk: a meta-analysis and critical literature review. Breast Cancer Res Treat. https://doi.org/10.1007/s10549-012-2170-x
Giovannucci E, Harlan DM, Archer MC, Bergenstal RM, Gapstur SM, Habel LA et al (2010) Diabetes and cancer: a consensus report. Diabetes Care 33:1674–1685
Surveillance Epidemiology and End Results Program, National Cancer Institute. Cancer Stat Facts: Female Breast Cancer Subtypes [Internet]. 2019 [cited 2019 Dec 1]. Available from: https://seer.cancer.gov/statfacts/html/breast-subtypes.html
Peila R, Rohan TE (2020) Diabetes, glycated hemoglobin, and risk of cancer in the UK Biobank Study. Cancer Epidemiol Biomark Prev. https://doi.org/10.1158/1055-9965.EPI-19-1623
Zhang J, Xu H, Zhou X, Li Y, Liu T, Yin X et al (2017) Role of metformin in inhibiting estrogen-induced proliferation and regulating ERα and ERβ expression in human endometrial cancer cells. Oncol Lett 14:4949–4956
Daugan M, Dufaÿ Wojcicki A, d’Hayer B, Boudy V (2016) Metformin: an anti-diabetic drug to fight cancer. Pharmacol Res. https://doi.org/10.1016/j.phrs.2016.10.006
Checkley LA, Rudolph MC, Wellberg EA, Giles ED, Wahdan-Alaswad RS, Houck JA et al (2017) Metformin accumulation correlates with organic cation transporter 2 protein expression and predicts mammary tumor regression in vivo. Cancer Prev Res. https://doi.org/10.1158/1940-6207.CAPR-16-0211-T
Evans JMM, Donnelly LA, Emslie-Smith AM, Alessi DR, Morris AD (2005) Metformin and reduced risk of cancer in diabetic patients. Br Med J. https://doi.org/10.1136/bmj.38415.708634.F7
Surveillance Epidemiology and End Results Program, National Cancer Institute, National Institutes of Health. List of SEER Registries [Internet]. [cited 2020 Apr 18]. Available from: https://seer.cancer.gov/registries/list.html
Hebert PL, Geiss LS, Tierney EF, Engelgau MM, Yawn BP, McBean AM (1999) Identifying persons with diabetes using medicare claims data. Am J Med Qual. https://doi.org/10.1177/106286069901400607
Rector TS, Wickstrom SL, Shah M, Greeenlee NT, Rheault P, Rogowski J et al (2004) Specificity and sensitivity of claims-based algorithms for identifying members of Medicare+choice health plans that have chronic medical conditions. Health Serv Res. https://doi.org/10.1111/j.1475-6773.2004.00321.x
Surveillance Epidemiology and End Results Program, National Cancer Institute, National Institutes of Health. ICD-O-3 Site Codes [Internet]. National Institutes of Health. [cited 2020 Apr 18]. Available from: https://training.seer.cancer.gov/breast/abstract-code-stage/codes.html
Surveillance Epidemiology and End Results Program, National Cancer Institute, National Institutes of Health. Breast Subtype (2010+) [Internet]. National Institutes of Health. [cited 2020 Apr 18]. Available from: https://seer.cancer.gov/seerstat/databases/ssf/breast-subtype.html
Chang CH, Lin JW, Wu LC, Lai MS, Chuang LM (2012) Oral insulin secretagogues, insulin, and cancer risk in type 2 diabetes mellitus. J Clin Endocrinol Metab. https://doi.org/10.1210/jc.2012-1162
Pottegård A, Friis S, Stürmer T, Hallas J, Bahmanyar S (2018) Considerations for pharmacoepidemiological studies of drug-cancer associations. Basic Clin Pharmacol Toxicol. https://doi.org/10.1111/bcpt.12946
Dankner R, Boker LK, Boffetta P, Balicer RD, Murad H, Berlin A, et al. A historical cohort study on glycemic-control and cancer-risk among patients with diabetes. Cancer Epidemiology [Internet]. 2018;57:104–9. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1877782118301097
Johnson JA, Carstensen B, Witte D, Bowker SL, Lipscombe L, Renehan AG (2012) Diabetes and cancer (1): evaluating the temporal relationship between type 2 diabetes and cancer incidence. Diabetologia. https://doi.org/10.1007/s00125-012-2525-1
Arfè A, Corrao G (2016) The lag-time approach improved drug–outcome association estimates in presence of protopathic bias. J Clin Epidemiol. https://doi.org/10.1016/j.jclinepi.2016.03.003
Gomes T, Juurlink DN, Antoniou T, Mamdani MM, Paterson JM, van den Brink W (2017) Gabapentin, opioids, and the risk of opioid-related death: a population-based nested case–control study. PLoS Med. https://doi.org/10.1371/journal.pmed.1002396
Andersen R (1968) A Behavioral model of families’ use of health services. Center for Health Administration Studies. University of Chicago, Chicago, IL
Andersen RM (1995) Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav. https://doi.org/10.2307/2137284
Rosato V, Bosetti C, Talamini R, Levi F, Montella M, Giacosa A et al (2011) Metabolic syndrome and the risk of breast cancer in postmenopausal women. Ann Oncol. https://doi.org/10.1093/annonc/mdr025
Klil-Drori AJ, Azoulay L, Pollak MN (2017) Cancer, obesity, diabetes, and antidiabetic drugs: is the fog clearing? Nat Rev Clin Oncol. https://doi.org/10.1038/nrclinonc.2016.120
Mayo Clinic. Breast cancer chemoprevention: Medicines that reduce breast cancer risk [Internet]. Mayo Clinic. 2019 [cited 2020 Apr 18]. Available from: https://www.mayoclinic.org/diseases-conditions/breast-cancer/in-depth/breast-cancer/art-20045353
Gapstur SM, Morrow M, Sellers TA. Hormone Replacement Therapy and Risk of Breast Cancer With a Favorable Histology. JAMA [Internet]. 1999;281:2091. Available from: http://jama.jamanetwork.com/article.aspx?doi=10.1001/jama.281.22.2091
Chang HY, Weiner JP, Richards TM, Bleich SN, Segal JB (2012) Validating the adapted diabetes complications severity index in claims data. Am J Managed Care 18:721–726
Bosco JLF, Antonsen S, Sorensen HT, Pedersen L, Lash TL (2011) Metformin and incident breast cancer among diabetic women: a population-based case-control study in Denmark. Cancer Epidemiol Biomark Prev. https://doi.org/10.1158/1055-9965.EPI-10-0817
Elixhauser A, Steiner C, Harris DR, Coffey RM (1998) Comorbidity measures for use with administrative data. Med Care. https://doi.org/10.1097/00005650-199801000-00004
Mathur MB, Ding P, Riddell CA, VanderWeele TJ (2018) Web site and R package for computing E-values. Epidemiology. https://doi.org/10.1097/EDE.0000000000000864
van der Weele TJ, Ding P (2017) Sensitivity analysis in observational research: introducing the E-Value. Ann Intern Med. https://doi.org/10.7326/M16-2607
Park Y-MM, Bookwalter DB, O’Brien KM, Jackson CL, Weinberg CR, Sandler DP. A prospective study of type 2 diabetes, metformin use, and risk of breast cancer. Annals of Oncology [Internet]. 2021;32:351–9. Available from: https://linkinghub.elsevier.com/retrieve/pii/S0923753420432144
Palmer JR, Castro-Webb N, Bertrand K, Bethea TN, Denis Gv (2017) Type II diabetes and incidence of estrogen receptor negative breast cancer in African American women. Cancer Res. https://doi.org/10.1158/0008-5472.CAN-17-1903
Bodmer M, Meier C, Krähenbühl S, Jick SS, Meier CR (2010) Long-term metformin use is associated with decreased risk of breast cancer. Diabetes Care 33:1304–1308
Tseng CH (2014) Metformin may reduce breast cancer risk in Taiwanese women with type 2 diabetes. Breast Cancer Res Treat 145:785–790
Singletary SE (2003) Rating the risk factors for breast cancer. Ann Surg. https://doi.org/10.1097/01.SLA.0000059969.64262.87
Xia X, Chen W, Li J, Chen X, Rui R, Liu C et al (2014) Body mass index and risk of breast cancer: a nonlinear dose-response meta-analysis of prospective studies. Scientific Rep. https://doi.org/10.1038/srep07480
Lambertini M, Santoro L, del Mastro L, Nguyen B, Livraghi L, Ugolini D et al (2016) Reproductive behaviors and risk of developing breast cancer according to tumor subtype: a systematic review and meta-analysis of epidemiological studies. Cancer Treat Rev. https://doi.org/10.1016/j.ctrv.2016.07.006
Anderson KN, Schwab RB, Martinez ME (2014) Reproductive risk factors and breast cancer subtypes: a review of the literature. Breast Cancer Res Treat. https://doi.org/10.1007/s10549-014-2852-7
Acknowledgements
This study used the linked SEER-Medicare database. The interpretation and reporting of these data are the sole responsibility of the authors. The authors acknowledge the efforts of the National Cancer Institute; the Office of Research, Development and Information, CMS; Information Management Services (IMS), Inc.; and the Surveillance, Epidemiology, and End Results (SEER) Program tumor registries in the creation of the SEER-Medicare database.
Funding
This research received no funding from any agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. The first draft of the manuscript was written by SGC and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. Individual contributions are: SGC: Conceptualization, data curation, formal analysis, methodology, writing, reviewing, editing. MS: Conceptualization, methodology, reviewing and editing. SMA: Conceptualization, methodology, reviewing and editing. Rajender R. Aparasu: Conceptualization, methodology and reviewing. MVT: Conceptualization, methodology and reviewing. MLJ: Resources, funding acquisition, conceptualization, methodology, reviewing and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors have nothing to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Previous meeting presentation: Meeting date: ISPOR 2021, May 17-20, 2021. Meeting date: ASCO 2021, June 4-8, 2021.
Supplementary Information
Below is the link to the electronic supplementary material.
10549_2022_6706_MOESM2_ESM.pdf
Supplementary eFigure 2 (Forest plot of multivariable analysis (odds ratios with 95% confidence intervals) (Model 2). [Legend: Average daily intensity of metformin: Category 0: 0 mg/day, Category 1: 0 mg/day < intensity ≤ 500 mg/day, Category 2: intensity > 500 mg/day (category 2)]Abbreviations: aDCSI- adapted Diabetes Complications Severity Index. Description: The horizontal axis shows the odds ratios in the multivariable model. The blue dot represent the odds ratio estimate for the variable and the bounds around the dot represent the 95% confidence interval. (PDF 295 kb)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chikermane, S.G., Sharma, M., Abughosh, S.M. et al. Dose-dependent relation between metformin and the risk of hormone receptor-positive, her2-negative breast cancer among postmenopausal women with type-2 diabetes. Breast Cancer Res Treat 195, 421–430 (2022). https://doi.org/10.1007/s10549-022-06706-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-022-06706-0