Abstract
Purpose
The definition of "no tumor on ink" is generally applied for clear resection margin (RM) after breast-conserving surgery (BCS). However, few studies reported the effect of RM in the setting of neoadjuvant chemotherapy (NAC). We investigated the association between RM status and survival outcomes for those who underwent BCS after NAC for breast cancer.
Methods
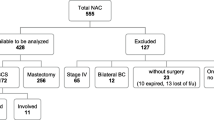
We retrospectively reviewed the data of 2,803 patients who underwent BCS and whole-breast irradiation after NAC between January 2008 and December 2016 from three institutions in South Korea.
Results
The 786 patients in the pathologic complete response group (RpCR) had significantly longer local recurrence-free survival (LRFS) than the 1,949 patients in clear or close RM and non-pCR group (R0) and the 68 patients in involved RM and non-pCR group (R1) (vs. R0, p = 0.001; vs. R1, p = 0.049). Patients in R0 showed no benefit in LRFS compared to R1 on both log-rank test (HR = 1.20; 95% C.I., 0.49–2.93; p = 0.692) and Cox regression analysis (HR = 2.05; 95% C.I., 0.64–6.58; p = 0.227). Subgroup analysis according to tumor subtypes revealed that there was no significant difference in LRFS, distant metastasis-free survival, and recurrence-free survival between the R0 and R1 group. Additionally, among 286 patients with pCR with residual ductal carcinoma in situ (DCIS) alone, RM status was not significantly associated with LRFS.
Conclusion
Clear RM of specimen does not have benefit on LRFS after NAC. Additionally, for the patients showing pCR with residual DCIS in the breast, margin involvement also did not affect the risk of local recurrence.




Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Puig CA, Hoskin TL, Day CN et al (2017) National trends in the use of neoadjuvant chemotherapy for hormone receptor-negative breast cancer: A national cancer data base study. Ann Surg Oncol 24:1242–1250. https://doi.org/10.1245/s10434-016-5733-y
Colomer R, Saura C, Sánchez-Rovira P et al (2019) Neoadjuvant management of early breast cancer: A clinical and investigational position statement. Oncologist 24:603–611. https://doi.org/10.1634/theoncologist.2018-0228
Schott AF, Hayes DF (2012) Defining the benefits of neoadjuvant chemotherapy for breast cancer. J Clin Oncol 30:1747–1749. https://doi.org/10.1200/JCO.2011.41.3161
Rastogi P, Anderson SJ, Bear HD et al (2008) Preoperative chemotherapy: updates of national surgical adjuvant breast and bowel project protocols B-18 and B-27. J Clin Oncol 26:778–785. https://doi.org/10.1200/JCO.2007.15.0235
National Comprehensive Cancer Network (2021) Breast Cancer (Version 3.2021). https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed 19 Apr 2021
Cardoso F, Kyriakides S, Ohno S et al (2019) Early breast cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 30:1194–1220. https://doi.org/10.1093/annonc/mdz173
Moran MS, Schnitt SJ, Giuliano AE et al (2014) Society of surgical oncology-American society for radiation oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in stages i and II invasive breast cancer. Int J Radiat Oncol Biol Phys 88:553–564. https://doi.org/10.1016/j.ijrobp.2013.11.012
Russo AL, Arvold ND, Niemierko A et al (2013) Margin status and the risk of local recurrence in patients with early-stage breast cancer treated with breast-conserving therapy. Breast Cancer Res Treat 140:353–361. https://doi.org/10.1007/s10549-013-2627-6
Park CC, Mitsumori M, Nixon A et al (2000) Outcome at 8 years after breast-conserving surgery and radiation therapy for invasive breast cancer: Influence of margin status and systemic therapy on local recurrence. J Clin Oncol 18:1668–1675. https://doi.org/10.1200/JCO.2000.18.8.1668
Lin J, Lin KJ, Wang YF et al (2020) Association of surgical margins with local recurrence in patients undergoing breast-conserving surgery after neoadjuvant chemotherapy. BMC Cancer 20:1–9. https://doi.org/10.1186/s12885-020-06955-6
Chen AM, Meric-Bernstam F, Hunt KK et al (2004) Breast conservation after neoadjuvant chemotherapy: the M.D. Anderson cancer center experience. J Clin Oncol 22:2303–2312. https://doi.org/10.1200/JCO.2004.09.062
Haussmann J, Corradini S, Nestle-Kraemling C et al (2020) Recent advances in radiotherapy of breast cancer. Radiat Oncol 15:71. https://doi.org/10.1186/s13014-020-01501-x
Morrow M, van Zee KJ, Solin LJ et al (2016) Society of surgical oncology-American society for radiation oncology-American society of clinical oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in ductal carcinoma in situ. J Clin Oncol 34:4040–4046. https://doi.org/10.1200/JCO.2016.68.3573
Allison KH, Hammond MEH, Dowsett M et al (2020) Estrogen and progesterone receptor testing in breast cancer: ASCO/CAP guideline update. J Clin Oncol 38:1346–1366. https://doi.org/10.1200/JCO.19.02309
Yoon TI, Lee JW, Lee SB et al (2018) No association of positive superficial and/or deep margins with local recurrence in invasive breast cancer treated with breast-conserving surgery. Cancer Res Treat 50:275–282. https://doi.org/10.4143/crt.2017.041
Wimmer K, Bolliger M, Bago-Horvath Z et al (2020) Impact of surgical margins in breast cancer after preoperative systemic chemotherapy on local recurrence and survival. Ann Surg Oncol 27:1700–1707. https://doi.org/10.1245/s10434-019-08089-x
Tyler S, Truong PT, Lesperance M et al (2018) Close margins less than 2 mm are not associated with higher risks of 10-year local recurrence and breast cancer mortality compared with negative margins in women treated with breast-conserving therapy. Int J Radiat Oncol Biol Phys 101:661–670. https://doi.org/10.1016/j.ijrobp.2018.03.005
Volders JH, Haloua MH, Krekel NMA et al (2016) Neoadjuvant chemotherapy in breast-conserving surgery – consequences on margin status and excision volumes: a nationwide pathology study. Eur J Surg Oncol 42:986–993. https://doi.org/10.1016/j.ejso.2016.02.252
Tang R, Coopey SB, Specht MC et al (2015) Lumpectomy specimen margins are not reliable in predicting residual disease in breast conserving surgery. Am J Surg 210:93–98. https://doi.org/10.1016/j.amjsurg.2014.09.029
Mann RM, Cho N, Moy L (2019) Reviews and Commentary • State of the Art. Radiology 292:520–536
Loo CE, Straver ME, Rodenhuis S et al (2011) Magnetic resonance imaging response monitoring of breast cancer during neoadjuvant chemotherapy: relevance of Breast Cancer Subtype. J Clin Oncol 29:660–666. https://doi.org/10.1200/JCO.2010.31.1258
Mo H, Kim Y, Rhu J et al (2017) Actual conversion rate from total mastectomy to breast conservation after neoadjuvant chemotherapy for stages II–III breast cancer patients. J Breast Disease 5:51–56. https://doi.org/10.14449/jbd.2017.5.2.51
Cho WK, Choi DH, Park W et al (2019) Is higher dose radiation necessary for positive resection margin after breast-conserving surgery for breast cancer? Breast 47:16–21. https://doi.org/10.1016/j.breast.2019.06.005
Kim S, il, Sohn J, Koo JS, et al (2011) Molecular subtypes and tumor response to neoadjuvant chemotherapy in patients with locally advanced breast cancer. Oncology 79:324–330. https://doi.org/10.1159/000322192
Liedtke C, Mazouni C, Hess KR et al (2008) Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J Clin Oncol 26:1275–1281. https://doi.org/10.1200/JCO.2007.14.4147
Pastorello RG, Laws A, Grossmith S et al (2020) Clinico-pathologic predictors of patterns of residual disease following neoadjuvant chemotherapy for breast cancer. Mod Pathol. https://doi.org/10.1038/s41379-020-00714-5
Ballesio L, Gigli S, di Pastena F et al (2017) Magnetic resonance imaging tumor regression shrinkage patterns after neoadjuvant chemotherapy in patients with locally advanced breast cancer: Correlation with tumor biological subtypes and pathological response after therapy. Tumor Biology. https://doi.org/10.1177/1010428317694540
Sharma P, López-Tarruella S, García-Saenz JA et al (2018) Pathological response and survival in triple-negative breast cancer following neoadjuvant carboplatin plus docetaxel. Clin Cancer Res 24:5820–5829. https://doi.org/10.1158/1078-0432.CCR-18-0585
Pilewskie M, Morrow M (2018) Margins in breast cancer: how much is enough? Cancer 124:1335–1341. https://doi.org/10.1002/cncr.31221
Mazouni C, Peintinger F, Wan-Kau S et al (2007) Effect on patient outcome of residual DCIS in patients with complete eradication of invasive breast cancer after neoadjuvant chemotherapy. J Clin Oncol 25:530–530. https://doi.org/10.1200/jco.2007.25.18_suppl.530
Jones RL, Lakhani SR, Ring AE et al (2006) Pathological complete response and residual DCIS following neoadjuvant chemotherapy for breast carcinoma. Br J Cancer 94:358–362. https://doi.org/10.1038/sj.bjc.6602950
Acknowledgements
The authors would like to sincerely appreciate Mr. Yong Seop Lee and Ms. Sun Hee Kang for financial support to conduct research in the department of breast surgery, Samsung Medical Center. Additionally, we thank Dr. Sae Byul Lee, Jisun Kim, Il Yong Chung, Hee Jeong Kim, Beom Seok Ko, Jong Won Lee, Byung Ho Son, and Sei-hyun Ahn (Division of Breast Surgery, Department of Surgery, University of Ulsan College of Medicine, Asan Medical Center, Seoul, South Korea) for critical advice and consultation.
Funding
This study was conducted with the support of the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (2018R1D1A1A09081884) and by the MSIT (Ministry of Science and ICT), Korea, under the ICT Creative Consilience program (IITP-2020–0-01821) supervised by the IITP (Institute for Information & communications Technology Planning & Evaluation) and by SMC-SKKU Future Convergence Program (Grant SMO1190341).
Author information
Authors and Affiliations
Contributions
All authors whose names appear on the submission made substantial contributions to the conception of design of the work or the acquisition, analysis, or interpretation or data; drafted the work or revised it critically for important intellectual content; approved the version to be published; and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
Han-Byoel Lee and Wonshik Han report being a member on the board of directors of and holding stock and ownership interests at DCGen, Co., Ltd., not relevant to this study. Other authors declare no competing interests.
Ethical approval
The study was performed in accordance with the Declaration of Helsinki or comparable ethical standards. Approval was granted by the ethics committee or institutional review board at the participating sites.
Informed consent
Requirement for informed consent was waived for all patients.
Consent to publication
All authors have read the paper and consent to its publication.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Cheun, JH., Lee, Y.J., Lee, JH. et al. Surgical margin status and survival outcomes of breast cancer patients treated with breast-conserving surgery and whole-breast irradiation after neoadjuvant chemotherapy. Breast Cancer Res Treat 194, 683–692 (2022). https://doi.org/10.1007/s10549-021-06500-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-021-06500-4