Abstract
Purpose
A large proportion of patients with breast cancer who had mastectomy had undergone breast reconstruction with implants or autologous flaps. However, only a few studies have compared the breast cancer outcomes between the implant-based reconstruction (IBR) and autologous flap reconstruction (AFR). In this study, we retrospectively compared the local recurrence rates, distant metastasis rates, and survival outcomes between immediate IBR and AFR.
Methods
A total of 1530 patients with primary breast cancer who underwent IBR or AFR with nipple-/skin-sparing mastectomy were included. Patients who underwent neoadjuvant systemic therapy were excluded from the study. After propensity score matching by age at diagnosis, T stage, N stage, molecular subtype, mastectomy type, adjuvant radiotherapy status, and follow-up period, 938 patients were 1:1 matched, comprising the well-balanced IBR and AFR groups. Locoregional recurrence-free survival (LRRFS), disease-free survival (DFS), distant metastasis-free survival (DMFS), and breast cancer-specific survival (BCSS) were compared between the matched groups.
Results
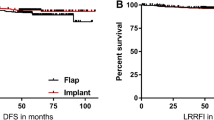
After matching, the median follow-up periods were 68 months and 71 months for the IBR and AFR groups, respectively. No significant differences were observed between the IBR and AFR groups regarding the local recurrence (7.2% vs. 5.1%; P = 0.175), regional recurrence (2.1% vs. 1.5%; P = 0.463), or distant metastasis (3.2% vs. 3.2%; P = 1.000) rates. Moreover, no significant difference was observed between the IBR and AFR groups in the LRRFS (hazard ratio, 0.691; 95% CI, 0.433–1.102; P = 0.118), DFS (hazard ratio, 0.709; 95% CI, 0.468–1.076; P = 0.104), DMFS (hazard ratio, 1.006; 95% CI, 0.491–2.059; P = 0.987), or BCSS (hazard ratio, 0.445; 95% CI, 0.111–1.786; P = 0.659).
Conclusion
In this propensity score-matched analysis of oncologic outcomes in patients with primary breast cancer who underwent immediate breast reconstruction with nipple-/skin-sparing mastectomy, no significant differences were observed between the IBR and AFR groups.

Similar content being viewed by others
References
DeSantis CE, Ma J, Gaudet MM, Newman LA, Miller KD, Goding Sauer A et al (2019) Breast cancer statistics, 2019. CA Cancer J Clin 69:438–451
Kang SY, Kim YS, Kim Z, Kim HY, Kim HJ, Park S et al (2020) Breast cancer statistics in Korea in 2017: data from a breast cancer registry. J Breast Cancer 23:115–128
Rosenberg SM, Dominici LS, Gelber S, Poorvu PD, Ruddy KJ, Wong JS et al (2020) Association of breast cancer surgery with quality of life and psychosocial well-being in young breast cancer survivors. JAMA Surg 155:1035–1042
Eltahir Y, Werners L, Dreise MM, van Emmichoven IAZ, Jansen L, Werker PMN et al (2013) Quality-of-life outcomes between mastectomy alone and breast reconstruction: comparison of patient-reported BREAST-Q and other health-related quality-of-life measures. Plast Reconstr Surg 132:201e–209e
Ueda S, Tamaki Y, Yano K, Okishiro N, Yanagisawa T, Imasato M et al (2008) Cosmetic outcome and patient satisfaction after skin-sparing mastectomy for breast cancer with immediate reconstruction of the breast. Surgery 143:414–425
Galimberti V, Vicini E, Corso G, Morigi C, Fontana S, Sacchini V et al (2017) Nipple-sparing and skin-sparing mastectomy: review of aims, oncological safety and contraindications. Breast 34(Suppl 1):S82–S84
Wong SM, Chun YS, Sagara Y, Golshan M, Erdmann-Sager J (2019) National patterns of breast reconstruction and nipple-sparing mastectomy for breast cancer, 2005–2015. Ann Surg Oncol 26:3194–3203
Eriksen C, Frisell J, Wickman M, Lidbrink E, Krawiec K, Sandelin K (2011) Immediate reconstruction with implants in women with invasive breast cancer does not affect oncological safety in a matched cohort study. Breast Cancer Res Treat 127:439–446
McCarthy CM, Pusic AL, Sclafani L, Buchanan C, Fey JV, Disa JJ et al (2008) Breast cancer recurrence following prosthetic, postmastectomy reconstruction: incidence, detection, and treatment. Plast Reconstr Surg 121:381–388
Lee SB, Lee JW, Kim HJ, Ko BS, Son BH, Eom JS et al (2018) Long-term outcomes of patients with breast cancer after nipple-sparing mastectomy/skin-sparing mastectomy followed by immediate transverse rectus abdominis musculocutaneous flap reconstruction: comparison with conventional mastectomy in a single center study. Medicine (Baltimore) 97:e0680
Adam H, Docherty Skogh AC, Edsander Nord A, Schultz I, Gahm J, Hall P et al (2018) Risk of recurrence and death in patients with breast cancer after delayed deep inferior epigastric perforator flap reconstruction. Br J Surg 105:1435–1445
Geers J, Wildiers H, Van Calster K, Laenen A, Floris G, Vandevoort M et al (2018) Oncological safety of autologous breast reconstruction after mastectomy for invasive breast cancer. BMC Cancer 18:994
Ha JH, Hong KY, Lee HB, Moon HG, Han W, Noh DY et al (2020) Oncologic outcomes after immediate breast reconstruction following mastectomy: comparison of implant and flap using propensity score matching. BMC Cancer 20:78
Leberfinger AN, Behar BJ, Williams NC, Rakszawski KL, Potochny JD, Mackay DR et al (2017) Breast implant-associated anaplastic large cell lymphoma: a systematic review. JAMA Surg 152:1161–1168
de Boer M, van Leeuwen FE, Hauptmann M, Overbeek LIH, de Boer JP, Hijmering NJ et al (2018) Breast implants and the risk of anaplastic large-cell lymphoma in the breast. JAMA Oncol 4:335–341
Nelson JA, Dabic S, Mehrara BJ, Cordeiro PG, Disa JJ, Pusic AL et al (2020) Breast implant-associated anaplastic large cell lymphoma incidence: determining an accurate risk. Ann Surg 272:403–409
DeCoster RC, Lynch EB, Bonaroti AR, Webster JM, Butterfield TA, Evers BM et al (2020) Breast implant-associated anaplastic large cell lymphoma: an evidence-based systematic review. Ann Surg 273:449–458
Jagsi R, Jiang J, Momoh AO, Alderman A, Giordano SH, Buchholz TA et al (2014) Trends and variation in use of breast reconstruction in patients with breast cancer undergoing mastectomy in the United States. J Clin Oncol 32:919–926
Song WJ, Kang SG, Kim EK, Song SY, Lee JS, Lee JH et al (2020) Current status of and trends in post-mastectomy breast reconstruction in Korea. Arch Plast Surg 47:118–125
Santosa KB, Qi J, Kim HM, Hamill JB, Wilkins EG, Pusic AL (2018) Long-term patient-reported outcomes in postmastectomy breast reconstruction. JAMA Surg 153:891–899
Pusic AL, Matros E, Fine N, Buchel E, Gordillo GM, Hamill JB et al (2017) Patient-reported outcomes 1 year after immediate breast reconstruction: results of the mastectomy reconstruction outcomes consortium study. J Clin Oncol 35:2499–2506
Nelson JA, Allen RJ Jr, Polanco T, Shamsunder M, Patel AR, McCarthy CM et al (2019) Long-term patient-reported outcomes following postmastectomy breast reconstruction: an 8-year examination of 3268 patients. Ann Surg 270:473–483
Weichman KE, Broer PN, Thanik VD, Wilson SC, Tanna N, Levine JP et al (2015) Patient-reported satisfaction and quality of life following breast reconstruction in thin patients: a comparison between microsurgical and prosthetic implant recipients. Plast Reconstr Surg 136:213–220
Bennett KG, Qi J, Kim HM, Hamill JB, Pusic AL, Wilkins EG (2018) Comparison of 2-year complication rates among common techniques for postmastectomy breast reconstruction. JAMA Surg 153:901–908
Isern AE, Manjer J, Malina J, Loman N, Mårtensson T, Bofin A et al (2011) Risk of recurrence following delayed large flap reconstruction after mastectomy for breast cancer. Br J Surg 98:659–666
Lee KT, Kim S, Jeon BJ, Pyon JK, Mun GH, Ryu JM et al (2020) Association of the implant surface texture used in reconstruction with breast cancer recurrence. JAMA Surg 155:1132–1140
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
This study was approved by the institutional review board of Asan Medical Center, Seoul, Korea (No. 20201793). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Because of the retrospective nature of the study, the requirement for informed consent was waived, and the study was conducted with the exemption of consent under IRB deliberation as it used a platform that offers unidentified clinical information for research purposes.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wu, ZY., Han, J., Kim, H.J. et al. Breast cancer outcomes following immediate breast reconstruction with implants versus autologous flaps: a propensity score-matched study. Breast Cancer Res Treat 191, 365–373 (2022). https://doi.org/10.1007/s10549-021-06350-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-021-06350-0