Abstract
Introduction
Breast cancer is the most common cancer in women worldwide. The number of childbearing-age women diagnosed with early breast cancer (eBC) is increasing, raising questions over their subsequent fertility.
Purpose
The main objective of this study was therefore to assess, in a cohort of eBC patients with pregnancy desire, the rate of live births achieved spontaneously or by assisted reproductive technology.
Methods
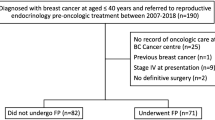
We conducted an observational, descriptive, retrospective study including patients aged 18–40, treated for eBC at the Institut de Cancérologie de l’Ouest (ICO) Pays de Loire between July 2010 and July 2016, with pregnancy desire. The primary outcome was the rate of live births. Secondary outcomes were overall survival, disease-free survival, time to conception, and spontaneous or assisted pregnancy rate.
Results
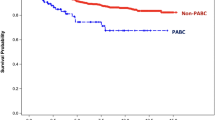
61 patients were included, with a live birth rate of 19.7% (12/61). We observed no recurrence or death in women with a pregnancy. Pregnancy started with a median time of 36.4 months after the end of treatment (4.1–51.3 months). All pregnancies in this cohort were achieved spontaneously.
Conclusion
The results of our cohort are consistent with previous results showing that spontaneous pregnancy remains possible after treatment for eBC without increasing the risk of recurrence or death.



Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Defossez G, Le Guyader-Peyrou S, Uhry Z, Grosclaude P, Colonna M, Dantony E, et al (2019) Estimations nationales de l’incidence et de la mortalité par cancer en France métropolitaine entre 1990 et 2018. Tumeurs solides. Saint-Maurice (Fra) : Santé publique France 1: 372. Available at https://www.ecancer.fr/.
Oktay K, Harvey BE, Loren AW (2018) Fertility Preservation in Patients With Cancer: ASCO clinical practice guideline update summary. J Oncol pract 14(6):381–385
Paluch-Shimon S, Cardoso F, Partridge AH, Abulkhair O, Azim HA, Bianchi-Micheli G et al (2020) ESO–ESMO 4th International consensus guidelines for breast cancer in young women (BCY4). Ann Oncol 31(6):674–696
Levine J, Canada A, Stern CJ (2010) Fertility preservation in adolescents and young adults with cancer. J Clin Oncol 28(32):4831–4841
Torino F, Barnabei A, De Vecchis L, Sini V, Schittulli F, Marchetti P et al (2014) Chemotherapy-induced ovarian toxicity in patients affected by endocrine-responsive early breast cancer. Crit Rev Oncol Hematol 89(1):27–42
Margulies AL, Selleret L, Zilberman S, Nagarra IT, Chopier J, Gligorov J et al (2015) Pregnancy after cancer: for whom and when? Bull Cancer 102(5):463–469
Helewa M, Lévesque P, Provencher D, Lea RH, Rosolowich V, Shapiro HM et al (2002) Breast cancer, pregnancy, and breastfeeding. J Obstet Gynaecol Can 24(2):164–180
Rodgers RJ, Reid GD, Koch J, Deans R, Ledger WL, Friedlander M et al (2017) The safety and efficacy of controlled ovarian hyperstimulation for fertility preservation in women with early breast cancer: a systematic review. Hum Reprod 32(5):1033–1045
Azim AA, Costantini-Ferrando M, Oktay K (2008) Safety of fertility preservation by ovarian stimulation with letrozole and gonadotropins in patients with breast cancer: a prospective controlled study. J Clin Oncol 26(16):2630–2635
Oktay K, Buyuk E, Libertella N, Akar M, Rosenwaks Z (2005) Fertility preservation in breast cancer patients: a prospective controlled comparison of ovarian stimulation with tamoxifen and letrozole for embryo cryopreservation. J Clin Oncol 23(19):4347–4353
Meirow D, Raanani H, Maman E, Paluch-Shimon S, Shapira M, Cohen Y et al (2014) Tamoxifen co-administration during controlled ovarian hyperstimulation for in vitro fertilization in breast cancer patients increases the safety of fertility-preservation treatment strategies. Fertil Steril 102(2):488-495.e3
Goldrat O, Kroman N, Peccatori FA, Cordoba O, Pistilli B, Lidegaard O et al (2015) Pregnancy following breast cancer using assisted reproduction and its effect on long-term outcome. Eur J Cancer 51(12):1490–1496
Letourneau JM, Wald K, Sinha N, Juarez-Hernandez F, Harris E, Cedars MI et al (2020) Fertility preservation before breast cancer treatment appears unlikely to affect disease-free survival at a median follow-up of 43 months after fertility-preservation consultation. Cancer 126(3):487–495
Arecco L, Perachino M, Damassi A, Latocca MM, Soldato D, Vallome G et al (2020) Burning Questions in the Oncofertility Counseling of Young Breast Cancer Patients. Breast Cancer Basic Clinic Res 14:1178223420954179
Ives A, Saunders C, Bulsara M, Semmens J (2007) Pregnancy after breast cancer: population-based study. BMJ 334(7586):194
Partridge AH, Gelber S, Peppercorn J, Ginsburg E, Sampson E, Rosenberg R et al (2008) Fertility and Menopausal Outcomes in Young Breast Cancer Survivors. Clin Breast Cancer 8(1):65–69
Hamy A-S, Porcher R, Eskenazi S, Cuvier C, Giacchetti S, Coussy F et al (2016) Anti-Müllerian hormone in breast cancer patients treated with chemotherapy: a retrospective evaluation of subsequent pregnancies. Reprod Biomed Online 32(3):299–307
Gerstl B, Sullivan E, Ives A, Saunders C, Wand H, Anazodo A (2018) Pregnancy outcomes after a breast cancer diagnosis: a systematic review and meta-analysis. Clin Breast Cancer 18(1):e79-88
Valachis A, Tsali L, Pesce LL, Polyzos NP, Dimitriadis C, Tsalis K et al (2010) Safety of pregnancy after primary breast carcinoma in young women: a meta-analysis to overcome bias of healthy mother effect studies. Obstet Gynecol Surv 65(12):786–793
Azim HA, Santoro L, Pavlidis N, Gelber S, Kroman N, Azim H et al (2011) Safety of pregnancy following breast cancer diagnosis: a meta-analysis of 14 studies. Eur J Cancer 47(1):74–83
Kopeika J, Bhaduri M, Kugadas A, Reddy N, Shewbridge A, Mukherji D et al (2019) Planned and unplanned pregnancies in breast cancer survivors. Breast 46:75–80
Assogba ELF, Kamga AM, Costaz H, Jankowski C, Dumas A, Roignot P et al (2020) What are young women living conditions after breast cancer? health-related quality of life, sexual and fertility issues, professional reinsertion. Cancers (Basel) 12(6):1564
Assi HI, Kakati RT, Attieh RM, Khoury J, Sukhon F, Berro J et al (2020) Fertility in breast cancer survivors in the middle east: a retrospective study. Breast 52:58–63
Blakely LJ, Buzdar AU, Lozada JA, Shullaih SA, Hoy E, Smith TL et al (2004) Effects of pregnancy after treatment for breast carcinoma on survival and risk of recurrence. Cancer 100(3):465–469
Largillier R, Savignoni A, Gligorov J, Chollet P, Guilhaume M-N, Spielmann M et al (2009) Prognostic role of pregnancy occurring before or after treatment of early breast cancer patients aged <35 years: a GET(N)A Working Group analysis. Cancer 115(22):5155–5165
Gelber S, Coates AS, Goldhirsch A, Castiglione-Gertsch M, Marini G, Lindtner J et al (2001) Effect of pregnancy on overall survival after the diagnosis of early-stage breast cancer. J Clin Oncol 19(6):1671–1675
Mueller BA, Simon MS, Deapen D, Kamineni A, Malone KE, Daling JR (2003) Childbearing and survival after breast carcinoma in young women. Cancer 98(6):1131–1140
Kroman N, Jensen M-B, Wohlfahrt J, Ejlertsen B (2008) Pregnancy after treatment of breast cancer—a population-based study on behalf of Danish Breast Cancer Cooperative Group. Acta Oncol 47(4):545–549
Azim HAJ, Kroman N, Paesmans M, Gelber S, Rotmensz N, Ameye L et al (2013) Prognostic impact of pregnancy after breast cancer according to estrogen receptor status: a multicenter retrospective study. J Clin Oncol 31(1):73–79
Velentgas P, Daling JR, Malone KE, Weiss NS, Williams MA, Self SG et al (1999) Pregnancy after breast carcinoma: outcomes and influence on mortality. Cancer 85(11):2424–2432
Hartman EK, Eslick GD (2016) The prognosis of women diagnosed with breast cancer before, during and after pregnancy: a meta-analysis. Breast Cancer Res Treat 160(2):347–360
Lambertini M, Kroman N, Ameye L, Cordoba O, Pinto A, Benedetti G et al (2018) Long-term safety of pregnancy following breast cancer according to estrogen receptor status. J Natl Cancer Inst 110(4):426–429
Dignam JJ, Dukic V, Anderson SJ, Mamounas EP, Wickerham DL, Wolmark N (2009) Hazard of recurrence and adjuvant treatment effects over time in lymph node-negative breast cancer. Breast Cancer Res Treat 116(3):595–602
Douay-Hauser N, Ngo C, Bats AS, Bensaïd C, Seror J, Médioni J et al (2014) (2014) Désir de grossesse après cancer du sein: que répondre au couple ? La Lettre du Cancérologue 23:426–429
Davies C, Pan H, Godwin J, Gray R, Arriagada R, Raina V et al (2013) Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet 381(9869):805–816
Lambertini M, Peccatori FA, Demeestere I, Amant F, Wyns C, Stukenborg J-B et al (2020) Fertility preservation and post-treatment pregnancies in post-pubertal cancer patients: ESMO Clinical Practice Guidelines. Annals Oncol Offic J Eur Soc Med Oncol 31(12):1664–1678
Elies A, Salakos E, Rouzier R (2019) Desire for pregnancy and breast cancer. Bull Cancer. 106(12S1):S53–S59
Rosenberg E, Fredriksson A, Einbeigi Z, Bergh C, Strandell A (2019) No increased risk of relapse of breast cancer for women who give birth after assisted conception. Human Reprod Open 2019(4):039
Luke B, Brown MB, Missmer SA, Spector LG, Leach RE, Williams M et al (2016) Assisted reproductive technology use and outcomes among women with a history of cancer. Human Reprod (Oxford, England) 31(1):183–189
Hashimoto T, Nakamura Y, Obata R, Doshida M, Toya M, Takeuchi T et al (2017) Effects of fertility preservation in patients with breast cancer: a retrospective two-centers study. Reprod Med Biol 16(4):374–379
Francis PA, Regan MM, Fleming GF, Láng I, Ciruelos E, Bellet M et al (2015) Adjuvant ovarian suppression in premenopausal breast cancer. N Engl J Med 372(5):436–446
Funding
During this study, no financial support was received.
Author information
Authors and Affiliations
Contributions
BS provided idea and concept and participated in control and supervision; BS and CL involved in design; CL performed data collection and processing, literature review, and writing the article; VS contributed to analysis and interpretation; AP and BS involved in critical review; and AP performed English correction:.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures in this human-subject study were performed in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The protocol was accepted by the Ethics Committee of Angers University Hospital Center on 12/16/2019.
Informed consent
The data were collected anonymously from information contained in patients’ electronic medical records; surviving patients were informed of the use of their data by post. To oppose it, they were required to write to the Data Protection Officer within one month. Informed consent was not obtained, which was in accordance with ethical approval from the Ethics Committee of Angers University Hospital Center (file number 2019/114).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Leproux, C., Seegers, V., Patsouris, A. et al. Success and risks of pregnancy after breast cancer. Breast Cancer Res Treat 188, 593–600 (2021). https://doi.org/10.1007/s10549-021-06232-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-021-06232-5