Abstract
Purpose
We compared oncologic outcomes between breast cancer patients who underwent immediate implant-based breast reconstruction (IBBR) and those who underwent autologous flap reconstruction (AFR) after neoadjuvant chemotherapy (NACT).
Methods
The study group comprised 536 patients with primary breast cancer who underwent NACT followed by immediate IBBR or AFR. After propensity score matching, 138 patients in the IBBR group and 276 patients in the AFR group were selected for comparisons of locoregional recurrence-free survival (LRRFS), disease-free survival (DFS), distant metastasis-free survival (DMFS), and breast cancer-specific survival (BCSS).
Results
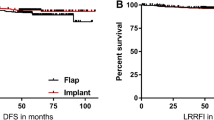
No significant differences were observed between the matched groups in locoregional recurrence rates (IBBR vs. AFR: 12.3% vs. 12%; P = 0.915) and distant metastasis (13% vs. 17%; P = 0.293). There was also no significant difference between the groups in LRRFS (P = 0.956), DFS (P = 0.606), DMFS (P = 0.283), or BCSS (P = 0.121). The 5- and 10-year LRRFS rates were 87.6% and 85.9% in the IBBR group, and 87.7% and 86.1% in the AFR group; the 5- and 10-year DFS rates were 79% and 77.5% in the IBBR group, and 77% and 75% in the AFR group; the 5- and 10-year DMFS rates were 85.9% and 85.9% in the IBBR group, and 83.2% and 81.8% in the AFR group; and the 5- and 10-year BCSS rates were 97.8% and 91.3% in the IBBR group, and 91.8% and 86% in the AFR group, respectively.
Conclusions
In this propensity score-matched analysis of oncologic outcomes in breast cancer patients who underwent immediate reconstruction after NACT, no significant differences were observed between the IBBR and AFR groups.

Similar content being viewed by others
References
Bailey CR, Ogbuagu O, Baltodano PA et al (2017) Quality-of-life outcomes improve with nipple-sparing mastectomy and breast reconstruction. PlastReconstrSurg 140(2):219–226. https://doi.org/10.1097/PRS.0000000000003505
Romanoff A, Zabor EC, Stempel M, Sacchini V, Pusic A, Morrow M (2018) A comparison of patient-reported outcomes after nipple-sparing mastectomy and conventional mastectomy with reconstruction. Ann Surg Oncol 25(10):2909–2916. https://doi.org/10.1245/s10434-018-6585-4
Ueda S, Tamaki Y, Yano K et al (2008) Cosmetic outcome and patient satisfaction after skin-sparing mastectomy for breast cancer with immediate reconstruction of the breast. Surgery 143(3):414–425. https://doi.org/10.1016/j.surg.2007.10.006
Siotos C, Naska A, Bello RJ et al (2019) Survival and disease recurrence rates among breast cancer patients following mastectomy with or without breast reconstruction. PlastReconstrSurg 144(2):169e–177e. https://doi.org/10.1097/PRS.0000000000005798
Eriksen C, Frisell J, Wickman M, Lidbrink E, Krawiec K, Sandelin K (2011) Immediate reconstruction with implants in women with invasive breast cancer does not affect oncological safety in a matched cohort study. Breast Cancer Res Treat 127(2):439–446. https://doi.org/10.1007/s10549-011-1437-y
Lee SB, Lee JW, Kim HJ et al (2018) Long-term outcomes of patients with breast cancer after nipple-sparing mastectomy/skin-sparing mastectomy followed by immediate transverse rectus abdominis musculocutaneous flap reconstruction: comparison with conventional mastectomy in a single center study. Medicine (Baltimore) 97(18):e0680. https://doi.org/10.1097/MD.0000000000010680
Adam H, Bygdeson M, de Boniface J (2014) The oncological safety of nipple-sparing mastectomy—a Swedish matched cohort study. Eur J Surg Oncol 40(10):1209–1215. https://doi.org/10.1016/j.ejso.2014.07.037
Platt J, Baxter NN, McLaughlin J, Semple JL (2015) Does breast reconstruction after mastectomy for breast cancer affect overall survival? Long-term follow-up of a retrospective population-based cohort. PlastReconstrSurg 135(3):468e–476e. https://doi.org/10.1097/PRS.0000000000001054
Wengler CA, Valente SA, Al-Hilli Z et al (2017) Determinants of short and long term outcomes in patients undergoing immediate breast reconstruction following neoadjuvant chemotherapy. J Surg Oncol 116(7):797–802. https://doi.org/10.1002/jso.24741
Ryu JM, Park S, Paik HJ et al (2017) Oncologic safety of immediate breast reconstruction in breast cancer patients who underwent neoadjuvant chemotherapy: short-term outcomes of a matched case-control study. Clin Breast Cancer 17(3):204–210. https://doi.org/10.1016/j.clbc.2016.10.009
Vieira R, Ribeiro LM, Carrara GFA, Abrahão-Machado LF, Kerr LM, Nazário ACP (2019) Effectiveness and safety of implant-based breast reconstruction in locally advanced breast carcinoma: a matched case-control study. Breast Care (Basel) 14(4):200–210. https://doi.org/10.1159/000496429
Leberfinger AN, Behar BJ, Williams NC et al (2017) Breast implant-associated anaplastic large cell lymphoma: a systematic review. JAMASurg 152(12):1161–1168. https://doi.org/10.1001/jamasurg.2017.4026
Collett DJ, Rakhorst H, Lennox P, Magnusson M, Cooter R, Deva AK (2019) Current risk estimate of breast implant-associated anaplastic large cell lymphoma in textured breast implants. PlastReconstrSurg 143(3S A Review of Breast Implant-Associated Anaplastic Large Cell Lymphoma):30S-40S. https://doi.org/10.1097/PRS.0000000000005567
de Boer M, van Leeuwen FE, Hauptmann M et al (2018) Breast implants and the risk of anaplastic large-cell lymphoma in the breast. JAMA Oncol 4(3):335–341. https://doi.org/10.1001/jamaoncol.2017.4510
Peled AW, Wang F, Foster RD et al (2016) Expanding the indications for total skin-sparing mastectomy: is it safe for patients with locally advanced disease? Ann Surg Oncol 23(1):87–91. https://doi.org/10.1245/s10434-015-4734-6
Wong SM, Chun YS, Sagara Y, Golshan M, Erdmann-Sager J (2019) National patterns of breast reconstruction and nipple-sparing mastectomy for breast cancer, 2005–2015. Ann Surg Oncol 26(10):3194–3203. https://doi.org/10.1245/s10434-019-07554-x
Amin MB, Edge S, Greene F et al (2017) AJCC cancer staging manual, 8th edn. Springer, New York, NY
Bennett KG, Qi J, Kim HM, Hamill JB, Pusic AL, Wilkins EG (2018) Comparison of 2-year complication rates among common techniques for postmastectomy breast reconstruction. JAMASurg 153(10):901–908. https://doi.org/10.1001/jamasurg.2018.1687
Tsoi B, Ziolkowski NI, Thoma A, Campbell K, O’Reilly D, Goeree R (2014) Safety of tissue expander/implant versus autologous abdominal tissue breast reconstruction in postmastectomy breast cancer patients: a systematic review and meta-analysis. PlastReconstrSurg 133(2):234–249. https://doi.org/10.1097/01.prs.0000436847.94408.11
Santosa KB, Qi J, Kim HM, Hamill JB, Wilkins EG, Pusic AL (2018) Long-term patient-reported outcomes in postmastectomy breast reconstruction. JAMASurg 153(10):891–899. https://doi.org/10.1001/jamasurg.2018.1677
Eltahir Y, Krabbe-Timmerman IS, Sadok N, Werker PMN, de Bock GH (2020) Outcome of quality of life for women undergoing autologous versus alloplastic breast reconstruction following mastectomy: a systematic review and meta-analysis. PlastReconstrSurg 145(5):1109–1123. https://doi.org/10.1097/PRS.0000000000006720
Toyserkani NM, Jørgensen MG, Tabatabaeifar S, Damsgaard T, Sørensen JA (2020) Autologous versus implant-based breast reconstruction: a systematic review and meta-analysis of Breast-Q patient-reported outcomes. J PlastReconstrAesthetSurg 73(2):278–285. https://doi.org/10.1016/j.bjps.2019.09.040
Ha JH, Hong KY, Lee HB et al (2020) Oncologic outcomes after immediate breast reconstruction following mastectomy: comparison of implant and flap using propensity score matching. BMC Cancer 20(1):78. https://doi.org/10.1186/s12885-020-6568-2
Cortazar P, Zhang L, Untch M et al (2014) Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet 384(9938):164–172. https://doi.org/10.1016/S0140-6736(13)62422-8
Lee KT, Kim S, Jeon BJ et al (2020) Association of the implant surface texture used in reconstruction with breast cancer recurrence. JAMASurg 7:e204124. https://doi.org/10.1001/jamasurg.2020.4124
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Ethical approval
This study was approved by the institutional review board of Asan Medical Center, Seoul, Korea (No. 2020-0712). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Because of the retrospective nature of the study, the requirement for informed consent was waived, and the study was conducted with the exemption of consent under IRB deliberation as it used a platform that offers unidentified clinical information for research purposes.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wu, ZY., Han, H.H., Kim, H.J. et al. A propensity score-matched comparison of recurrence outcomes after immediate implant vs autologous flap reconstruction in patients receiving neoadjuvant chemotherapy for breast cancer. Breast Cancer Res Treat 187, 417–425 (2021). https://doi.org/10.1007/s10549-021-06114-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-021-06114-w