Abstract
Background
Myosteatosis (intramuscular adiposity) is predictive of chemotherapy toxicity in women undergoing adjuvant chemotherapy for breast cancer (BC). We evaluated a novel, user-friendly and cost-effective technique utilizing a Picture Archiving and Communication Systems (PACS) tool that is readily available in the electronic medical record (EMR), using skeletal muscle density (SMD) to detect myosteatosis and then compared PACS results with those derived from widely used body composition software (SliceOMatic, QC, Canada).
Methods
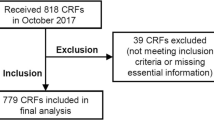
Using retrospective data from a sample of women with early BC (Stage I-III) who had CT scan and received chemotherapy. Pearson correlation coefficients were used to compare SliceOMatic with PACS results. Associations of PACS results with chemotherapy-related adverse events were evaluated using multivariable (MV) log-binomial models adjusted for age, race, BMI, anthracycline-based therapy, and number of comorbidities.
Results
In 338 patients, mean age was 51, 32% were non-white, and 40% had obesity (BMI ≥ 30 kg/m2). Correlation of SMD using SliceOMatic whole muscle measurements with PACS psoas muscle was 0.76 (p < .0001) and with PACS erector spinae muscle 0.91 (p < .0001). Using PACS psoas muscle, myosteatosis was associated with any adverse event [RR 1.66, CI 1.22–2.26 (p < .0001)], dose reduction [RR 1.63, CI 1.01–2.65 (p = .05)], and early treatment discontinuation [RR 2.14, CI 1.10–4.14 (p = 0.03)]. Using PACS erector spinae muscle, myosteatosis was associated any adverse event [RR 1.59, CI 1.11–2.27 (p = 0.01)] and dose reduction [RR 1.91, CI 1.07–3.42 (p = .03)].
Conclusion and relevance
Skeletal muscle density measures using PACS correlated strongly with SliceOMatic results and both are similarly predictive of chemotherapy-related adverse events



Similar content being viewed by others
Abbreviations
- CT:
-
Computed tomography
- DICOM:
-
Digital imaging and communications in medicine
- SMD:
-
Skeletal muscle density
- HU:
-
Hounsfield units
- PACS:
-
Picture Archiving and Communication System
- EMR:
-
Electronic medical record
- EBC:
-
Early breast cancer
- ROI:
-
Region of interest
References
Sueda T, Takahasi H, Nishimura J et al (2018) Impact of low muscularity and myosteatosis on long-term outcome after curative colorectal cancer surgery: a propensity score-matched analysis. Dis Colon Rectum 61(3):364–374
Caan BJ, Cespedes Feliciano EM, Prado CM et al (2018) Association of muscle and adiposity measured by computed tomography with survival in patients with nonmetastatic breast cancer. JAMA Oncol 4(6):798–804
Aleixo GFP, Shachar SS, Deal AM et al (2020) The association of body composition parameters and adverse events in women receiving chemotherapy for early breast cancer. Breast Cancer Res Treat. https://doi.org/10.1007/s10549-020-05731-1
Cespedes Feliciano EM, Chen WY, Lee V et al (2019) Body composition, adherence to anthracycline and taxane-based chemotherapy, and survival after nonmetastatic breast cancer. JAMA Oncol. https://doi.org/10.1001/jamaoncol.2019.4668
Cespedes Feliciano EM, Popuri K, Cobzas D et al (2020) Evaluation of automated computed tomography segmentation to assess body composition and mortality associations in cancer patients. J Cachexia Sarcopenia Muscle. https://doi.org/10.1002/jcsm.12573
Caffrey C, Cairns C, Rome V (2020) Trends in electronic health record use among residential care communities: United States, 2012, 2014, and 2016. Natl Health Stat Rep 140:1–10
Kalafateli M, Karatzas A, Tsiaoussis G et al (2018) Muscle fat infiltration assessed by total psoas density on computed tomography predicts mortality in cirrhosis. Ann Gastroenterol 31(4):491–498
Herrod PJJ, Boyd-Carson H, Doleman B et al (2019) Quick and simple; psoas density measurement is an independent predictor of anastomotic leak and other complications after colorectal resection. Tech Coloproctol 23(2):129–134
Rollins KE, Gopinath A, Awwad A, Macdonald IA, Lobo DN (2019) Computed tomography-based psoas skeletal muscle area and radiodensity are poor sentinels for whole L3 skeletal muscle values. Clin Nutr. https://doi.org/10.1016/j.clnu.2019.10.003
Amini B, Boyle SP, Boutin RD, Lenchik L (2019) Approaches to assessment of muscle mass and myosteatosis on computed tomography: a systematic review. J Gerontol A 74(10):1671–1678
Kroenke CH, Prado CM, Meyerhardt JA et al (2018) Muscle radiodensity and mortality in patients with colorectal cancer. Cancer 124(14):3008–3015
Overholser BR, Sowinski KM (2008) Biostatistics primer: part 2. Nutr Clin Pract 23(1):76–84
Kaminska M, Ciszewski T, Lopacka-Szatan K, Miotla P, Staroslawska E (2015) Breast cancer risk factors. Prz Menop 14(3):196–202
Klepin HD, Pitcher BN, Ballman KV et al (2014) Comorbidity, chemotherapy toxicity, and outcomes among older women receiving adjuvant chemotherapy for breast cancer on a clinical trial: CALGB 49907 and CALGB 361004 (alliance). J Oncol Pract 10(5):e285-292
Aleixo GFP, Shachar SS, Nyrop KA, Muss HB, Malpica L, Williams GR (2020) Myosteatosis and prognosis in cancer: systematic review and meta-analysis. Crit Rev Oncol Hematol 145:102839
Van Rijssen LB, van Huijgevoort NC, Coelen RJ et al (2017) Skeletal muscle quality is associated with worse survival after pancreatoduodenectomy for periampullary, nonpancreatic cancer. Ann Surg Oncol 24(1):272–280
van Vugt J, Alferink LJ, Büttner S, Metselaar H, IJzermans J (2018) Reply to: “May sarcopenia and/or hepatic encephalopathy improve the predictivity of model for end-stage liver disease?” and “has the time come for using MELD-Sarcopenia score?” J Hepatol 68(6):1326
Martin L, Birdsell L, Macdonald N et al (2013) Cancer cachexia in the age of obesity: skeletal muscle depletion is a powerful prognostic factor, independent of body mass index. J Clin Oncol 31(12):1539–1547
Cespedes Feliciano EM, Chen WY, Bradshaw PT et al (2019) Adipose tissue distribution and cardiovascular disease risk among breast cancer survivors. J Clin Oncol 37:2528
Abdel-Rahman O (2019) Outcomes of early-stage breast cancer patients treated with sequential anthracyclines-taxanes in relationship to relative dosing intensity: a secondary analysis of a randomized controlled trial. Clin Transl Oncol 21(2):239–245
Yamashita M, Kamiya K, Matsunaga A et al (2017) Prognostic value of psoas muscle area and density in patients who undergo cardiovascular surgery. Can J Cardiol 33(12):1652–1659
Lo WD, Evans DC, Yoo T (2018) Computed tomography-measured psoas density predicts outcomes after enterocutaneous fistula repair. JPEN J Parenter Enter Nutr 42(1):176–185
Valenzuela PL, Maffiuletti NA, Tringali G, De Col A, Sartorio A (2020) Obesity-associated poor muscle quality: prevalence and association with age, sex, and body mass index. BMC Musculoskelet Disord 21(1):200
Acknowledgements
We greatly appreciate the active support of oncology clinicians and their research staff at multiple sites and, most importantly, the breast cancer patients participating in our study. We thank Tucker Brenizer, Shanah R. Kirk, and Amy Garrett for their commitment to study implementation best practices.
Funding
This study was supported by the Breast Cancer Research Foundation (New York), UNC Lineberger Comprehensive Cancer Center/University Cancer Research Fund, and Kay Yow Fund (Raleigh, North Carolina).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individuals participants in this study and approved by the IRB of the University of North Carolina at Chapel Hill.
Research involving human and animal participants
This article does not contain any animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Aleixo, G.F.P., Yu, H., Chen, Y.T. et al. Myosteatosis evaluation using erector spinae and psoas muscles to predict adverse events during adjuvant chemotherapy for breast cancer. Breast Cancer Res Treat 186, 487–495 (2021). https://doi.org/10.1007/s10549-020-06061-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-06061-y