Abstract
Purpose
Public safety net hospitals (SNH) serve a disparate patient population; however, little is known about long-term oncologic outcomes of patients receiving care at these facilities. This study is the first to examine overall survival (OS) and the initiation of treatment in breast cancer patients treated at a SNH.
Methods
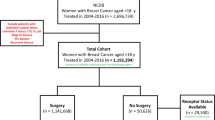
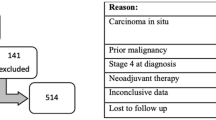
Patients presenting to a SNH with stage I-IV breast cancer from 2005 to 2017 were identified from the local tumor registry. The hospital has a weekly breast tumor board and a multidisciplinary approach to breast cancer care. Kaplan-Meier survival analysis was performed to identify patient, tumor, and treatment characteristics associated with OS. Factors with a p < 0.1 were included in the Cox proportional hazards model.
Results
2709 breast cancer patients were evaluated from 2005 to 2017. The patient demographics, tumor characteristics, and treatments received were analyzed. Five-year OS was 78.4% (93.9%, 87.4%, 70.9%, and 23.5% for stages I, II, III, and IV, respectively). On multivariable analysis, higher stage, age > 70 years, higher grade, and non-Hispanic ethnicity were associated with worse OS. Patients receiving surgery (HR = 0.33, p < 0.0001), chemotherapy (HR = 0.71, p = 0.006), and endocrine therapy (HR = 0.61, p < 0.0001) had better OS compared to those who did not receive these treatments.
Conclusion
Despite serving a vulnerable minority population that is largely poor, uninsured, and presenting with more advanced disease, OS at our SNH approaches national averages. This novel finding indicates that in the setting of multidisciplinary cancer care and with appropriate initiation of treatment, SNHs can overcome socioeconomic barriers to achieve equitable outcomes in breast cancer care.




Similar content being viewed by others
References
Genther DJ, Gourin CG (2012) The effect of hospital safety-net burden status on short-term outcomes and cost of care after head and neck cancer surgery. Arch Otolaryngol Head Neck Surg 138(11):1015–1022
Mouch CA et al (2014) The quality of surgical care in safety net hospitals: a systematic review. Surgery 155(5):826–838
Hoehn RS et al (2016) Effect of hospital safety-net burden on cost and outcomes after surgery. JAMA Surg 151(2):120–128
Lewin ME (2000) A.S., America's health care safety-net: intact but endangered, M.C. committee on the changing market, and the future viability of safety-net providers; Institute of Medicine, editor. National Academy Press, Washington, DC
Bazzoli GJ et al (2012) The effects of safety net hospital closures and conversions on patient travel distance to hospital services. Health Serv Res 47(1 Pt 1):129–150
Mobley L, Kuo TM, Bazzoli GJ (2011) Erosion in the healthcare safety net: impacts on different population groups. Open Health Serv Policy J 4:1–14
Virgo KS et al (2011) Safety-net burden hospitals and likelihood of curative-intent surgery for non-small cell lung cancer. J Am Coll Surg 213(5):633–643
Bradley CJ et al (2008) Differences in breast cancer diagnosis and treatment: experiences of insured and uninsured women in a safety-net setting. Inquiry 45(3):323–339
Bradley CJ et al (2012) Surgery wait times and specialty services for insured and uninsured breast cancer patients: does hospital safety net status matter? Health Serv Res 47(2):677–697
McHugh M, Kang R, Hasnain-Wynia R (2009) Understanding the safety net: inpatient quality of care varies based on how one defines safety-net hospitals. Med Care Res Rev 66(5):590–605
Shields AE (2007) Trends in private insurance, Medicaid/state Children's health insurance program, and the health-care safety net: implications for asthma disparities. Chest 132(5 Suppl):818s–830s
Halpern MT et al (2008) Association of insurance status and ethnicity with cancer stage at diagnosis for 12 cancer sites: a retrospective analysis. Lancet Oncol 9(3):222–231
McLaughlin JM et al (2012) Effect on survival of longer intervals between confirmed diagnosis and treatment initiation among low-income women with breast cancer. J Clin Oncol 30(36):4493–4500
Neugut AI et al (2012) The breast Cancer quality of care study (BQUAL): a multi-center study to determine causes for noncompliance with breast cancer adjuvant therapy. Breast J 18(3):203–213
Elmore JG et al (2005) Racial inequities in the timing of breast cancer detection, diagnosis, and initiation of treatment. Med Care 43(2):141–148
Silber JH et al (2013) Characteristics associated with differences in survival among black and white women with breast cancer. Jama 310(4):389–397
Chagpar AB et al (2011) Primary tumor size, not race, determines outcomes in women with hormone-responsive breast cancer. Surgery 150(4):796–801
Hershman D et al (2005) Racial disparities in treatment and survival among women with early-stage breast cancer. J Clin Oncol 23(27):6639–6646
Gorin SS et al (2006) Delays in breast cancer diagnosis and treatment by racial/ethnic group. Arch Intern Med 166(20):2244–2252
Jackson Health System Website. (cited 2020 2/22/2020); Available from: https://jacksonhealth.org/
JMH Breast Health Center Website. 2/22/20]; Available from: https://jacksonhealth.org/jackson-memorial/radiology-breast-health-center
National Cancer Data Base Breast Cancer PUF. (2004-2015) American cancer society, Commission on cancer of the American college of surgeons
Ross JS et al (2007) Quality of care for acute myocardial infarction at urban safety-net hospitals. Health Aff (Millwood) 26(1):238–248
Bradley CJ, Given CW, Roberts C (2001) Disparities in cancer diagnosis and survival. Cancer 91(1):178–188
Bureau, U.C. 2010 Census Quick Facts. 2/24/2020]; Available from: https://www.census.gov/quickfacts/fact/table/US/RHI225218
Taplin SH et al (2015) Reviewing cancer care team effectiveness. J Oncol Pract 11(3):239–246
Fennell ML et al (2010) The organization of multidisciplinary care teams: modeling internal and external influences on cancer care quality. J Natl Cancer Inst Monogr 2010(40):72–80
Kesson EM et al (2012) Effects of multidisciplinary team working on breast cancer survival: retrospective, comparative, interventional cohort study of 13 722 women. Bmj 344:e2718
Ju M et al (2020) Multidisciplinary teams improve gastric Cancer treatment efficiency at a large safety net hospital. Ann Surg Oncol 27(3):645–650
Duininck G et al (2019) Optimizing cancer care for hepatocellular carcinoma at a safety-net hospital: the value of a multidisciplinary disease management team. J Surg Oncol 120(8):1365–1370
Noone AM, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). . SEER Cancer Statistics Review, 1975–2015, National Cancer Institute. . based on November 2017 SEER data submission, posted to the SEER web site, April 2018. [cited 2020; Available from: https://seer.cancer.gov/csr/1975_2015/
Parise CA, Caggiano V (2015) The influence of socioeconomic status on racial/ethnic disparities among the ER/PR/HER2 breast Cancer subtypes. J Cancer Epidemiol 2015:813456
Braithwaite D et al (2009) Hypertension is an independent predictor of survival disparity between African-American and white breast cancer patients. Int J Cancer 124(5):1213–1219
Tammemagi CM et al (2005) Comorbidity and survival disparities among black and white patients with breast cancer. Jama 294(14):1765–1772
Daly B, Olopade OI (2015) A perfect storm: how tumor biology, genomics, and health care delivery patterns collide to create a racial survival disparity in breast cancer and proposed interventions for change. CA Cancer J Clin 65(3):221–238
Fejerman L et al (2008) Genetic ancestry and risk of breast cancer among U.S. Latinas. Cancer Res 68(23):9723–9728
Dunning AM et al (2016) Breast cancer risk variants at 6q25 display different phenotype associations and regulate ESR1, RMND1 and CCDC170. Nat Genet 48(4):374–386
O'Brien KM et al (2010) Intrinsic breast tumor subtypes, race, and long-term survival in the Carolina breast Cancer study. Clin Cancer Res 16(24):6100–6110
Chlebowski RT et al (2005) Ethnicity and breast cancer: factors influencing differences in incidence and outcome. J Natl Cancer Inst 97(6):439–448
Joslyn SA, West MM (2000) Racial differences in breast carcinoma survival. Cancer 88(1):114–123
Li CI, Malone KE, Daling JR (2003) Differences in breast cancer stage, treatment, and survival by race and ethnicity. Arch Intern Med 163(1):49–56
Daly B et al (2017) Evaluation of the quality of adjuvant endocrine therapy delivery for breast Cancer Care in the United States. JAMA Oncol 3(7):928–935
Acknowledgements
The authors acknowledge support from the National Cancer Institute (NCI) of the National Institutes of Health (NIH) Award—1K12CA226330-01 (Alan Pollack, Neha Goel).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Kristin N. Kelly, Alexandra Hernandez, Sina Yadegarynia, Emily Ryon, Dido Franceschi, Eli Avisar, Erin N. Kobetz, Nipun Merchant, Susan Kesmodel, Neha Goel declares that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kelly, K.N., Hernandez, A., Yadegarynia, S. et al. Overcoming disparities: Multidisciplinary breast cancer care at a public safety net hospital. Breast Cancer Res Treat 187, 197–206 (2021). https://doi.org/10.1007/s10549-020-06044-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-06044-z