Abstract
Purpose
Many studies have revealed that statin therapy reduced mortality in cancer patients, especially in breast cancer, but the effect for second cancer was unclear. We, therefore, performed a comparable cohort study to determine the risk of second cancer in breast cancer patients with statin therapy.
Methods
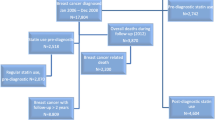
Using claims data from Taiwan’s National Health Insurance Program, this study enrolled newly diagnosed breast cancer patients from 2000 to 2007 with and without statin therapy as the statin (n = 1222) and nonstatin (n = 4888) cohorts, respectively. The nonstatin cohort was propensity score matched by cohort entry year, age, and randomly selected comorbidities. These two cohorts were followed up until the diagnosis of second cancer, death, or the end of 2011. Cox proportional hazard models were used to estimate the hazard ratios.
Results
The statin cohort had a lower incidence rate than the nonstatin cohort for second cancer (7.37 vs. 8.36 per 1000 person-years), although the difference was not significant (adjusted hazard ratio [aHR] 0.90, 95% confidence interval [CI] 0.65–1.26). Compared with the nonstatin cohort, the second cancer risk was significantly higher for patients taking pravastatin (aHR 2.71, 95% CI 1.19–6.19) but lower for those receiving multiple statin treatment (aHR 0.45, 95% CI 0.25–0.81) and combined lipophilic and hydrophilic type of statin (aHR 0.42, 95% CI 0.20–0.89). The risk was lower for patients receiving a cumulative defined daily dose (cDDD) of > 430 (aHR 0.41, 95% CI 0.19–0.86).
Conclusion
This study showed that there is little association between statin use and second cancer risk in breast cancer patients.





Similar content being viewed by others
Data availability
The NHIRD is held by the Taiwan Ministry of Health and Welfare. Any researcher interested in accessing the data set can submit an application form to the Ministry of Health and Welfare requesting access.
Abbreviations
- cDDD:
-
Cumulative defined daily dose
- CI:
-
Confidence interval
- ICD-9-CM:
-
International Classification of Disease, Ninth Revision, Clinical Modification
- NHIRD:
-
National Health Insurance Research Database
- RCIPD:
-
Registry of Catastrophic Illness Patient Database
- SHR:
-
Subdistribution hazard ratio
References
Lu YC, Lu CL, Chen YY, Chen PT, Lin MS, Chen W, Chen SC (2016) Trend of incidence of second primary malignancies following breast cancer in Taiwan: a 12-year Nationwide Cohort Study. Breast J 22:360–362. https://doi.org/10.1111/tbj.12582
Ho ML, Hsiao YH, Su SY, Chou MC, Liaw YP (2015) Mortality of breast cancer in Taiwan, 1971–2010: temporal changes and an age-period-cohort analysis. J Obstet Gynaecol 35:60–63. https://doi.org/10.3109/01443615.2014.935717
Molina-Montes E, Requena M, Sanchez-Cantalejo E, Fernandez MF, Arroyo-Morales M, Espin J, Arrebola JP, Sanchez MJ (2015) Risk of second cancers cancer after a first primary breast cancer: a systematic review and meta-analysis. Gynecol Oncol 136:158–171. https://doi.org/10.1016/j.ygyno.2014.10.029
Bonovas S, Filioussi K, Tsavaris N, Sitaras NM (2005) Use of statins and breast cancer: a meta-analysis of seven randomized clinical trials and nine observational studies. J Clin Oncol 23:8606–8612. https://doi.org/10.1200/JCO.2005.02.7045
Demierre MF, Higgins PD, Gruber SB, Hawk E, Lippman SM (2005) Statins and cancer prevention. Nat Rev Cancer 5:930–942. https://doi.org/10.1038/nrc1751
Sacks FM, Pfeffer MA, Moye LA, Rouleau JL, Rutherford JD, Cole TG, Brown L, Warnica JW, Arnold JM, Wun CC et al (1996) The effect of pravastatin on coronary events after myocardial infarction in patients with average cholesterol levels. Cholesterol and Recurrent Events Trial investigators. N Engl J Med 335:1001–1009. https://doi.org/10.1056/NEJM199610033351401
Almuti K, Rimawi R, Spevack D, Ostfeld RJ (2006) Effects of statins beyond lipid lowering: potential for clinical benefits. Int J Cardiol 109:7–15. https://doi.org/10.1016/j.ijcard.2005.05.056
Usui H, Shikata K, Matsuda M, Okada S, Ogawa D, Yamashita T, Hida K, Satoh M, Wada J, Makino H (2003) HMG-CoA reductase inhibitor ameliorates diabetic nephropathy by its pleiotropic effects in rats. Nephrol Dial Transplant 18:265–272. https://doi.org/10.1093/ndt/18.2.265
Fujimoto M, Higuchi T, Hosomi K, Takada M (2015) Association between statin use and cancer: data mining of a spontaneous reporting database and a claims database. Int J Med Sci 12:223–233. https://doi.org/10.7150/ijms.10656
Jick H, Zornberg GL, Jick SS, Seshadri S, Drachman DA (2000) Statins and the risk of dementia. Lancet 356:1627–1631. https://doi.org/10.1016/s0140-6736(00)03155-x
Meier CR, Schlienger RG, Kraenzlin ME, Schlegel B, Jick H (2000) HMG-CoA reductase inhibitors and the risk of fractures. JAMA 283:3205–3210. https://doi.org/10.1001/jama.283.24.3205
Clendening JW, Penn LZ (2012) Targeting tumor cell metabolism with statins. Oncogene 31:4967–4978. https://doi.org/10.1038/onc.2012.6
Gazzerro P, Proto MC, Gangemi G, Malfitano AM, Ciaglia E, Pisanti S, Santoro A, Laezza C, Bifulco M (2012) Pharmacological actions of statins: a critical appraisal in the management of cancer. Pharmacol Rev 64:102–146. https://doi.org/10.1124/pr.111.004994
Campbell MJ, Esserman LJ, Zhou Y, Shoemaker M, Lobo M, Borman E, Baehner F, Kumar AS, Adduci K, Marx C et al (2006) Breast cancer growth prevention by statins. Cancer Res 66:8707–8714. https://doi.org/10.1158/0008-5472.CAN-05-4061
Pocobelli G, Newcomb PA, Trentham-Dietz A, Titus-Ernstoff L, Hampton JM, Egan KM (2008) Statin use and risk of breast cancer. Cancer 112:27–33. https://doi.org/10.1002/cncr.23129
Boudreau DM, Gardner JS, Malone KE, Heckbert SR, Blough DK, Daling JR (2004) The association between 3-hydroxy-3-methylglutaryl conenzyme A inhibitor use and breast carcinoma risk among postmenopausal women: a case-control study. Cancer 100:2308–2316. https://doi.org/10.1002/cncr.20271
Baigent C, Keech A, Kearney PM, Blackwell L, Buck G, Pollicino C, Kirby A, Sourjina T, Peto R, Collins R et al (2005) Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet 366:1267–1278. https://doi.org/10.1016/S0140-6736(05)67394-1
Stone NJ, Robinson JG, Lichtenstein AH, Bairey Merz CN, Blum CB, Eckel RH, Goldberg AC, Gordon D, Levy D, Lloyd-Jones DM et al (2014) 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 129:S1-45. https://doi.org/10.1161/01.cir.0000437738.63853.7a
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94:496–509
Nielsen SF, Nordestgaard BG, Bojesen SE (2012) Statin use and reduced cancer-related mortality. N Engl J Med 367:1792–1802. https://doi.org/10.1056/NEJMoa1201735
Zhang X, Zhang D, Jia H, Feng Q, Wang D, Liang D, Wu X, Li J, Tang L, Li Y et al (2015) The oral and gut microbiomes are perturbed in rheumatoid arthritis and partly normalized after treatment. Nat Med 21:895–905. https://doi.org/10.1038/nm.3914
Yokomichi H, Nagai A, Hirata M, Tamakoshi A, Kiyohara Y, Kamatani Y, Muto K, Ninomiya T, Matsuda K, Kubo M et al (2017) Statin use and all-cause and cancer mortality: BioBank Japan cohort. J Epidemiol 27:S84–S91. https://doi.org/10.1016/j.je.2016.12.011
Islam MM, Yang HC, Nguyen PA, Poly TN, Huang CW, Kekade S, Khalfan AM, Debnath T, Li YJ, Abdul SS (2017) Exploring association between statin use and breast cancer risk: an updated meta-analysis. Arch Gynecol Obstet 296:1043–1053. https://doi.org/10.1007/s00404-017-4533-3
Wu QJ, Tu C, Li YY, Zhu J, Qian KQ, Li WJ, Wu L (2015) Statin use and breast cancer survival and risk: a systematic review and meta-analysis. Oncotarget 6:42988–43004. https://doi.org/10.18632/oncotarget.5557
Borgquist S, Broberg P, Tojjar J, Olsson H (2019) Statin use and breast cancer survival—a Swedish nationwide study. BMC Cancer 19:54. https://doi.org/10.1186/s12885-018-5263-z
Liu B, Yi Z, Guan X, Zeng YX, Ma F (2017) The relationship between statins and breast cancer prognosis varies by statin type and exposure time: a meta-analysis. Breast Cancer Res Treat 164:1–11. https://doi.org/10.1007/s10549-017-4246-0
Langballe R, Cronin-Fenton D, Dehlendorff C, Jensen MB, Ejlertsen B, Andersson M, Friis S, Mellemkjaer L (2018) Statin use and risk of contralateral breast cancer: a nationwide cohort study. Br J Cancer 119:1297–1305. https://doi.org/10.1038/s41416-018-0252-1
Hague WE, Simes J, Kirby A, Keech AC, White HD, Hunt D, Nestel PJ, Colquhoun DM, Pater H, Stewart RA et al (2016) Long-term effectiveness and safety of pravastatin in patients with coronary heart disease: sixteen years of follow-up of the LIPID study. Circulation 133:1851–1860. https://doi.org/10.1161/CIRCULATIONAHA.115.018580
Bonovas S, Sitaras NM (2007) Does pravastatin promote cancer in elderly patients? A meta-analysis. CMAJ 176:649–654. https://doi.org/10.1503/cmaj.060803
Righolt CH, Bisewski R, Mahmud SM (2019) Statin use and prostate cancer incidence in Manitoba, Canada: a population-based nested case-control study. Cancer Epidemiol Biomark Prev 28:1765–1768. https://doi.org/10.1158/1055-9965.EPI-19-0464
Hague WE, Simes J, Kirby A, Keech AC, White HD, Hunt D, Nestel PJ, Colquhoun DM, Pater H, Stewart RA, Sullivan DR, Thompson PL, West M, Glasziou PP, Tonkin AM, Ls investigatorsdagger (2016) Long-term effectiveness and safety of pravastatin in patients with coronary heart disease: sixteen years of follow-up of the LIPID study. Circulation 133:1851–1860. https://doi.org/10.1161/CIRCULATIONAHA.115.018580
Duncan RE, El-Sohemy A, Archer MC (2005) Statins and cancer development. Cancer Epidemiol Biomark Prev 14:1897–1898. https://doi.org/10.1158/1055-9965.EPI-05-0027
Desai P, Wallace R, Anderson ML, Howard BV, Ray RM, Wu C, Safford M, Martin LW, Rohan T, Manson JE et al (2018) An analysis of the association between statin use and risk of endometrial and ovarian cancers in the Women’s Health Initiative. Gynecol Oncol 148:540–546. https://doi.org/10.1016/j.ygyno.2018.01.006
Nimako GK, Wintrob ZA, Sulik DA, Donato JL, Ceacareanu AC (2017) Synergistic benefit of statin and metformin in gastrointestinal malignancies. J Pharm Pract 30:185–194. https://doi.org/10.1177/0897190015627255
El Sayed I, Helmy MW, El-Abhar HS (2018) Inhibition of SRC/FAK cue: a novel pathway for the synergistic effect of rosuvastatin on the anti-cancer effect of dasatinib in hepatocellular carcinoma. Life Sci 213:248–257. https://doi.org/10.1016/j.lfs.2018.10.002
Oh B, Kim TY, Min HJ, Kim M, Kang MS, Huh JY, Kim Y, Lee DS (2013) Synergistic killing effect of imatinib and simvastatin on imatinib-resistant chronic myelogenous leukemia cells. Anticancer Drugs 24:20–31. https://doi.org/10.1097/CAD.0b013e32835a0fbd
Chen CC, Hsu YP, Liu JC, Kao PF, Sung LC, Lin CF, Hao WR, Liu SH, Wu SY (2016) Statins dose-dependently exert significant chemopreventive effects against various cancers in chronic obstructive pulmonary disease patients: a population-based cohort study. J Cancer 7:1892–1900. https://doi.org/10.7150/jca.15779
Manthravadi S, Shrestha A, Madhusudhana S (2016) Impact of statin use on cancer recurrence and mortality in breast cancer: a systematic review and meta-analysis. Int J Cancer 139:1281–1288. https://doi.org/10.1002/ijc.30185
Anothaisintawee T, Udomsubpayakul U, McEvoy M, Lerdsitthichai P, Attia J, Thakkinstian A (2016) Effect of lipophilic and hydrophilic statins on breast cancer risk in Thai women: a cross-sectional study. J Cancer 7:1163–1168. https://doi.org/10.7150/jca.14941
Cheung KS, Chan EW, Wong AYS, Chen L, Seto WK, Wong ICK, Leung WK (2020) Statins were associated with a reduced gastric cancer risk in patients with eradicated helicobacter pylori infection: a territory-wide propensity score matched study. Cancer Epidemiol Biomark Prev 29:493–499. https://doi.org/10.1158/1055-9965.EPI-19-1044
Thomas T, Loke Y, Beales ILP (2018) Systematic review and meta-analysis: use of statins is associated with a reduced incidence of oesophageal adenocarcinoma. J Gastrointest Cancer 49:442–454. https://doi.org/10.1007/s12029-017-9983-0
Yi C, Song Z, Wan M, Chen Y, Cheng X (2017) Statins intake and risk of liver cancer: a dose-response meta analysis of prospective cohort studies. Medicine 96:e7435. https://doi.org/10.1097/MD.0000000000007435
Wang K, Gerke TA, Chen X, Prosperi M (2019) Association of statin use with risk of Gleason score-specific prostate cancer: a hospital-based cohort study. Cancer Med 8:7399–7407. https://doi.org/10.1002/cam4.2500
Kim YS, Park MS, Lee JH, Chung JW, Lee MJ, Kim CK, Jung JM, Oh K, Bang OY, Kim GM et al (2018) Effect of statins on survival following stroke in patients with cancer. Front Neurol 9:205. https://doi.org/10.3389/fneur.2018.00205
Branvall E, Ekberg S, Eloranta S, Wasterlid T, Birmann BM, Smedby KE (2020) Statin use is associated with improved survival in multiple myeloma: a Swedish population-based study of 4315 patients. Am J Hematol 95:652–661. https://doi.org/10.1002/ajh.25778
Suzuki R, Iwasaki M, Inoue M, Sasazuki S, Sawada N, Yamaji T, Shimazu T, Tsugane S, Japan Public Health Center-Based Prospective Study G (2010) Alcohol consumption-associated breast cancer incidence and potential effect modifiers: the Japan Public Health Center-based Prospective Study. Int J Cancer 127:685–695. https://doi.org/10.1002/ijc.25079
Giovannucci E, Harlan DM, Archer MC, Bergenstal RM, Gapstur SM, Habel LA, Pollak M, Regensteiner JG, Yee D (2010) Diabetes and cancer: a consensus report. Diabetes Care 33:1674–1685. https://doi.org/10.2337/dc10-0666
Garcia-Estevez L, Moreno-Bueno G (2019) Updating the role of obesity and cholesterol in breast cancer. Breast Cancer Res 21:35. https://doi.org/10.1186/s13058-019-1124-1
Zheng G, Hemminki A, Forsti A, Sundquist J, Sundquist K, Hemminki K (2019) Second primary cancer after female breast cancer: familial risks and cause of death. Cancer Med 8:400–407. https://doi.org/10.1002/cam4.1899
Clemons M, Goss P (2001) Estrogen and the risk of breast cancer. N Engl J Med 344:276–285. https://doi.org/10.1056/NEJM200101253440407
Warner M, Gustafsson JA (2014) On estrogen, cholesterol metabolism, and breast cancer. N Engl J Med 370:572–573. https://doi.org/10.1056/NEJMcibr1315176
Acknowledgements
The authors thank Dr. Yu-Fen Li for her help with the analysis of the NHIRD.
Funding
This research was funded by the China Medical University (CMU107-N-23), Taiwan Ministry of Health and Welfare Clinical Trial Center (MOHW109-TDU-B-212-114004), MOST Clinical Trial Consortium for Stroke (MOST 108-2321-B-039-003-), Ditmanson Medical Foundation Chia-Yi Christian Hospital (Grant No. R105-024), and Tseng-Lien Lin Foundation, Taichung, Taiwan.
Author information
Authors and Affiliations
Contributions
YCL, DWH, SHW, and YJP contributed to conceptualization, methodology, and investigation; PTC, CFT, MCL, and CCL contributed to software and formal analysis; SHW and YJP contributed to validation, supervision, project administration, and writing—review and editing; CFT, MCL, and CCL contributed to resources and data curation; PTC and CFT contributed to visualization; and YCL and DWH contributed to writing—original draft preparation. All the authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The studies are in accordance to the institutional guidelines for clinical research under IRB approved protocol (CMUH-104-REC2-115-R4) by the Research Ethics Committee of China Medical University for this retrospective study.
Informed consent
Informed consent of the subjects was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lu, YC., Huang, DW., Chen, PT. et al. Association between statin use and second cancer risk in breast cancer patients: a nationwide population-based cohort study. Breast Cancer Res Treat 185, 773–783 (2021). https://doi.org/10.1007/s10549-020-05969-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05969-9