Abstract
Background
Breast cancer survival outcomes vary across different ethnic groups. We clarified the differences in clinicopathological and survival characteristics of breast cancer among Japanese, US residents with Japanese origin (USJ), and US residents with other origins (USO).
Method
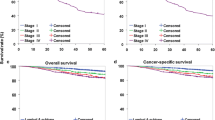
Using Surveillance, Epidemiology, and End Results (SEER) 18 dataset and Japanese Breast Cancer Society (JBCS) registry, we included patients first diagnosed with breast cancer between 2004 and 2015. We categorized the patients into three groups based on the database and the recorded ethnicity: Japanese (all those from the JBCS registry), USJ (those from SEER with ethnicity: Japanese), and USO (those from SEER with ethnicity other than Japanese). Excluding patients diagnosed after 2012, stage 0, and 4 patients, we examined the overall survival (OS) and breast cancer-specific survival (BCSS) using the Kaplan–Meier method and Cox proportional hazards models, adjusting for age, sex, cancer stage, and hormone receptor (HR) status.
Results
We identified 7362 USJ, 701,751 USO, and 503,013 Japanese breast cancer patients. The proportion of HR-positive breast cancer was the highest among USJ (71%). OS was significantly longer among Japanese and USJ than USO (Hazard ratio 0.46; 95% Confidence Interval [CI] 0.45–0.47 for Japanese and 0.66 [95% CI 0.59–0.74] for USJ) after adjusting for baseline covariates. BCSS was also significantly higher in the two groups (HR 0.53 [95% CI 0.51–0.55] for Japanese and 0.53 [95% CI 0.52–0.74] for USJ).
Conclusions
In stage I–III breast cancer, Japanese and US residents with Japanese origin experienced significantly longer survival than US residents with non-Japanese origins.





Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424. https://doi.org/10.3322/caac.21492
Waks AG, Winer EP (2019) Breast cancer treatment. JAMA 321(3):288. https://doi.org/10.1001/jama.2018.19323
Genentech (1998) Biotechnology Breakthrough In Breast Cancer Wins FDA Approval, Press Releases|Friday, Sep 25, 1998. https://www.gene.com/media/press-releases/4763/1998–09–25/biotechnology-breakthrough-in-breast-can. Accessed September 25, 2019.
Yeo W, Ueno T, Lin C-H et al (2019) Treating HR+/HER− breast cancer in premenopausal Asian women: Asian Breast Cancer Cooperative Group 2019 Consensus and position on ovarian suppression. Breast Cancer Res Treat. https://doi.org/10.1007/s10549-019-05318-5
Costa RLB, Gradishar WJ (2017) Differences are important: breast cancer therapy in different ethnic groups. J Glob Oncol 3(4):281–284. https://doi.org/10.1200/jgo.2017.009936
Wakai K, Suzuki S, Ohno Y, Kawamura T, Tamakoshi A, Aoki R (1995) Epidemiology of breast cancer in Japan. Int J Epidemiol. 24(2):285–291
Howlader N, Noone A, Krapcho M, et al. (2017) SEER Cancer Statistics Review, 1975–2014. April. https://seer.cancer.gov/csr/1975_2014/, based on November 2016 SEER data submission, posted to the SEER web site, April 2017, Published 2017.
DeSantis CE, Bray F, Ferlay J, Lortet-Tieulent J, Anderson BO, Jemal A (2015) International variation in female breast cancer incidence and mortality rates. Cancer Epidemiol Biomarkers Prev 24(10):1495–1506. https://doi.org/10.1158/1055-9965.epi-15-0535
Zhang J, Dhakal IB, Zhao Z, Li L (2012) Trends in mortality from cancers of the breast, colon, prostate, esophagus, and stomach in East Asia: role of nutrition transition. Eur J Cancer Prev 21(5):480–489. https://doi.org/10.1097/CEJ.0b013e328351c732
Matsuno RK, Anderson WF, Yamamoto S et al (2007) Early- and late-onset breast cancer types among women in the United States and Japan. Cancer Epidemiol Biomarkers Prev 16(7):1437–1442. https://doi.org/10.1158/1055-9965.EPI-07-0108
National Cancer Institute Nationa Cancer Institute DCCPS Surveillancel Research Program (2017) Female breast cancer—cancer stat facts. Surveillance, epidemiology, and end results (SEER) program populations (1969–2016). https://seer.cancer.gov/statfacts/html/breast.html. Published 2017. Accessed June 17, 2019.
Iwamoto T, Fukui N, Kinoshita T et al (2015) Comprehensive prognostic report of the Japanese Breast Cancer Society registry in 2006. Breast Cancer. https://doi.org/10.1007/s12282-015-0646-3
Curtis E, Quale C, Haggstrom D, Smith-Bindman R (2008) Racial and ethnic differences in breast cancer survival: How much is explained by screening, tumor severity, biology, treatment, comorbidities, and demographics? Cancer 112(1):171–180. https://doi.org/10.1002/cncr.23131
Pineda MD, White E, Kristal AR, Taylor V (2001) Asian breast cancer survival in the US: a comparison between Asian immigrants, US-born Asian Americans and Caucasians. Int J Epidemiol 30(5):976–982. https://doi.org/10.1093/ije/30.5.976
Lin SS, Clarke CA, Prehn AW, Glaser SL, West DW, O’Malley CD (2002) Survival differences among Asian subpopulations in the United States after prostate, colorectal, breast, and cervical carcinomas. Cancer 94(4):1175–1182. https://doi.org/10.1002/cncr.10319
National Cancer Institute DCCPS Surveilane Research Program The Surveillance Research Program of the Division of Cancer Control and Population Science (2017) SEER*Stat Database: Incidence - SEER 18 Regs Research Data + Hurricane Katrina Impacted Louisiana Cases, Nov 2017 Sub (2000–2015) <Katrina/Rita Population Adjustment>.
Tokuda Y, Kumamaru H, Jinno H (2019) The japanese breast cancer society breast cancer registry in the national clinical database: current status and future perspectives to improve outcomes for breast cancer patients. Jpn Surg Soc. 120(6):639–645
Greene FL, Page DL, Fleming ID, et al. (2002) AJCC cancer staging manual. 6th ed. (the American Joint Committee on Cancer, ed.). Springer-Verlag, New York
Cianfrocca M, Goldstein LJ (2004) Prognostic and predictive factors in early-stage breast cancer. Oncologist 9(6):606–616. https://doi.org/10.1634/theoncologist.9-6-606
Uchida K, Ohashi H, Kinoshita S et al (2015) Breast cancer screening and the changing population pyramid of Japan. Breast Cancer 22(2):172–176. https://doi.org/10.1007/s12282-013-0470-6
World Bank (2016) World Bank: population ages 65 and above (% of total). https://data.worldbank.org/indicator/SP.POP.65UP.TO.ZS. Published 2016. Accessed July 23, 2019.
Kurebayashi J, Moriya T, Ishida T et al (2007) The prevalence of intrinsic subtypes and prognosis in breast cancer patients of different races. Breast 16(2 SUPPL.):72–77. https://doi.org/10.1016/j.breast.2007.07.017
Kamineni A, Anderson ML, White E et al (2013) Body mass index, tumor characteristics, and prognosis following diagnosis of early stage breast cancer in a mammographically-screened population. Cancer Causes Control 24(2):305–312. https://doi.org/10.1007/s10552-012-0115-7
Kwan ML, John EM, Caan BJ et al (2014) Obesity and mortality after breast cancer by Race/Ethnicity: The california breast cancer survivorship consortium. Am J Epidemiol 179(1):95–111. https://doi.org/10.1093/aje/kwt233
Ziegler RG, Hoover RN, Pike MC et al (1993) Migration patterns and breast cancer risk in Asian–American women. J Natl Cancer Inst 85(22):1819–1827. https://doi.org/10.1093/jnci/85.22.1819
Pike MC, Kolonel LN, Henderson BE et al (2002) Breast cancer in a multiethnic cohort in Hawaii and Los Angeles: risk factor-adjusted incidence in Japanese equals and in Hawaiians exceeds that in whites. Cancer Epidemiol Biomarkers Prev. 11(9):795–800
Maeda H, Kurokawa T (2015) Recent trends for drug lag in clinical development of oncology drugs in Japan: does the oncology drug lag still exist in Japan? Int J Clin Oncol 20(6):1072–1080. https://doi.org/10.1007/s10147-015-0825-4
DPE Research Department (2019) The U.S. Health care system. https://international.commonwealthfund.org/countries/united_states/.
Chambers JD, May KE, Neumann PJ (2013) Medicare covers the majority of FDA-approved devices and part B drugs, but restrictions and discrepancies remain. Health Aff 32(6):1109–1115. https://doi.org/10.1377/hlthaff.2012.1073
Shaw DL, Dhruva SS, Ross JS (2018) Coverage of novel therapeutic agents by medicare prescription drug plans following FDA approval. J Manag Care Spec Pharm 24(12):1230–1238. https://doi.org/10.18553/jmcp.2018.24.12.1230
Hsu CD, Wang X, Habif DV, Ma CX, Johnson KJ (2017) Breast cancer stage variation and survival in association with insurance status and sociodemographic factors in US women 18 to 64 years old. Cancer 123(16):3125–3131. https://doi.org/10.1002/cncr.30722
Sakamoto H, Rahman M, Nomura S, et al. (2018) Japan health system review. Vol. 8 No. 1. World Health Organization, Regional Office for South-East Asia. https://apps.who.int/iris/. Accessed June 21, 2019.
Iqbal J, Ginsburg O, Rochon PA, Sun P, Narod SA (2015) Differences in breast cancer stage at diagnosis and cancer-specific survival by race and ethnicity in the United States. JAMA 313(2):165–173. https://doi.org/10.1001/jama.2014.17322
Rae M (2019) Tax Subsidies for Private Health Insurance – II. Non-Group Coverage – 7779–02 | The Henry J. Kaiser Family Foundation. https://www.kff.org/report-section/tax-subsidies-for-private-health-insurance-ii-non-group-coverage/. Accessed May 17, 2019.
Ebell MH, Thai TN, Royalty KJ (2018) Cancer screening recommendations: an international comparison of high income countries. Public Health Rev. https://doi.org/10.1186/s40985-018-0080-0
American Cancer Society (2019) Cancer prevention & early detection facts & figures, 2019–2020
Cancer Information Service (2019) Cancer registry and statistics, National Cancer Center, Japan
Wilson RJ, Zhang K (2014) Coding completeness and quality of relative survival-related variables in the national program of cancer registries cancer surveillance system, 1995–2008. J Registry Manag. 41(2):65–71
Process—SEER Quality Improvement (2019s) https://seer.cancer.gov/qi/process.html. Accessed August 7, 2019.
Tomotaki A, Miyata H, Hashimoto H, Murakami A, Ono M (2014) Results of data verification of the Japan congenital cardiovascular database, 2008 to 2009. World J Pediatr Congenit Heart Surg 5(1):47–53. https://doi.org/10.1177/2150135113508794
Howlader N, Noone AM, Krapcho M, Miller D, Brest A, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ CK (eds) (2019) SEER Cancer Statistics Review, 1975–2014, National Cancer Institute. Bethesda, MD, https://seer.cancer.gov/csr/1975_2014/, based on November 2016 SEER data submission, posted to the SEER web site, April 2017
Acknowledgements
We would like to thank the patients and institutions involved in the Breast Cancer Registry of the JBCS for their efforts to register patients’ data. We would also like to thank Nancy L. Keating for statistical advice and Editage (www.editage.jp) for English language editing.
Funding
This work was supported by the research fund from the Japanese Breast Cancer Society (JBCS) (Grant Number: 17003).
Author information
Authors and Affiliations
Contributions
RO, TO, and NN, contributed to the concept and design of the study. RO, HK, YT, YS, and NN contributed to the analysis and interpretation of data, and the drafting of the article. All authors contributed to the revision, approved the final version to be published, and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of interests
Dr. Ogiya, Dr. Aogi, Dr. Kinoshita, Dr. Iwamoto, Dr. Jinno, Dr. Kawai, Dr. Okamura, Dr. Takeuchi, Dr. Yoshida, Dr. Imoto, Dr. Masuoka, Dr. Sagara, and Dr. Kojima have nothing to disclose. Dr. Niikura reports grants from Novartis, Bristol-Myers Squibb, Chugai Pharmaceutical Co, Nihon Medi-Physics Co. Ltd., Merc Sharp & Dohme, Daiichi-Sankyo (RF-to Tokai University), and personal fees from AstraZeneca, Novartis, Eisai, and Pfizer; Dr. Ishida reports grants from Taiho Pharmaceutical Co., Ltd, Eisai, Kyowa-Kirin, Chugai Pharmaceutical co., Ltd., personal fees from Chugai Pharmaceutical co., Ltd., Pfizer Japan Inc., and Eisai Co., Ltd. Dr. Hayashi reports personal fees from Chugai-pharma, Novartis, AstraZeneca, Pfizer, Kirin Pharma, Genomic Health Inc., Devicor Japan, and Allergan Japan. Dr. Anan reports personal fees from Pfizer, Chugai Pharmaceutical, AstraZeneca, Eisai, Novartis Pharma, and Eli Lilly. Dr. Tsuda reports grants from Taiho Pharmaceutical Co. and Chugai Pharmaceutical Co., grants and personal fees from Roche Diagnostics Co., and personal fees from Konica Minolta Co., Eisai Co., AstraZeneca, and Bristol-Myers Squibb. Dr. Miyata and Dr. Kumamaru report being affiliated with the department of healthcare quality assessment at the University of Tokyo. The department is a social collaboration department supported by the National Clinical Database, Johnson & Johnson K.K., and Nipro Corporation.
Ethical approval
This article does not contain any studies involving human participants performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ogiya, R., Niikura, N., Kumamaru, H. et al. Breast cancer survival among Japanese individuals and US residents of Japanese and other origins: a comparative registry-based study. Breast Cancer Res Treat 184, 585–596 (2020). https://doi.org/10.1007/s10549-020-05869-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10549-020-05869-y